AbstractObjectiveTo describe an alternative technique of annuloplasty for treatment of chronic discogenic back pain in an ambulatory setting.
MethodsA retrospective review of all patients presenting with chronic discogenic low back pain and managed by target-oriented thermal annuloplasty at our institute from May 2015 to June 2019 was performed. The procedure is carried out under local anaesthesia in prone position. The principle of the technique relies on dividing the posterior annulus into nine equal segments on AP-view of the C-arm. The trajectory is through the Kambin’s triangle in a horizontal trajectory as much as possible to target the posterior part of the disc annulus. Each of the nine segments is treated with radio-frequency probe to produce disc alterations required to relieve the pain.
ResultsA total of 9 patients were treated by this method with an average follow-up of 28.1±11.4 months. The average VAS improved from 4.1±1.2 to 2.5±0.4 at final follow-up. The ODI improved from 42±6.7 to 19.98±5.6. None of the patients had any complications. The patient satisfaction rate was 82%, the rate of return to daily life was 100% and recommendation rate to others was 100%.
INTRODUCTIONLow back pain is the most common complaint among patients with musculoskeletal disorders and has varied aetiologies including facet joint disease, spondylolysis, discogenic pain, disc herniations, etc. [1]. Discogenic pain may account for about 30–40% of these cases [2]. The management of these cases is difficult and often frustrating for the patient as well as the doctor. Many strategies have been proposed for treating back pain including, but not limited to drug therapy; multiple physical modalities like manipulation, physiotherapy, rehabilitation; interventional modalities like epidural injections, ozone injections, intradiscal electrothermal therapy, epiduroscopy and finally surgical options like fusion and artificial disc replacement. Most of these modalities have limited evidence and lack of consensus [3]. Often simultaneously and/or consecutively, more than one of these options have to be applied to a given patient. An ideal intervention for discogenic pain has to be effective, as little invasive, evidence based and cost-effective. However, such an ideal approach is hypothetical. Failure of conservative management is often an indication for surgery such as fusion, disc replacement or endoscopic discectomy. However, these procedures are not as effective and associated with significant costs, complications and morbidity [4-6]. Intradiscal electrothermal therapy involves applying heat to the posterior annulus through a catheter with a temperature-controlled heating coil. It proves to be a minimally invasive option whose effectiveness has been fairly substantive in the literature [7-12]. Numerous techniques of the procedure have been described. In this paper, the authors describe their technique of annuloplasty at nine different strategic locations on the posterior annulus using the DiscFx® system and report how this technique may be a better alternative than those described elsewhere.
MATERIALS AND METHODSAfter obtaining permission from the institutional review board, we performed a retrospective analysis of patients treated at our institute from May 2015 to June 2019 for chronic discogenic back pain by target-oriented thermal lumbar annuloplasty (The Elliquence Disc-FX® System, Elliquence, LLC, Baldwin, NY, USA). Inclusion criteria were patients with chronic discogenic low back pain (>6 months), failed conservative treatment, pain aggravated on sitting and forward leaning (sitting intolerance) and reduced by standing and walking; and pain temporarily improved by epidural steroid injection. Patients with frank disc herniation, leg pain and those treated by other methods such as fusion were excluded. The data were analysed to find the demographic data such as age, sex, presenting complaints; clinical data included VAS (visual analogue scale) for back pain and ODI (Oswestry disability index) at pre-op, post-op and 1, 3, 6 months and 1-year follow-up. The MRI records were analysed to identify the levels affected.
1. IndicationsThe key to a successful outcome is proper patient selection. The selection criteria includes following:
• Patients with non-radicular, chronic low back pain (>3 months), not relieved conservatively. A typical patient with discogenic pain has aggravated pain on flexion, sitting intolerance and a catch on active extension of the spine.
• Negative neurological signs including straight leg raise test (SLRT), normal power, tone, sensation and reflexes of lower limbs
• The MRI should show a degenerative disc disease with a hyper-intense zone (HIZ) in the posterior annulus, without evidence of disc herniation or canal stenosis or facet arthrosis. The disc protrusion should be <5 mm and disc height should be at least 50% of the adjacent levels
A positive provocative discogram- the role of a discogram is controversial and the author do not recommend it. However, it may be recommended for ambiguous cases. A discography helps to analyse the disc architecture and the target points for ablation.
