Use of Minimally Invasive Spine Surgery in the Management of High-grade Thoracolumbar Spine Injuries
Article information
Abstract
Objective
Spinal fractures often have devastating sequelae. Thoracolumbar fractures are classified using the Thoracolumbar Injury Classification and Severity score (TLICS) to determine the severity of injury and to guide treatment. Recently advancements in minimally invasive spine surgery (MISS) have led to new approaches to high-severity fractures. Studies have suggested that MISS may yield similar outcomes to conventional, more invasive procedures while producing several benefits.
Methods
This retrospective study involves 46 patients treated from 2005 through 2020 for high grade thoracolumbar trauma from T2 to L5 with a minimum follow-up of 6-months treated with MISS techniques using percutaneous instrumentation.
Results
Average TLICS was 7.5. Patient derived outcome measures with average length of follow-up of 602 days included Oswestry Disability Index 28.9, Patient Satisfaction Index 4.2, Short Form-12 Mental Component Score 51.9, and Short Form-12 Physical Component Score 37.7. Average estimated blood loss was 119.2 mL.
Conclusion
The TLICS is a validated tool used to guide surgical intervention in high grade trauma. The utilization of MISS techniques for the treatment and stabilization of thoracolumbar trauma is efficacious and a viable alternative to traditional open approaches.
INTRODUCTION
Spinal fractures can result in damage to the adjacent spinal cord or neural structures, reduce quality of life, cause chronic pain, and confer an approximate mortality rate twice that of matched controls [1]. Traumatic spinal injuries most commonly affect the thoracolumbar junction (T10-L2). This region endures a great amount of biomechanical stress, serving as the transition point from the more rigid thoracic spine (and its rib attachments) to the more flexible lumbar spine, making it particularly vulnerable [2].
Traumatic thoracolumbar fractures are characterized into compression, burst, flexion-distraction, extension-distraction, and translation injuries. Compression and burst fractures are generally less severe and associated with lower risk of spinal instability. The mechanism of injury for both compression and burst fractures is excessive axial force that causes vertebral collapse, such as from motor vehicle accidents or a fall from height. Compression fractures affect only the anterior column while burst fractures affect both the anterior and middle columns [2].
While ligamentous disruption may occur in unstable burst fractures, this is more often seen in translation/rotational, flexion-distraction, and extension-distraction fractures. In translation/rotational fractures, injury results from vertebral displacement in the horizontal plane or from rotation. Flexion-distraction fractures happen due to hyperflexion in which the anterior and middle columns collapse from compression, and the posterior column is separated into two fragments from excessive tension (Figure 1). This mechanism of injury commonly involves a patient wearing only a lap belt during a motor vehicle accident; the collision causes sudden deceleration and hyperflexion against the lap belt. Extension-distraction fractures are less common and happen due to hyperextension. The anterior spine is separated into two pieces from excessive tension, while the posterior spine collapses from compression [2].
