INTRODUCTION
Over the past few decades, there has been notable progress in the field of minimally invasive spine surgery (MISS). MISS is known to offer several advantages, including reduced postoperative pain, faster recovery and reduced surgical site infection (SSI) due to minimal incisions and tissue manipulation [1]. Based on these advantages, MISS has become a highly preferred surgical approach for treating various spinal conditions, including degenerative, traumatic, and deformity cases [2]. However, despite its many advantages, SSI remains a significant concern for spine surgeons who prefer MISS [3]. In this article, we aim to share a unique case experience involving the revision of a patient who developed a delayed surgical site fungal infection following anterior lateral interbody fusion (ALIF). The revision procedure involved oblique lateral interbody fusion (OLIF) using an allo-bone graft.
CASE REPORT
1. Case Presentation
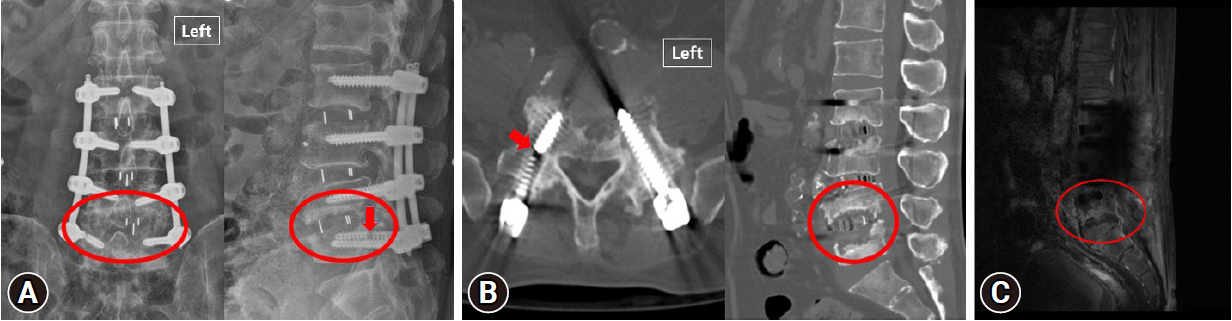
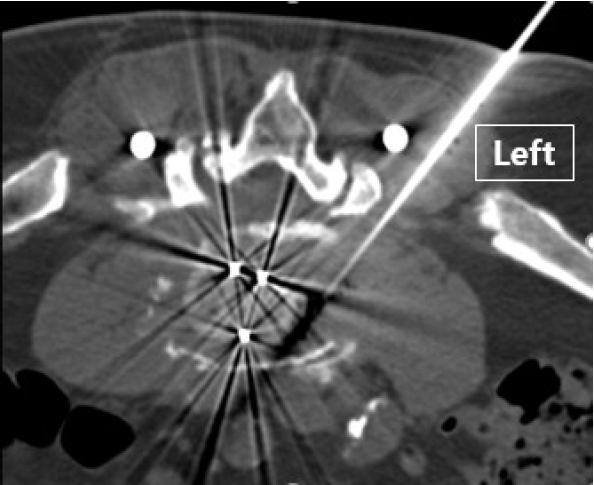
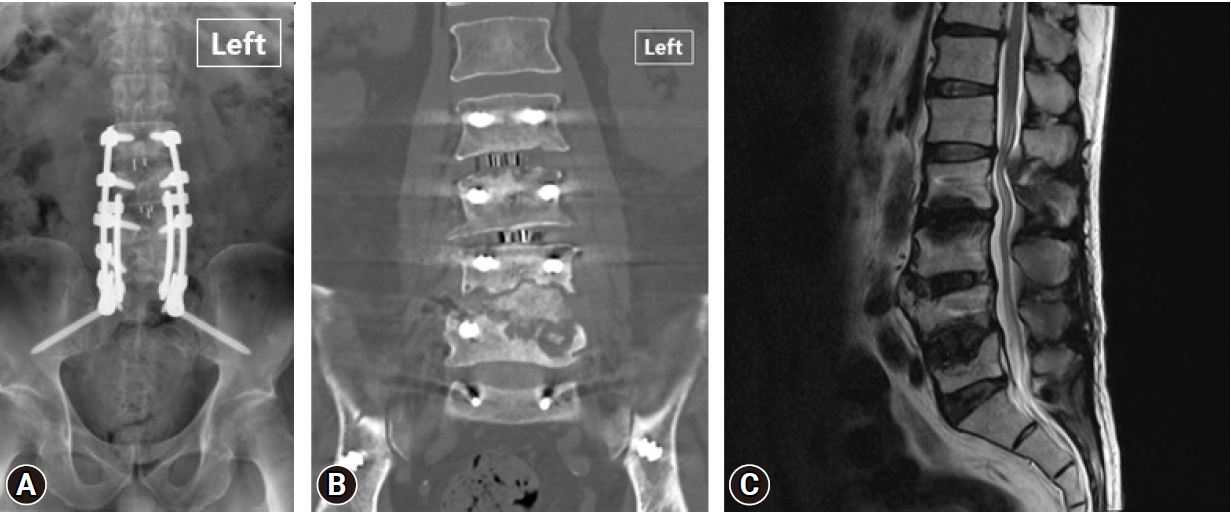
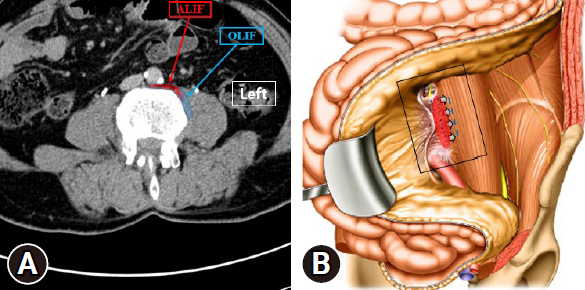
A 73-year-old male patient with a medical history of rheumatoid arthritis diagnosed in 2017 has been taking leflunomide, methotrexate, and hydroxychloroquine. He underwent ALIF surgery from L2 to L5 at a Gwangju Wooridul Hospital in April 2021. The purpose of the surgery was to address lumbar spondylolisthesis and spinal stenosis, which were causing low back pain. Immediately after the operation, there were no signs of neurological deficit, and the patient experienced some improvement in low back pain. However, after approximately 6 months, the pain recurred and worsened, ultimately rendering the patient unable to walk due to severe low back pain. Initial treatment involved conservative measures to manage the symptoms, but no significant improvement was observed. Accordingly, radiological examinations, including x-ray and computed tomography (CT), were conducted. These tests confirmed a fracture of the right L5 screw and revealed the presence of pseudoarthrosis with osteolysis at the L4L/5 (Figure 1A, B). SSI was suspected, prompting the performance of contrast-enhanced magnetic resonance imaging, which identified a contrast-enhancing lesion at L5 (Figure 1C). Peripheral blood tests showed white blood cell count of 13,450/mm3 (neutrophils 78.3%, lymphocytes 12.0%, monocytes 0.96%), erythrocyte sedimentation rate (ESR) of 37 mm/hr, and C-reactive protein (CRP) of 2.20 mg/dL. To isolate the pathogen, a CT-guided biopsy was conducted (Figure 2), and the culture test the presence of Aspergillus fumigatus.