2. Pre-operative AssessmentThe first modality of treatment in a chronic, axial back pain patient in our clinic is a medial branch block (MBB). This helps us to identify a component of facet joint pain in these patients [13]. If the pain relief by MBB is insignificant, the next modality is an epidural block. If an epidural block is effective, it can be repeated up to 2 times [14]. For long term benefits, an option of annuloplasty is offered to the patient in whom epidural block relieves the back pain significantly. Our workflow is shown in Figure 1.
3. Relevant Surgical AnatomyThe knowledge of Kambin’s triangle forms the foundation for all transforaminal procedures. Kambin’s triangle is a window of entry into the lumbar spinal canal. It is dorsolateral to the spinal canal and bounded medially by the traversing nerve root and the superior articular process; the base is formed by the superior endplate of caudal vertebrae and the hypotenuse is formed by the exiting nerve root. The trajectory for needle placement is planned on MRI as is done in endoscopic procedures [15].
4. Analysis of the Pain Generators and Planning the Needle TrajectoryThe MRI should be carefully evaluated to find the hyper-intense zone of inflammation that is the cause of pain in these conditions. We believe that there are three components to a disc protrusion as described in Figure 2. The innermost portion is the desiccated and degenerated nucleus pulposus, a fissured tract along the annulus and the terminal portion is the disc protrusion. Targeting of all three components is essential for a successful outcome of the procedure. Whereas a conventional IDET (intradiscal electrothermal therapy) targets the central disc, our method targets the pain generating intra-annular and sub-annular part of the disc. Hence, our technique requires the needle to be introduced in a more horizontal manner compared to the conventional IDET techniques. This helps us to target the pain generating sub-annular and intra-annular portions. A difference in the approach of conventional IDET and our technique is shown in Figure 3.
5. Technical DetailsThe patient is positioned prone on a Wilson frame over a radio-lucent table. A combination of local anaesthesia and conscious sedation is utilized as an out-patient procedure. Under C-arm guidance, mark the midline, the iliac crest, and the rib cage. Next, mark the transverse disc line in AP view. Then, in lateral view, draw a line parallel to the disc space. The intersection of the first and the second line is the entry point. Before making the skin incision, it is essential to palpate the lateral border the back muscles and avoid entry lateral to it as it may cause abdominal organ injury. First, place the needle in the epidural space and inject a radio-opaque dye to delineate the dural sac and the nerve roots. Then withdraw the needle and advance it deeper into the disc so that the tip of the needle lies in the center of the disc in AP view and in the posterior annulus in lateral view. Inject a small amount of dye to confirm the location of the needle. A concordant pain will be elicited. A guide-wire is put in the spinal needle and the needle is removed. Then, a dilator is placed over the guide-wire and the cannula is inserted. At this point, the cannula and the dilator are at the outer surface of the annulus. The dilator is removed and a trephine is inserted in the cannula. By gentle rotations of the trephine, the annulus is cut and the trephine is advanced to the midline. The cannula is then advanced over the trephine. Remove the trephine and reintroduce the dilator to enlarge the annular tract. The position of the guide-wire, dilator and the cannula is verified by C-arm. Remove the dilator and the guide-wire and use the cannula as the working channel. With the help of a disc punch, remove the disc material from the midline. First introduce the disc punch with the jaw opening ventrally and grasp the tissue to be removed. Then rotate the disc punch by 180° and remove the disc from the dorsal side. This is done under C-arm guidance. Now introduce the electrothermal probe for ablation. The system is a bipolar electrode with a saline flowing from the tip of the electrode. The power is set at “25” and the probe is pressed against the tissue for 6 seconds under “turbo” mode. It is important to note that during this process, the bevel of the cannula faces ventrally. Squeezing the handle makes the bipolar electrode extend out of the distal end of the shaft and point upward. This allows the bipolar tip to be guided as required. This procedure will be repeated 6 times; once at 12, 2, 4, 6, 8, and 10 o’clock sequentially. In the nine point annuloplasty part, the bipolar hemo (blue pedal) is used. The probe is held in the vertical position so the tip will come out and up (dorsally). The tip will be rubbing along the internal portion of the annulus where the disc is bulging. Squeeze and hold the handle to perform three 6 seconds sweeps using a sawing motion at 11:00, 12:00, and 1:00. This can be performed at 9 target points in the center, ipsilateral and contralateral part of the disc. These locations are center cranial, center central, center caudal, contralateral cranial, contralateral central, contralateral caudal, ipsilateral cranial, ipsilateral central, ipsilateral caudal. A diagrammatic representation of the procedure in shown in Figure 4. The 9 point as seen on C-arm are showing in Figure 5. After the procedure, the patient is observed for about 3 hours in the ambulatory spine care setting and can be discharged on the same day. A lumbosacral orthosis is given for 3–4 weeks. The pain is expected to flare up in the initial few weeks which subsides gradually. Forward bending is allowed after 3–4 weeks. Back range of motion and strengthening exercises are advised after 6 weeks. Heavy work is usually avoided for 6 months.