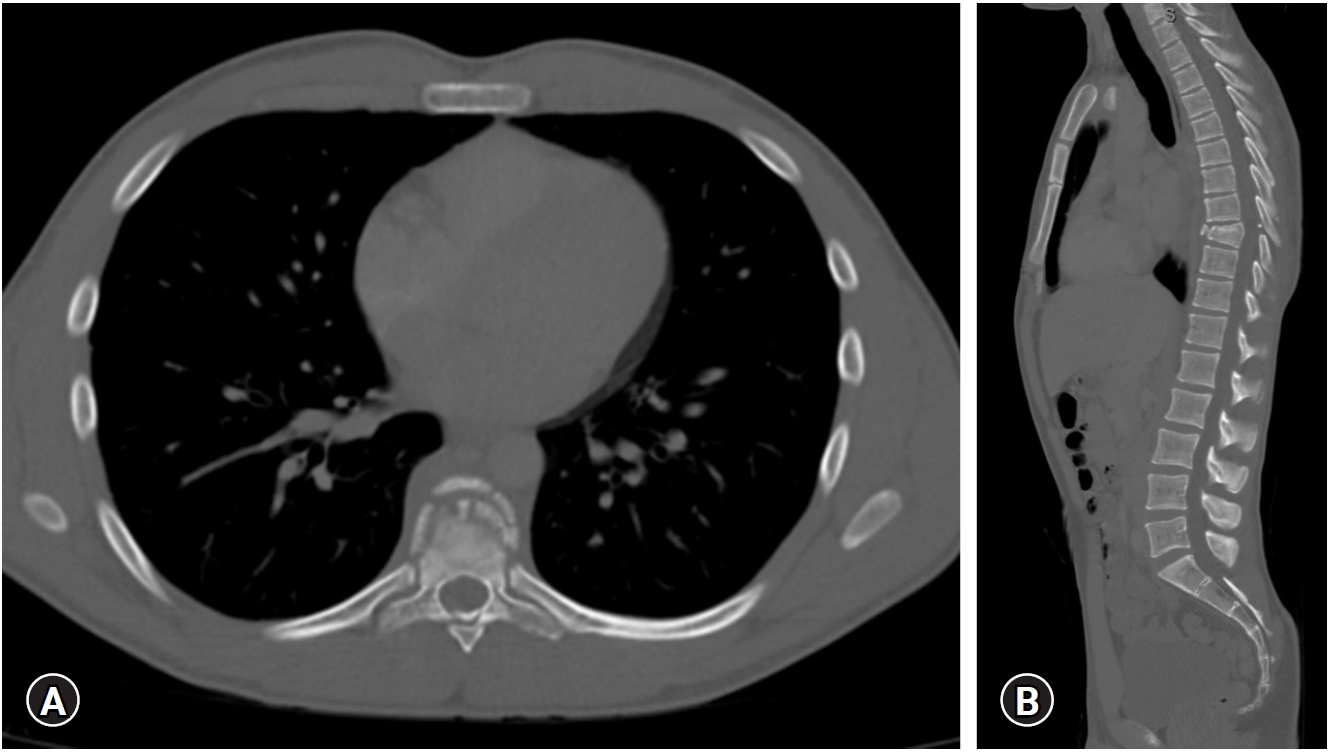
CT images in the (A) coronal and (B) sagittal planes of a thoracic flexion-distraction injury resulting in disruption of posterior column and spinal cord injury.
Thoracolumbar fractures are classified using the thoracolumbar injury classification and severity (TLICS) scale to determine the severity of injury and help guide treatment. It is classified based on three major categories of (1) injury morphology, (2) posterior ligamentous complex (PLC) integrity, and (3) the patient’s neurologic status. Points are assigned for each of the three categories and a higher total score indicates a more severe injury [3]. In terms of using the TLICS score to guide treatment, a total score of 0 to 3 suggests success with non-operative management, while a score of 5 or greater warrants operative treatment. A score of 4 falls into an area of ambiguity in which either non-operative or operative treatment may be appropriate [3]. Non-operative treatment includes mobilization with or without supportive braces and casts. Operative procedures include posterior pedicle screw fixation, decompression, and/or fusion, depending on the clinical scenario [2]. In addition, The American Spinal Injury Association (ASIA) impairment scale is often used to evaluate spinal cord injuries and to determine whether they are complete or incomplete. It considers sensory function, motor function with strength testing, reflexes, and level of neurologic injury [4,5].