2. Revision Procedure
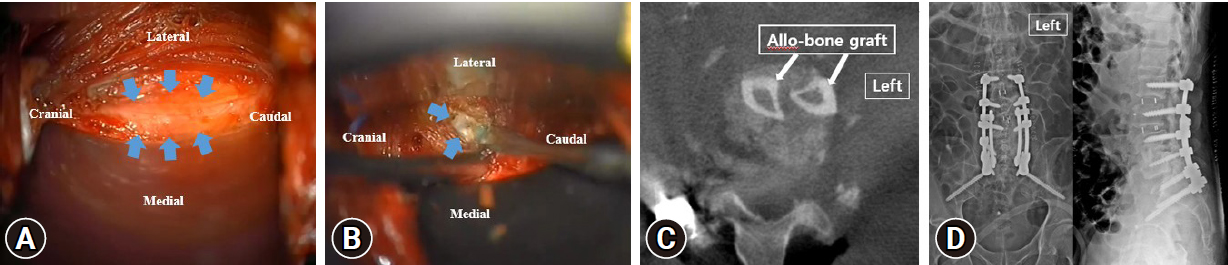
The planned approach for the revision surgery at the site of the lesion was OLIF. Following the conventional method [4], the patient was positioned in the right lateral decubitus position, and a layer-by-layer dissection of the abdominal muscles was performed to access the retroperitoneal space. Although there were tissue adhesions resulting from the previous surgery, they were not severe. Therefore, caution was exercised during the approach to the disk space. The psoas muscle was laterally dissected to expose the disk space through the corridor where the discectomy was previously performed during ALIF (Figure 3A). During annulotomy, fluid resembling an abscess was observed, and a specimen was collected for culture testing. To ensure an adequate window, annulotomy was further performed using a Kerrison punch and pituitary rongeur forceps, followed by the removal of the previously inserted cage (Figure 3B). Then, a fibular strut was cut to match the dimensions of the disk space and inserted to provide support within the empty interbody space. An intraoperative O-arm scan confirmed the stable positioning of the graft (Figure 3C).
After allo-bone graft insertion, the patient was changed to the prone position and the screws (65 mm × 4.5 mm) and rods previously placed in L2, 3, 4, and 5 were removed and larger diameter screws (70 mm × 5 mm) were inserted in the same path. Additional screws were inserted in S1 and S2 alar and a cross-link was used for extra stability (Figure 3D).
3. Postoperative Course
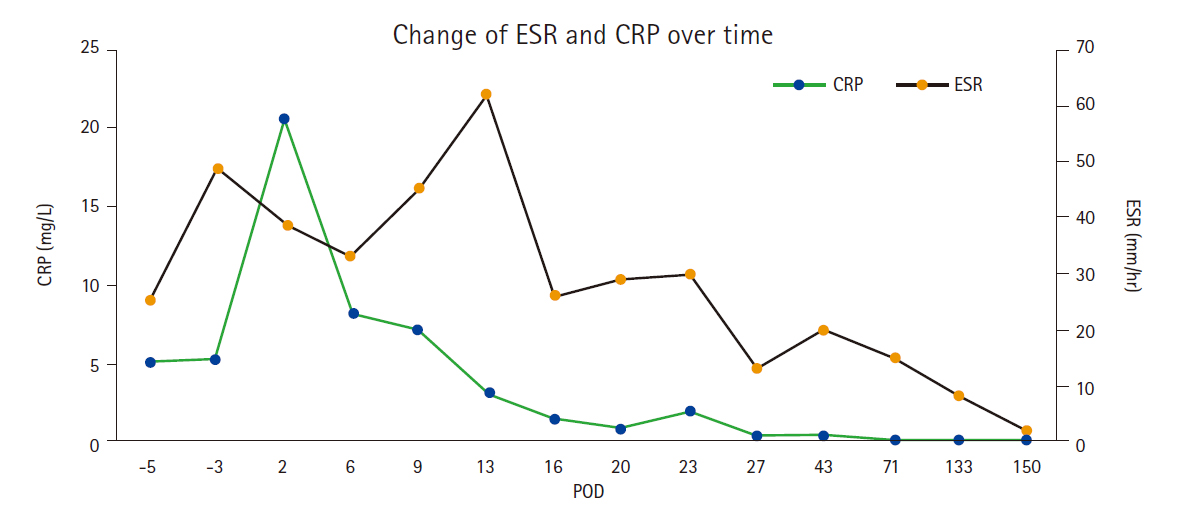
Following the surgery, the patient experienced a significant improvement in pain, and by the seventh day after the surgery, the patient was able to ambulate with the assistance of a walker. A. fumigatus was confirmed through culture tests conducted on the specimens obtained intraoperatively. The patient received intravenous as an antifungal treatment for 3 weeks, which was later switched to an oral agent. With antifungal agent, CRP exhibited a significant decrease, stabilizing below 0.5 (Figure 4). Subsequently, the patient was discharged. During outpatient follow-up at 6 months postsurgery, the patient demonstrated independent ambulation while wearing only a thoracolumbosacral orthosis brace. Peripheral blood tests showed normal CRP and ESR. Radiological examinations indicated well-maintained structural integrity (Figure 5), and there were no indications of infection recurrence.