RESULTSA total of 9 patients (5 males and 4 females) were included in the study with an average follow-up of 28.1±11.4 months. There were 6 patients who had the procedure at L4-5 level and one patient each at L2-3, L3-4, and L5-6. The average VAS improved from 4.1±1.2 to 2.5±0.4 at final follow-up. The ODI improved from 42±6.7 to 19.98±5.6. None of the patients had any complications. The patient satisfaction rate was 82%, the rate of return to daily life was 100% and recommendation rate to others was 100%. The MacNab criteria were excellent in 7 and good in 2.
Representative Case ExampleA 28 years old male patient with chronic low back pain and sitting intolerance presented to us. He had tried all conservative options but failed to get a permanent relief. His VAS back was 6. The pain was relieved on supine posture. A standing lateral X-ray of the lumbar spine showed reduced segmental lordosis at L4-5. An MRI of the lumbar spine showed a degenerative disc disease at L4-5 level with no canal stenosis or root compression. A nine point annuloplasty relieved his symptoms. At 3-month follow-up, his VAS reduced to 2 and completely relieved at 6-month follow-up. The patient satisfaction with the procedure was good. Follow-up X-rays showed improvement in the segmental lumbar angle and whole lumbar lordosis. The radiographic images are depicted in Figures 6,7.
DISCUSSIONEver since the first description of this procedure in 2000 by Saal and Saal [10], numerous reports have been described in the literature regarding electrothermal therapy. Various techniques have used thermal, bipolar, laser and radio-frequency probes as modes of coagulation. Although the exact mechanism of action is unknown, various theories postulate that the heat causes denaturation of collagen leading to increased stiffness, ablation of the nociceptors and shrinkage of the size of the annular defect leading to decreased secretion of pain generating chemo-mediators [16]. The heat required to produce these changes in the disc architecture has been determined to be in the range of 60–75 degrees C in various studies [17,18]. The conventional IDET involves placement of the needle in the center of the disc and negotiation a long probe in a circumferential manner into the sub-annular area for coagulation [8,12,19,20]. However, with various in-vivo and in-vitro studies, it was concluded that the central placement of the probe was undesirable since the pathology is in the posterior annulus [21].
Our technique of nine point annuloplasty ensures that the entire posterior annulus which is the site of pain generating receptors is effectively dealt by the coagulation therapy. All our patients improved significantly with respect to VAS for back and ODI. The procedure can be applied as a day-care procedure with good patient acceptability and high satisfaction rates and minimal complications. The sequential ablation by diving the entire posterior annulus into 9 quadrants is helpful so that no part is left untouched and thus ensuring the adequacy of ablation. The principal difference with our technique is the trajectory of the needle and the probe placement. A more horizontal approach puts the device in close proximity to the pathology. A central placement of the device, as in conventional IDET, is not sufficient to generate enough heat at the site of pathology [16,17,22]. The heating effect of the probes is negligible beyond 6 mm radius from the device. The temperatures produced are capable of inducing changes only in 1–2 mm radius from the device [17]. Thus placement of the probe according to our technique is a more target-oriented approach to the pathology. Furthermore, the central nucleus is not damaged by this approach. The three components of the DDD, the desiccated nucleus, the fissured tract as well as the annular bulge, all three can be dealt by our technique. Although the alteration of the disc architecture may alter the biomechanical properties of the affected segment, cadaveric studies have failed to demonstrate the same and conclude that the heat therapy does not destabilize the vertebral segment [18,23].