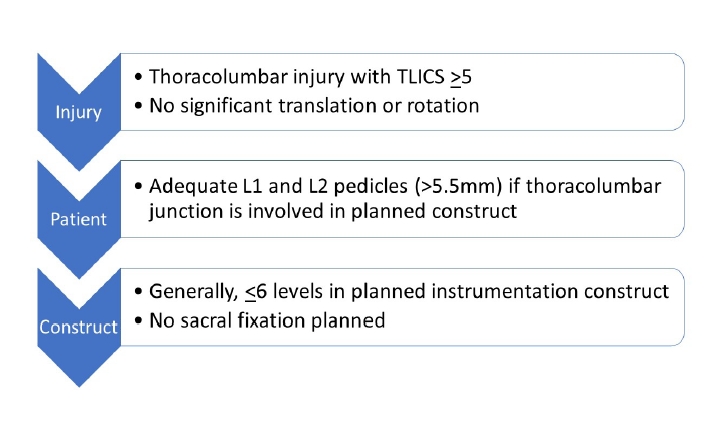
Recently, there have been advancements in minimally invasive spine surgery (MISS). Studies have suggested that MISS may yield similar outcomes to conventional, more invasive procedures while producing several benefits. Two randomized controlled trials conducted by Dai et al. [6] and Jindal et al. [7] took steps towards a less invasive approach for posterior pedicle screw fixation by forgoing fusion. Their results indicated that posterior pedicle screw fixation without fusion provided benefits of significantly decreased operative time and blood loss without compromising kyphosis angle correction for burst fractures [6,7]. Furthermore, a prospective, randomized trial by Jiang et al. [8] showed that MISS with percutaneous pedicle stabilization for burst fractures produced no differences in long-term clinical outcomes compared to open paraspinal pedicle stabilization. However, it is important to note that these studies included only low grade fracture cases in which all the patients had burst fractures with load-sharing scores of 6 [6,7], or in which none of the patients had neurologic deficits [8]. Our study investigates the effects of MISS percutaneous approaches for high grade injuries with TLICS scores of 4 or greater.
MATERIALS AND METHODS
The present retrospective case review was approved by the Institutional Review Board (IRB) at our institution (approval #5231). Informed consent was not obtained nor required given the de-identified, retrospective nature of this study. This study involves 46 patients treated by the senior surgeon from 2005 through 2020 for high grade thoracolumbar trauma from T2 to L5 with a minimum follow-up of six month.
Our departmental billing database was used to identify all patients who had undergone posterior MISS for management of acute thoracic, thoracolumbar, or lumbar fractures. Medical records and imaging studies were used to identify cases with the following inclusion criteria: acute traumatic spine injuries; TLICS>4; surgical management with a dorsal minimally invasive surgical technique using percutaneous approaches for all aspects of the procedure including placement of spinal instrumentation, deformity reduction, decompression and/or repair of cerebrospinal fluid leak; and a minimum follow-up period of 6-month.
Medical records were used to identify patient’s age, sex, height, weight, body mass index, race, tobacco use, insurance status, and mode of injury.
Pre-operative neurologic status was obtained from the medical records and classified as intact, nerve root injury, cauda equina injury, partial spinal cord injury or complete spinal cord injury. Patients with spinal cord injury were further classified by the ASIA score. Pre-operative imaging studies were used to classify the injury using TLICS. As described, a score of >4 constitutes a high-grade injury suggesting surgical intervention may be indicated. The current study specifically excludes stable burst fractures (TLICS<4). Accordingly, the few patients included with burst fractures had an accompanying neurologic deficit.
Medical records were used to determine the surgical techniques used in terms of decompression, arthrodesis, screw placement, vertebral augmentation, bone graft type and/or repair of cerebrospinal fluid leak.
Patient-derived outcome measures obtained during routine clinical follow-up include the Oswestry Disability Index (ODI), visual analogue scale (VAS) for back and leg pain, SF-12 Physical Component Score (SF-12 PCS), SF-12 Mental Component Score (SF-12 MCS), and a five level patient satisfaction score.
