The Italian Landscape of Spine Endoscopy: Are We Ready for the Challenges of the Future?
Article information
Abstract
Objective
Endoscopic spine surgery is gaining popularity, with efficacy comparable to that of traditional techniques. Apart from Germany, European countries are tentatively beginning to consider endoscopic surgery as a valid alternative to conventional procedures, and Italy is no exception. This survey aimed to reveal which spine surgeons currently use endoscopy in Italy, the levels of their skills, and how they have attained them.
Methods
We conducted an online survey of Italian spinal surgeons to gather information about their use of minimally invasive and endoscopic surgery. We collected data on their operating habits, including the percentage of minimally invasive techniques in their practice, the type of workplace, and experience. We also asked surgeons to analyze and resolve 4 cases of degenerative lumbar pathologies.
Results
Orthopedists and neurosurgeons in public and private facilities performed endoscopic surgery. One-third of respondents had never tried it, while others encountered it through workshops or producer presentations. A minority of interviewees considered themselves experts in endoscopic surgery, while more than half had “some” or “no” experience. Among endoscopic surgeons, none had experience in thoracic endoscopy, and only a few had used it for cervical diseases. The majority preferred a non-endoscopic approach when faced with clinical cases.
Conclusion
The use and knowledge of endoscopic surgery in Italy are not widespread. Our survey highlights a lack of training in the implementation of techniques that should be recognized as additional tools in addition to the traditional procedures for treating not only lumbar, but also thoracic and cervical pathologies.
INTRODUCTION
Endoscopic spine surgery has gained popularity in the last 2 decades and has become the least invasive surgical option of the open and mini-invasive techniques [1]. Its development and use worldwide [2] is an ongoing trend, accompanied by a rising number of randomized and nonrandomized studies proving its efficacy and safety in treating several degenerative spinal conditions. Among spine endoscopic procedures, the most developed one, with the most promising potential, is uniportal full-endoscopic surgery, either in the interlaminar or transforaminal form [3]. This technique acquired popularity in treating lumbar spine conditions such as disc herniations and foraminal stenosis [4], with surgeons proving its efficacy compared to traditional open techniques. Recently, several authors have also successfully expanded its field of application to the thoracic and cervical spine, not only in degenerative diseases but also in neoplastic and infectious ones [5].
However, a skewed distribution was found in the use and indications of endoscopy spine surgery worldwide, with Asian countries currently leading the field [6,7]. Apart from Germany, European countries have only recently and hesitatingly considered endoscopic spine surgery as a valuable alternative to traditional techniques [8,9]. Italy is no exception: only in the last few years have spine surgeons started exploring and taking an interest in full-endoscopic spine surgery (FESS) [10-12].
Indeed, only recently, this technique aroused the interest of the National Neurosurgery and Orthopedic spine surgeon committee, with expertise shared in national meetings, courses and workshops.
Therefore, this study is a snapshot of those who are currently performing endoscopic lumbar spinal surgery in Italy, the level of their skills and how they came across the practice. We intend to use this information to encourage Italian spine surgeons to consider FESS for lumbar decompression procedures.
MATERIALS AND METHODS
We invited spine surgeons from Italy to respond to an online survey via email and chat groups on social networks, including WhatsApp and LinkedIn. The survey was available online, with a link that took the responding surgeon to the Microsoft Forms website, where the survey was displayed automatically. Participants could enter their answers by means of a desktop computer, laptop or a hand-held device such as a tablet or smartphone.
The questions sought to solicit essential information on the use and distribution of mini-invasive and endoscopic surgery. We also collected information about the surgeons’ methods, including the percentage of his/her practice devoted to mini-invasive techniques or FESS, the type of workplace, expertise, and surgical indications. More specifically, the survey focused on the distribution and use of FESS techniques.
The survey was made up of simple multiple-choice questions, some with many possible answers, in order to make it easy to use, maximize respondent retention once on the website and facilitate its completion.
In the first part of the survey, surgeons were asked the following 4 questions:
(I) Please select your profession
(i) Neurosurgeon; (ii) Orthopedic surgeon; (iii) Others (anaesthesiologist/pain therapist)
(II) Please indicate your city.