Literature support favoring electrothermal therapy is fairly sufficient with numerous level 1 evidences. We believe that the key to a successful outcomes depends upon proper selection criteria and proficient execution of the procedure. A multimodal approach, with supervised physical therapy, ergonomic modifications and psychosocial rehabilitation are essential for a good outcome. Although fusion and disc replacement have been described in literature for management of these conditions, the lack of high quality evidence regarding their efficacy and the morbidity and cost associated with these technique warrant further investigation [24]. Annuloplasty, on the other hand, has fewer complications and is minimally invasive. The procedure is quite safe with experienced hands. The North American Spine Society guidelines for management of low back pain also state that “Intradiscal electrothermal annuloplasty is suggested to provide improvements in pain and function up to 2 years. This treatment is limited in effectiveness with roughly 40–50% of patients receiving a 50% reduction in pain”. A reference table from the NASS guidelines is quoted (Table 1).
Four randomized control trials comparing electrothermal therapy with placebo have been published. Three out of four provide sufficient reinforcement to this technique [7,9,16,25]. Desai et al. [7] performed a prospective multi-center RCT comparing intradiscal biacuplasty with medical management for discogenic lumbar back pain and found superior results with electrotheramal therapy. However, this study involved placement of bilateral probes for ablation. Pauza et al. [9] randomized 64 patients and found better improvements in pain, disability and depression in the IDET group. Karasek and Bogduk [26] reported their 12-month follow-up of controlled trial of IDET for discogenic back pain in 53 patients. They concluded that 54% of the patients reduced their pain by half and 1 in 5 patients had complete relief. Apart from these, numerous observational studies also provide significant evidence of its efficacy [4,10-12,19,20,27,28]. Saal and Saal [11] reported IDET in 62 patients who were followed up for 2 years and showed favorable outcomes. Although the complication rate is low, they have been described in literature and include discitis, catheter breakage, root injury, vertebral osteonecrosis, trans-thecal puncture, cauda equina syndrome.
Contra-indications and LimitationsThe procedure is contraindicated in presence of instability, frank disc herniation, stenosis (greater than Grade B of Schizas classification [25]) and in those who had surgery at the same level in the past 6 months. Familiarity with the transforaminal anatomy is essential to carry out the procedure safely. Also, in cases with a high iliac crest, it is difficult to obtain a satisfactory positioning of the probe.
CONCLUSIONBeing a minimally invasive option, nine point annuloplasty may be considered as a viable option for chronic discogenic back pain patients with relatively well-maintained disc heights and protrusions less than 5 mm. It is a more target-oriented approach and preserves the central nucleus. A successful outcomes depends upon proper patient selection and correct trajectory.