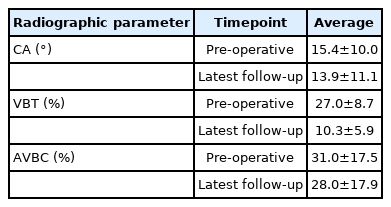
Using the measurements presented by the spine trauma group, pre-operative and final follow-up Cobb angle, vertebral body translation percentage, and anterior vertebral body compression percentage were measured and analyzed for the study population [9]. The Cobb angle was measured between the superior end plate one segments above the injured level to the inferior end plate one segment below the injured level. The vertebral body translation percentage defines the percentage of translation or sheer between the posterior endplates of adjacent segments. The anterior vertebral body compression percentage calculates the amount of wedge deformity in relation in adjacent vertebral bodies above and below the fractured segment.
RESULTS
Baseline patient characteristics are shown in Table 1. This cohort includes 71.1% men and 28.9% women with a mean age of 44.3±21.0 years. The most common modes of injury include motor vehicle collisions, accidental falls, and motor sports injuries. Trauma at the thoracic vertebrae and thoracolumbar junction each accounted for 37.8% of the cases, while trauma at the lumbar vertebrae accounted for the remaining 24.4%.
Average TLICS score was 7.5±1.6. Most injuries were distraction injuries, which comprised 71.1% of cases, and the PLC was injured in 73.9%. With regards to neurological compromise, 19.6%, 4.3%, and 13.0% of cases were classified as ASIA A, B, and C respectively. Overall, neurologic injury was seen in 56.5% of the cases. On the AO classification scale, the majority of cases were B2 (47.8%) and B3 (28.3%). 10.9% of cases were subtype C (Table 2).
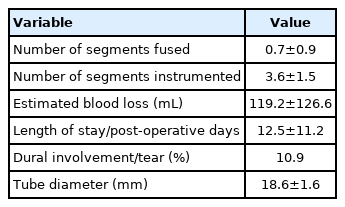
Average estimated blood loss was 119.2±126.6 mL, and average length of stay was 12.5±11.2 days. Dural involvement/tear occurred in 10.9% of cases. The average number of segments fused and instrumented were 0.7±0.9 and 3.6±1.5, respectively. The average diameter of the tube used for the MISS procedures was 18.6±1.6 mm (Table 3).
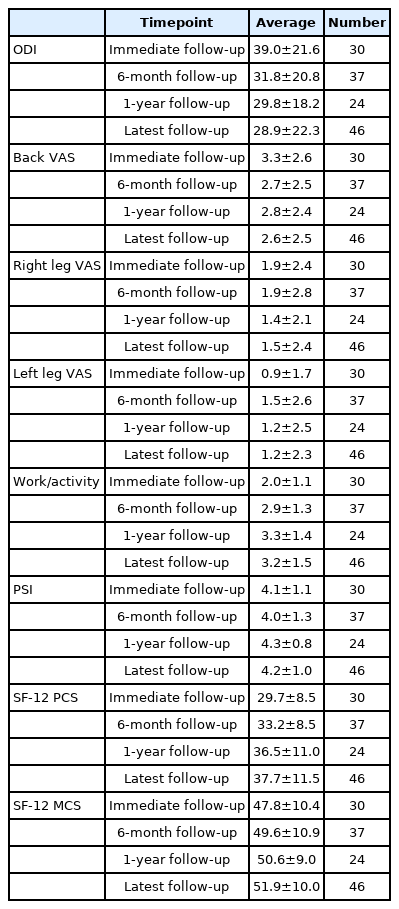
Patient-derived outcomes are shown in Table 4. ODI of the lower back decreased for each of the time points, suggesting decreased levels of disability as time progressed. SF-12 PCS and MCS scores increased for each of the time points and demonstrate improved physical health and mental well-being, respectively. There were also overall decreases in VAS scores indicating pain reduction in the back and lower extremities, as well as increases in work and activity levels. In addition, PSI scores were greater than 4.0 on a scale of 1 to 5 and demonstrated high patient satisfaction with the procedure.
Radiographic data are shown in Table 5. Cobb angle, vertebral body translation percentage, and anterior vertebral body compression percentage were all decreased at latest follow-up compared to pre-operative baselines.