(III) What kind of healthcare facility do you work for?
(i) Public/Government Hospital; (ii) Private/ affiliated health care facility
(IV) Please quantify your experience in minimally invasive surgery:
(i) No experience; (ii) Some experience (<20 cases); (iii) Enough experience (>20 cases <70); (iv) Expert (>70 cases < 100); (v) Master (>100 / 120 cases)
(V) What kind of minimally invasive surgery do you normally use in your surgical practice?
(i) Endoscopic assisted surgery; (ii) Tubular retractor surgery; (iii) Full-endoscopic surgery; (iv) none
(VI) Please quantify the percentage of minimally invasive surgery used in your surgical practice:
(i) <25%; (ii) 25%-50%; (iii) 50%-75%; (iv) >75%; (v) Don’t know.
(VII) What kind of endoscopic surgery have you encountered during conferences, courses, videos, and presentations?
(i) Cervical; (ii) Thoracic; (iii) Lumbar; (iv) None
(VIII) What kind of endoscopic surgery do you perform?
(i) Cervical; (ii) Thoracic; (iii) Lumbar; (iv) None
(IX) How did you come across endoscopic surgical techniques?
(i) Workshops; (ii) National and International Congresses; (iii) National Society of Surgery; (iv) Promotional advertisement
(X) What approaches are you familiar with in endoscopic surgery?
(i) Interlaminar; (ii) Transforaminal; (iii) None
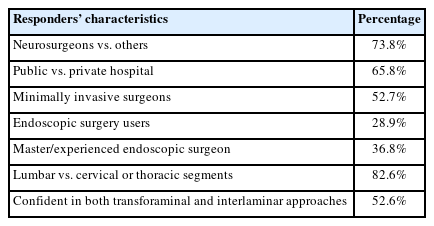
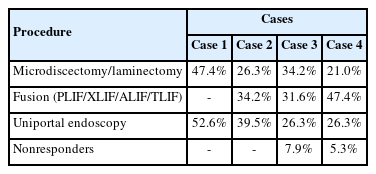