NOTESFigure 1.Flow-diagram depicting the step-wise management of chronic discogenic low-back pain patient. 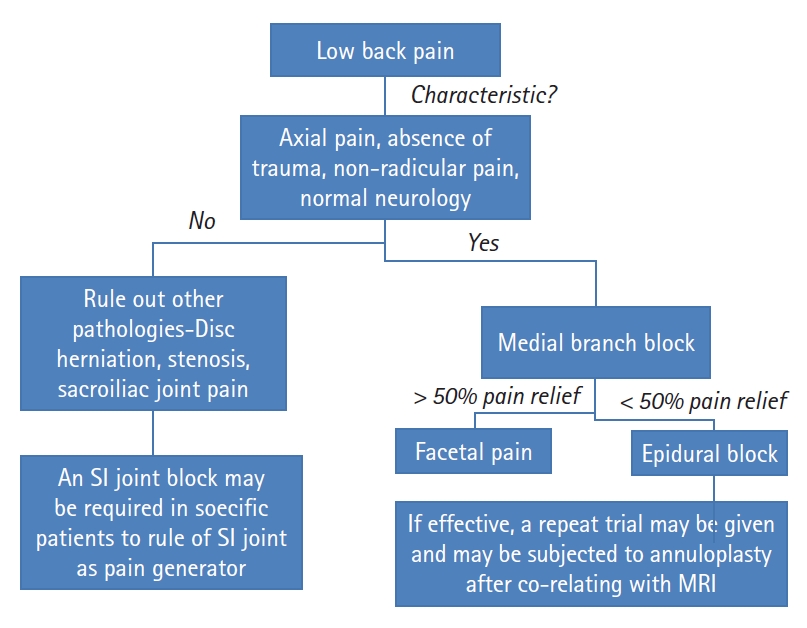
Figure 2.Sagittal and axial view of an L4-5 degenerative disc disease showing the three pain generating components. White arrows show the degenerated nucleus pulposus, red asterisks show the tract of herniation and yellow solid arrows show the bulging disc. 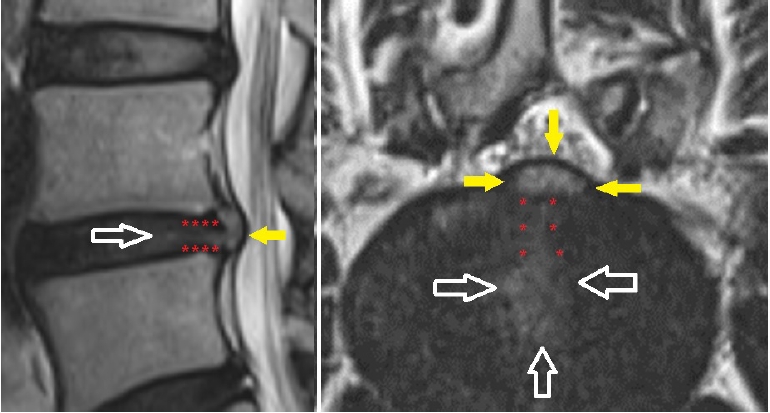
Figure 3.(A) Show the ideal target oriented trajectory as described in our technique, (B) pathological specimen showing pain-generators in the posterior annulus (described by white arrows) and (C) conventional IDET method. 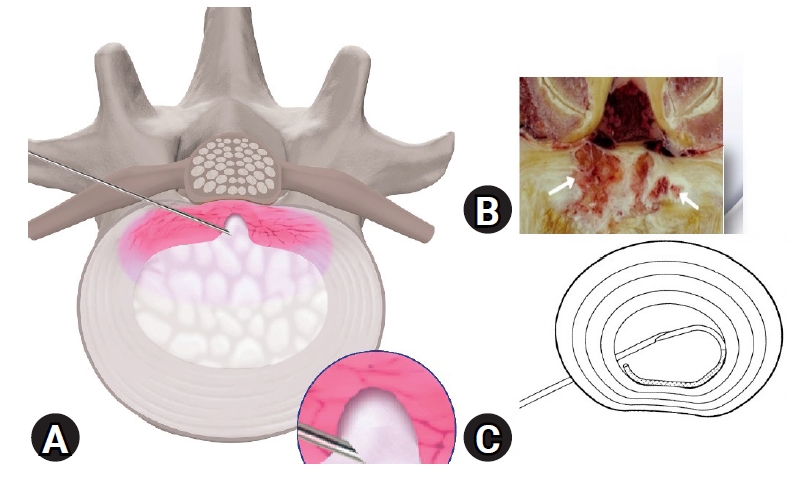
Figure 4.Schematic diagram showing step-wise procedure. (A) Spinal needle insertion; inset showing epidurography; (B) guide wire insertion; (C) insertion of dilator and cannula over the guide wire up to the outer surface of annulus; (D) annulotomy with a trephine; (E) advancement of cannula below the center of the posterior annulus; (F) verifying the correct position of the working cannula under C-arm (shown in inset); (G) grasping forceps is used to remove parts of disc to create a working space; (H) the radio-frequency probe is inserted, and then the nucleus and the tract of herniation are ablated; (I) annuloplasty/annulus modulation. 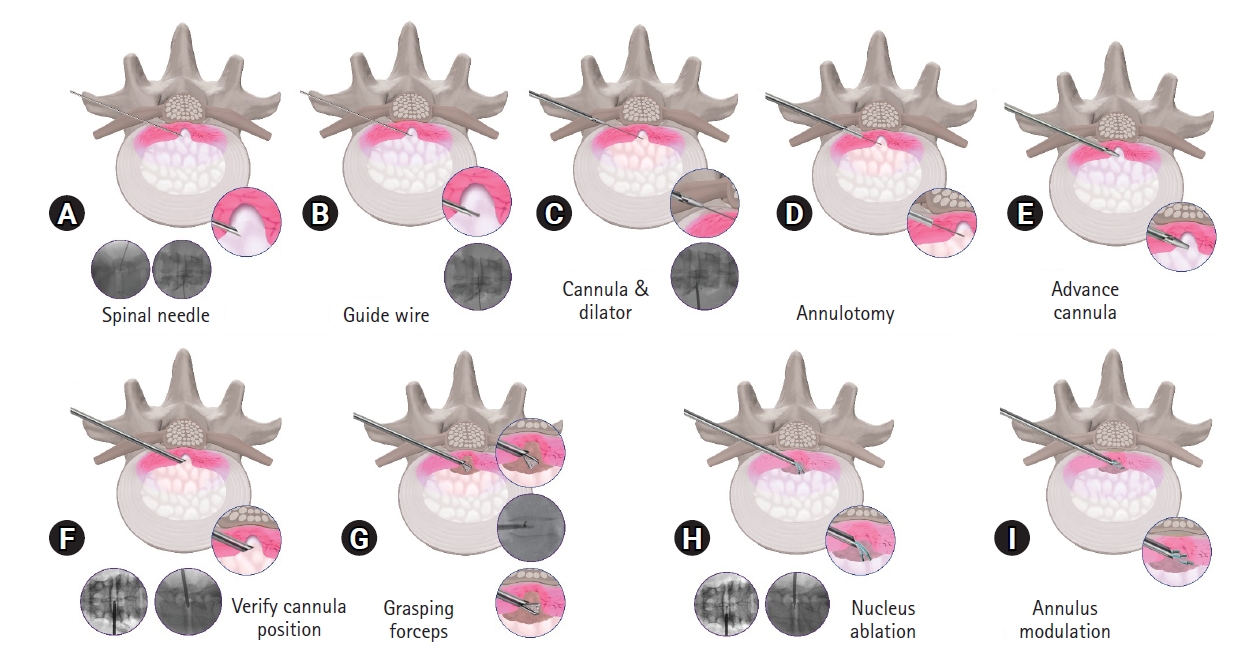
Figure 5.The 9 segments of the posterior annulus as seen on C-arm image which are targeted one by one for annulus modulation. 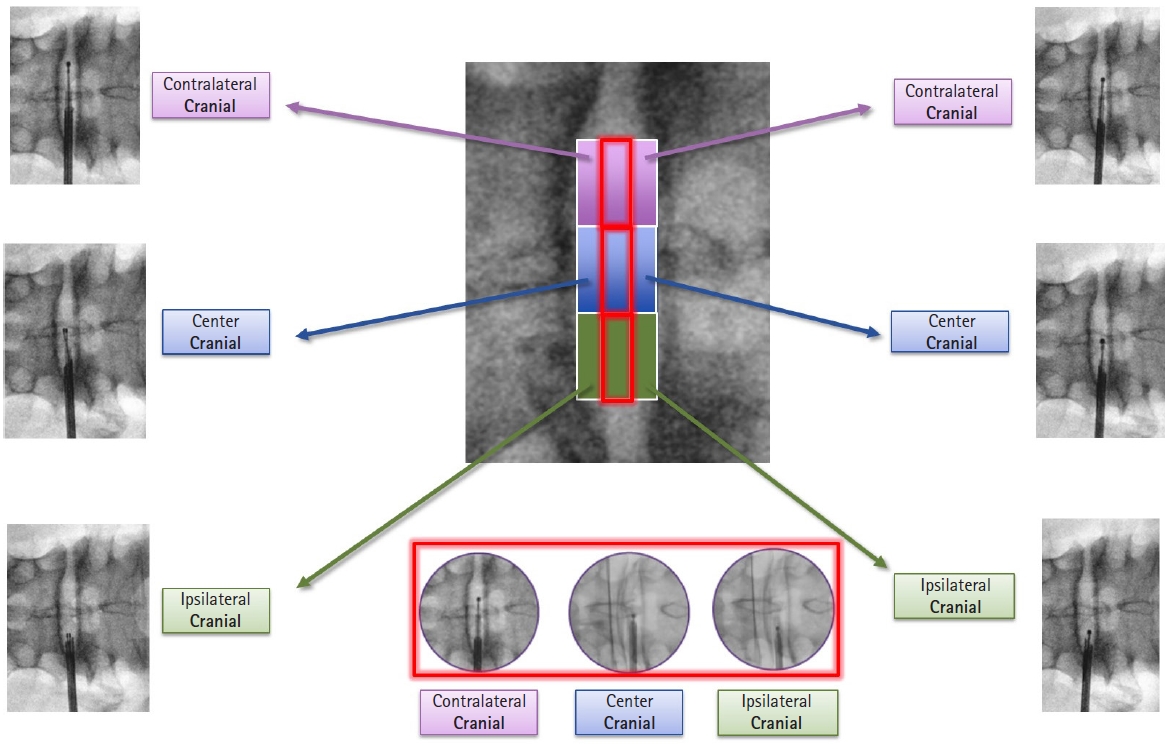