DISCUSSION
In this study, we retrospectively investigated the effects of MISS for high-grade thoracolumbar trauma on patient outcomes. Our patients had an average TLICS score of 7.5±1.6 with an average age of 44.4±20.8 years. Most of our patients were men, and motor vehicle collisions and accidental falls made up 78.3% of cases. Our patient population was therefore similar to that of Wang et al.’s [10] epidemiological study on traumatic spinal fractures.
Average intraoperative blood loss was approximately 120 mL, and average length of stay was less than 2 weeks. Radiographic analysis demonstrated an improvement in translation percentage following MISS reduction and fixation as well as radiographic improvement in both Cobb angles and vertebral body compression percentage without evidence of progressive kyphosis or deformity. A majority of patients underwent unilateral percutaneous instrumentation further minimizing blood loss and surgical time (Figure 2). Individuals requiring long constructs, sacral fixation due to inherent bone quality of the sacrum, those with complete loss of ligamentous integrity in translation injuries underwent bilateral instrumentation (Figure 3). In addition, disability and pain decreased, while activity level, physical health, and mental well-being increased (at the latest follow-up, the average ODI score was 28.9%± 22.3% and the VAS score for back pain was 2.6±2.5). Average SF-12 PCS and MCS scores were 37.7 and 51.9, respectively, at latest follow-up; both SF-12 PCS and MCS scores are approximately 50 for the general population. Therefore, our data indicate that our patients had lower physical capacity but similar mental capacity relative to the general population.
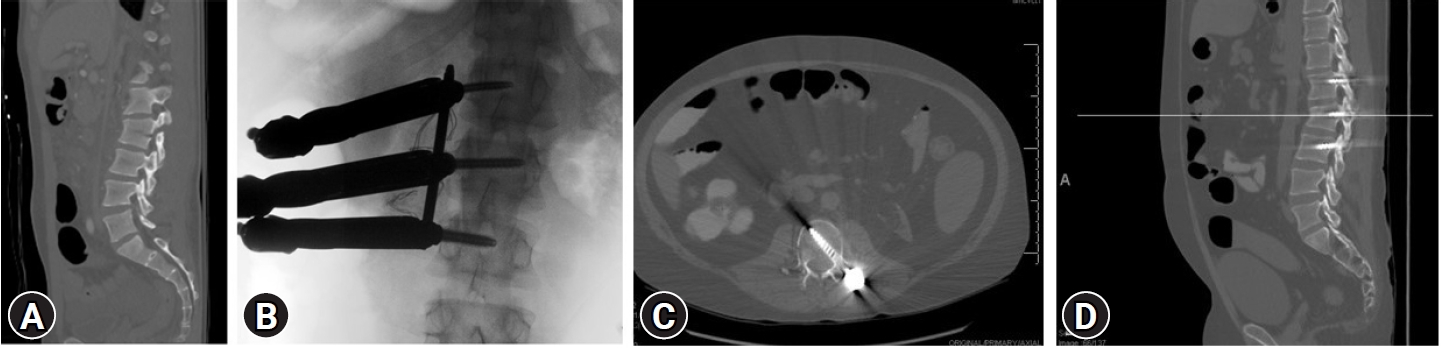
Coronal CT (A) pre-operative CT in the sagittal plane of a L2 flexion-distraction injury, (B) intra-operative AP X-ray with unilateral pedicle screw fixation and percutaneous towers in place, (C) post-operative axial CT with unilateral pedicle screw fixation and (D) post-operative sagittal CT at 3.5 years with healed L2 fracture without evidence of hardware failure or progressive kyphotic deformity.