In the second part, the survey asked surgeons to analyze and solve 4 different lumbar degenerative cases with multiple-choice answers (see Figure 1 for an explanation of multiple-choice selection).
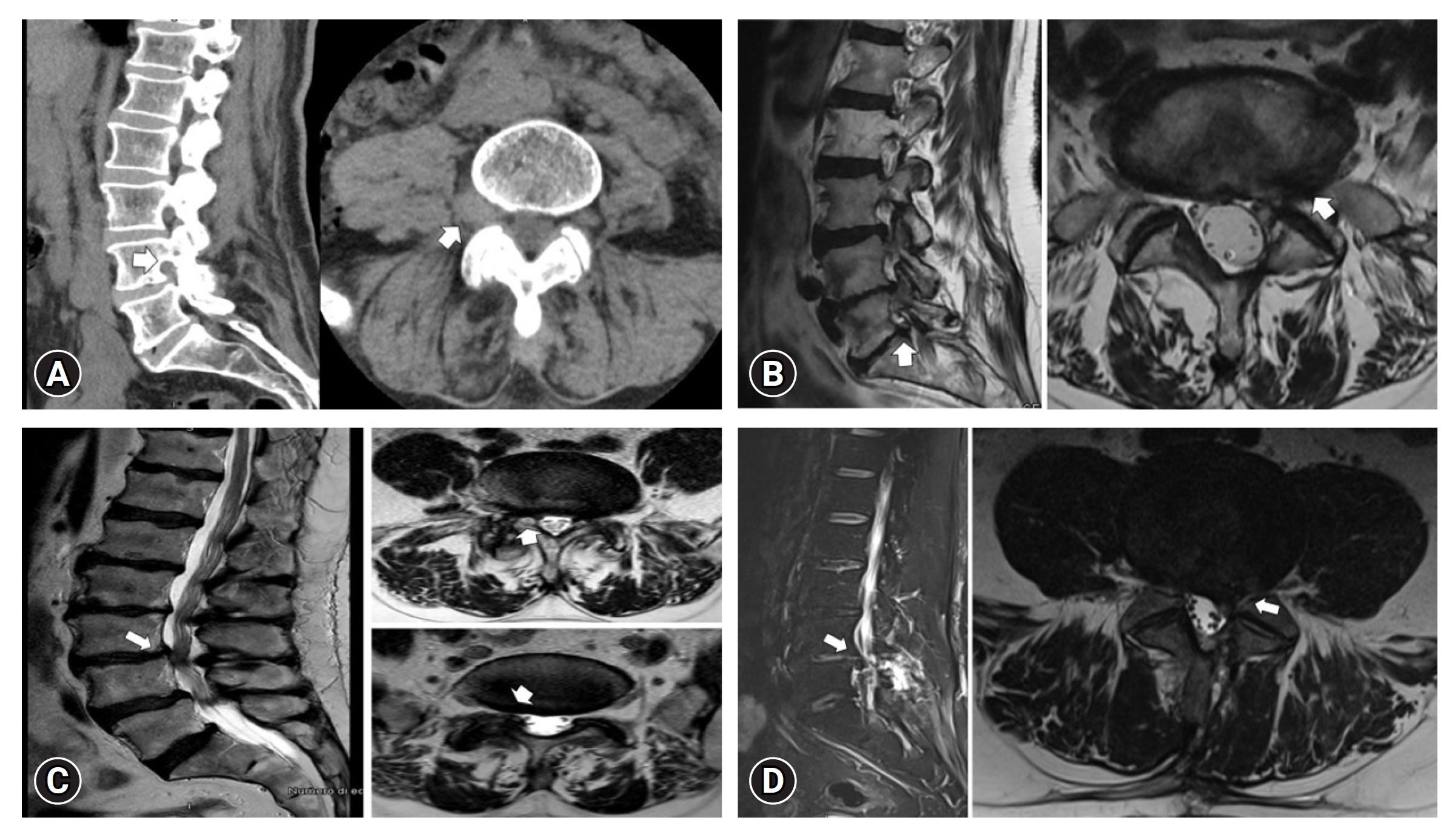
(A) Right extraforaminal disc herniation in L4–5 (white arrows): Extraforaminal microsurgical discectomy versus discectomy + fusion at L4–5 (TLIF, XLIF, ALIF) versus transforaminal full-endoscopic discectomy versus interlaminar full-endoscopic discectomy. (B) Left L5–S1 intra-extraforaminal hernia (white arrows) in the context of L4–5 and L5–S1 degenerative disc disease (Modic I): microsurgical discectomy versus L4–5 and/or L5–S1 fusion (PLIF/TLIF/ALIF) versus transforaminal full-endoscopic discectomy versus Interlaminar full-endoscopic discectomy. (C) Foraminal stenosis in L3–4 and L4–5, central stenosis in L3–4 and degenerative listhesis in L4–5 (white arrows, grade I): L3–4 laminectomy versus L4–5 and/or L5–S1 fusion (PLIF/TLIF/ALIF) versus transforaminal full-endoscopic discectomy versus interlaminar full-endoscopic discectomy. (D) Left L4–5 foraminal herniation (white arrows): Repeated microsurgical microdiscectomy versus L4–5 and/or L5–S1 fusion (PLIF/TLIF/ALIF)) versus transforaminal full-endoscopic discectomy versus interlaminar full-endoscopic discectomy. PLIF, posterior lumbar interbody fusion; ALIF, anterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; XLIF, extreme lateral lumbar interbody fusion.