Figure 6.Pre-operative images of a 27-year old male with chronic low back pain since 2 years ago. Visual analogue scale for back was 5 out of 10. There was no leg pain. The patient had been subjected to epidural steroid injections twice in the past two years and obtained reasonable short term relief. X-ray and MRI shows degenerative disc disease at L4-5 level. 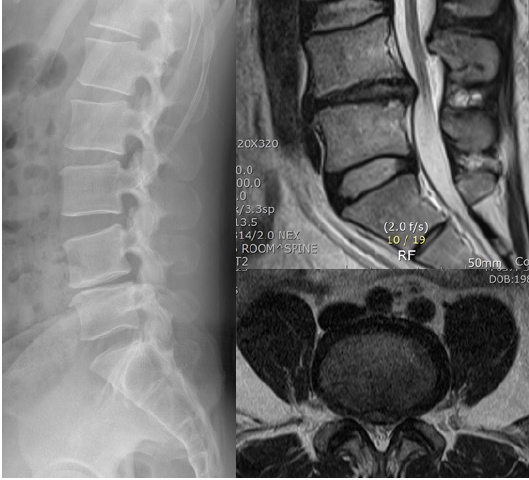
Figure 7.Comparison of pre-operative and follow-up images to show improvement in the spinal sagittal parameters, lumbar lordosis and segmental lordosis. VAS improved to 0 out of 10 at 6-month follow-up. 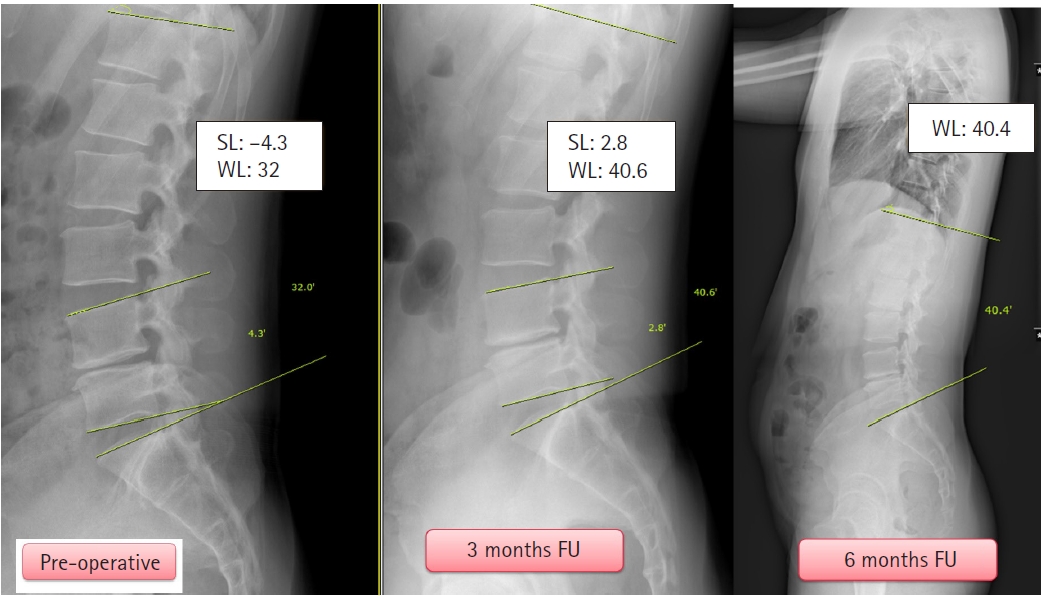
Table 1.Summary from the NASS guidelines depicting the grade of recommendation of intra-discal thermal annuloplasty for low back pain REFERENCES1. Papageorgiou AC, Croft PR, Ferry S, Jayson MI, Silman AJ. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine (Phila Pa 1976) 1995;20:1889–1894.
2. Fujii K, Yamazaki M, Kang JD, Risbud MV, Cho SK, Qureshi SA, et al. Discogenic back pain: literature review of definition, diagnosis, and treatment. JBMR Plus 2019;3:e10180.
3. Zhao L, Manchikanti L, Kaye AD, Abd-Elsayed A. Treatment of discogenic low back pain: current treatment strategies and future options: a literature review. Curr Pain Headache Rep 2019;23:86.
4. Andersson GB, Mekhail NA, Block JE. Treatment of intractable discogenic low back pain. A systematic review of spinal fusion and intradiscal electrothermal therapy (IDET). Pain Physician 2006;9:237–248.