DISCUSSION
MISS is widely recognized for its significantly low incidence of SSI. According to published literature, MISS has demonstrated a reduction in postoperative SSI by up to 10 times when compared to open spine surgery [5-7]. Staphylococcus aureus is commonly identified as the leading pathogen causing infections after spinal surgery [8]. Notably, cases of fungal spondylitis following MISS, as seen in our case, are extremely rare [9,10]. Previous literature reported that fungal infections can occur in the bloodstream through intravenous lines, prosthetic device implantation, or surgical procedures [11]. Fungal spondylitis tends to occur primarily in immunocompromised patients with conditions such as diabetes mellitus, undergoing chemotherapy, using chronic corticosteroids or experiencing malnutrition [10,12,13]. Given that the patient in our case had a history of continuous use of immunosuppressive agents for rheumatoid arthritis; it is presumed that the delayed fungal spondylitis occurred as a result. Therefore, it is crucial to recognize that if a delayed infection is suspected postsurgery, particularly in patients with a history of immunosuppressive agent usage, fungal infection should be considered as a possibility.
In our case, Aspergillus was consistently identified in both preoperative and intraoperative specimens. Spondylitis, an infection of the vertebral body, is typically caused by bacteria, but fungal infections are rare. The most common fungi causing infections are Candida, with Aspergillus being a less common pathogen [10,14].
Aspergillus can affect different parts of the body, including the lungs and sinuses. However, it can also rarely cause spondylitis [12,13,15]. Aspergillus spondylitis is a serious condition that requires immediate medical attention. Voriconazole, available in oral and intravenous forms, is considered the primary treatment for invasive aspergillosis [16]. Numerous reports have shown its effectiveness in clinical outcomes [17,18], which was also demonstrated in this case. However, careful monitoring is necessary due to its potential side effects of liver toxicity and renal dysfunction, as it maintains therapeutic concentrations in the bloodstream [19].
Allo-bone graft was chosen because it has proven to be a highly effective treatment option for spondylitis [20], and in this case, OLIF was considered as the most optimal procedure. The posterior approach was deemed unsuitable as it would not allow the insertion of larger supporting structures. Since the patient had an enlarged L4/5 interbody space caused by osteolysis, fusion using posterior approach was considered less suitable. Previous studies have shown higher complication rates when the anterior approach is used for revision surgery in patients who had initially undergone ALIF [21]. Similarly, performing revision OLIF after ALIF, as in this case, can pose a significant challenge for spine surgeons. However, by gaining a deeper understanding of the differences between ALIF and OLIF procedures, OLIF can be considered as an effective revision procedure. Since the ALIF corridor dissects only a portion of the medial boarder of the psoas muscle, the lateral part beyond the medial boarder is presumed to have fewer adhesions. Therefore, it is considered relatively safe to perform the OLIF by dissecting in this area (Figure 6).
CONCLUSION
In this case, we encountered a unique situation of delayed fungal spondylitis following ALIF in a patient with a history of immunosuppressive agent usage. Although fungal spondylitis is highly uncommon after MISS, it should be considered in the differential diagnosis when there are associated risk factors. Specifically, if the causative agent is Aspergillus, voriconazole could be a suitable choice for antifungal treatment. Moreover, as a revision method after ALIF, OLIF demonstrated effectiveness in this case.