While previous studies of thoracolumbar fractures provided insight on the use of percutaneous pedicle instrumentation for lower grade trauma, our study adds to the literature specifically with regards to MISS approaches for high-grade traumas. Cimatti et al. [11] obtained ODI, SF-36 PCS, and SF-36 MCS scores for patients with AO type A or B fractures who underwent percutaneous pedicle screw fixation, with half their patients receiving an additional lordorizing screw. At 3-years follow-up, their patients had lower ODI scores relative to our patients with a score of 11.68%. Our patient’s SF-12 scores can be compared with Cimatti et al.’s SF-36 scores, as previous data has shown the SF-12 to be a valid substitute for SF-36 [12]. Cimatti’s et al.’s [11] patients had lower SF-36 PCS and SF-36 MCS scores at 46 and 56, respectively, relative to our patients’ SF-12 scores.
Wang et al. [13] investigated lower grade thoracolumbar fractures as well, with most of their cases being classified AO A1-A3. They compared percutaneous to open pedicle screw fixation in 105 patients, with percutaneous screw fixation producing significantly less intraoperative blood loss, shorter recovery times, and lower ODI and VAS scores at 6-month follow-up. In their cohort, percutaneous fixation cases reported a blood loss of 100 mL and average length of stay of 1.5 weeks. Back-pain VAS and ODI scores at 23 month follow-up were 1.4±0.5 and 6.0±1.6%, respectively. Furthermore, Wang et al. [13] showed no significant difference in Cobb angles between the open and percutaneous fixation patients; the angle decreased from 15.8º pre-operatively to 9.5º at 23-month follow-up. The finding that percutaneous pedicle screw fixation decreases intraoperative blood and hospital stay without causing worsened radiographic outcomes for low-grade trauma (predominantly AO type A fractures) was also reported in many other studies, including meta-analyses by Phan et al. [14] and McAnany et al. [15-19].
Our results are comparable to those of other studies that investigated MISS techniques for higher grade thoracolumbar trauma. Zhang et al.’s [20] retrospective study compared the use of a MISS technique with Wiltse’s approach and Kambin’s triangle to the traditional open posterior technique in 50 patients with high grade upper lumbar fractures. Patients who underwent MISS had an average TLICS score of 6.5, and they experienced significantly less blood loss, length of stay, and 1-year post-operative back pain as reported on VAS. Average blood loss was reported to be 240 mL, average length of stay slightly less than 1 week, and VAS score for back pain at 1-year follow-up was 1.4 ± 0.9 [20]. Regarding percutaneous pedicle screw fixation, Ansar et al. [21] used this technique in 125 patients with high-grade thoracolumbar traumas. Patients selected for the study had either three-column injuries or new neurological deficits on presentation. Average length of stay was 14 days. At a follow-up period of 2 years post-operatively, patients had no pain or mild pain with VAS scores between 0 and 3. Such results correspond with our data of 12.5 days and 2.6 for average length of stay and back pain VAS at 20 month follow-up [21].
Previous studies have demonstrated MISS’s efficacy for lower grade thoracolumbar fractures [6-8], including decreased blood loss, shorter incisions, and reduced anesthesia time. Our study indicates that these beneficial effects are applicable for high grade thoracolumbar trauma as well. Limitations to our study include the retrospective design, lack of a comparison group, and heterogeneous patient population which inherently leads to selection bias and therefore may not be generalizable to the population at large.
Our study documents favorable patient and radiographic outcomes with the use of MISS percutaneous instrumentation for high grade thoracolumbar trauma. This cohort is the first to show that for very high-grade thoracolumbar trauma with an average TLICS score as high as 7.5, MISS techniques confer several benefits with regards to radiographic and patient survey outcomes.
Notes
Ethical statements
This study has been approved by Institutional Review Board of Albany Medical Center, USA (Approval #5231). Informed consent was not obtained nor required given the de-identified, retrospective nature of this study.
Conflicts of interest
No potential conflict of interest relevant to this article.
Authors' contribution
All four authors (MPS, MMS, PE, and JWG) were involved in substantial contributions to the conception or design of the work (including data acquisition and interpretation), drafting the manuscript and revising it, final approval of the manuscript, and agreement for all aspects of the manuscript.