5. Kim HS, Sharma SB, Wu PH, Raorane HD, Adsul NM, Singh R, et al. Complications and limitations of endoscopic spine surgery and percutaneous instrumentation. Indian Spine J 2020;3:78–85.
6. Willems PC, Staal JB, Walenkamp GH, de Bie RA. Spinal fusion for chronic low back pain: systematic review on the accuracy of tests for patient selection. Spine J 2013;13:99–109.
7. Desai MJ, Kapural L, Petersohn JD, Vallejo R, Menzies R, Creamer M, et al. A prospective, randomized, multicenter, open-label clinical trial comparing intradiscal biacuplasty to conventional medical management for discogenic lumbar back pain. Spine (Phila Pa 1976) 2016;41:1065–1074.
8. Kapural L, Hayek S, Malak O, Arrigain S, Mekhail N. Intradiscal thermal annuloplasty versus intradiscal radiofrequency ablation for the treatment of discogenic pain: a prospective matched control trial. Pain Med 2005;6:425–431.
9. Pauza KJ, Howell S, Dreyfuss P, Peloza JH, Dawson K, Bogduk N. A randomized, placebo-controlled trial of intradiscal electrothermal therapy for the treatment of discogenic low back pain. Spine J 2004;4:27–35.
10. Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain: a prospective outcome study with minimum 1-year follow-up. Spine (Phila Pa 1976) 2000;25:2622–2627.
11. Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain: prospective outcome study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 2002;27:966–974.
12. Tsou HK, Chao SC, Kao TH, Yiin JJ, Hsu HC, Shen CC, et al. Intradiscal electrothermal therapy in the treatment of chronic low back pain: experience with 93 patients. Surg Neurol Int 2010;1:37.
13. Malik KM, Cohen SP, Walega DR, Benzon HT. Diagnostic criteria and treatment of discogenic pain: a systematic review of recent clinical literature. Spine J 2013;13:1675–1689.
14. Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: part 1: discogenic pain without disc herniation or radiculitis. Pain Physician 2008;11:785–800.
15. Sharma SB, Lin GX, Jabri H, Sidappa ND, Song MS, Choi KC, et al. Radiographic and clinical outcomes of huge lumbar disc herniations treated by transforaminal endoscopic discectomy. Clin Neurol Neurosurg 2019;185:105485.
16. Shah RV, Lutz GE, Lee J, Doty SB, Rodeo S. Intradiskal electrothermal therapy: a preliminary histologic study. Arch Phys Med Rehabil 2001;82:1230–1237.
17. Kleinstueck FS, Diederich CJ, Nau WH, Puttlitz CM, Smith JA, Bradford DS, et al. Temperature and thermal dose distributions during intradiscal electrothermal therapy in the cadaveric lumbar spine. Spine (Phila Pa 1976) 2003;28:1700–1709.
18. Wang JC, Kabo JM, Tsou PM, Halevi L, Shamie AN. The effect of uniform heating on the biomechanical properties of the intervertebral disc in a porcine model. Spine J 2005;5:64–70.
19. Helm Ii S, Deer TR, Manchikanti L, Datta S, Chopra P, Singh V, et al. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician 2012;15:E279–E304.
20. Urrútia G, Kovacs F, Nishishinya MB, Olabe J. Percutaneous thermocoagulation intradiscal techniques for discogenic low back pain. Spine (Phila Pa 1976) 2007;32:1146–1154.
21. Peng B, Wu W, Hou S, Li P, Zhang C, Yang Y. The pathogenesis of discogenic low back pain. J Bone Joint Surg Br 2005;87:62–67.
22. Derby R, Seo KS, Kazala K, Chen YC, Lee SH, Kim BJ. A factor analysis of lumbar intradiscal electrothermal annuloplasty outcomes. Spine J 2005;5:256–262.
23. Lee J, Lutz GE, Campbell D, Rodeo SA, Wright T. Stability of the lumbar spine after intradiscal electrothermal therapy. Arch Phys Med Rehabil 2001;82:120–122.
24. Hansson T, Hansson E, Malchau H. Utility of spine surgery: a comparison of common elective orthopaedic surgical procedures. Spine (Phila Pa 1976) 2008;33:2819–2830.
25. Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 2010;35:1919–1924.
26. Karasek M, Bogduk N. Twelve-month follow-up of a controlled trial of intradiscal thermal anuloplasty for back pain due to internal disc disruption. Spine (Phila Pa 1976) 2000;25:2601–2607.
|
|
|||||||||||||||||||||||||||||||||||||||