The cases were:
I. A 56-year-old male. Right radiculopathy, unresponsive to medical treatment.
Body mass index (BMI): 27 kg/m2, visual analogue scale (VAS): 10/10
Right extraforaminal disc herniation in L4–5 (Figure 1A)
II. A 47-year-old, male. Long-lasting and drug-resistant left radiculopathy (VAS 8/10). Moderate axial back pain (VAS 4/10), BMI: 26 kg/m2
Left L5-1 intra- and extraforaminal hernia in the context of L4–L5 and L5–S1 degenerative disc disease (Modic I) (Figure 1B)
III. A 74-year-old female. Chronic and disabling right radiculopathy in L3 and L4 nerve root territory. Low axial back pain (VAS: 3/10), BMI: 29.8 kg/m2
Foraminal stenosis in L3–4 and L4–5, central stenosis in L3–4 and degenerative listhesis in L4–5 (grade I) (Figure 1C)
IV. A 52-year-old, 3rd recurrence (L4–5 microdiscectomy in 2020 and 2021). Disabling radiculopathy (VAS: 9/10), BMI: 32 kg/m2
Left L4–L5 foraminal herniation (Figure 1D)
The cases presented were all treated successfully by means of uniportal full-endoscopic transforaminal foraminotomy and discectomy. Each case was operated on by the same surgeons (JDV and EG) who had trained in basic and advanced endoscopic techniques and completed the endoscopic learning curve (150 and 100 cases, respectively) [13]. In the follow-up at 12 months, all patients confirmed the continuing satisfactory resolution of the radicular pain. Those cases were explicitly chosen as representative of the most common pathologies suitable to be treated successfully via a full-endoscopic transforaminal approach. Those are also the first conditions to be considered by a spine surgeon approaching endoscopy. Specifically, those cases were put on the order of difficulty, starting from extraforaminal herniation (I) to intra-extraforaminal compression (II), which requires adequate knowledge of the foraminal area and skills to change working channel and endoscope position, continuing to foraminal stenosis that requires adequate drilling/reaming of the neuroforamen from the exit to the entry zone (III) and eventually a revision case in which the surgeon must deal with postoperative adherences and that configures an additional challenging to the transforaminal technique (IV). Those cases could be treated with different approaches. We intended to show how the endoscopic technique could efficiently cover those mild painful spine conditions.
The survey was conducted between the 1st of October, 2022 and the 1st of January, 2023. The identities of the responding surgeons remained unknown to the authors. Individual personal identifiers were not recorded. The responses were downloaded as an Excel file once the survey had been completed. Descriptive statistical measures were used to count responses and calculate the mean, range, standard deviation and percentages.
This study did not involve human subjects and did not require Institutional Review Board review. Patients provided informed consent for image use.
RESULTS
The online survey was sent to surgeons at 51 public and private facilities with a renowned spine department in Italy. Thirty-eight surgeons, each from a different facility, submitted valid responses. The completion rate was 74.5% and, on average, the survey took 4 minutes and 59 seconds. The majority of participating surgeons were neurosurgeons (28 of 38, 73.8%), followed by orthopaedists (5 of 38, 13.1%) and anaesthesiologists/pain therapists (5 of 38, 13.1%).
The geographical distribution of the responding centers is shown in Figure 2. Most responding surgeons operated under public health regimes (25 of 38, 65.8%), while the rest (34.2%) were in private facilities. Most responding surgeons (52.7%) used mini-invasive techniques in <25% of their surgical practice, 15.8% between 25 and 50%, 10.5% between 50% to 75%, and 13.2% for >75% of cases. The remaining 7.8% of surgeons were not able to quantify it.

Distribution of the responding surgeons. The size of the dots is larger when responders come from the same area but different hospitals/clinics.
Asked what kind of mini-invasive techniques that respondents usually use in their daily surgery practice, 28.9% implemented full-endoscopic surgery, 18.4% were familiar with endoscopic assisted surgery, 10.5% mini-invasive surgery with tubular retractors, and 10.5% were proficient in a combination of mini-invasive techniques (i.e., full-endoscopic, mini-invasive with tubular retractors, endoscopic assisted). The majority, however (31.6%), reported that they did not routinely use mini-invasive techniques.
Almost one-third (28.9%) of responders rated their skill level in mini-invasive techniques, including endoscopic, as “master surgeon” and 7.9% “as experienced.” Ten point five percent of surgeons reported “adequate experience,” but the majority (52.7%) came under the “some” or “no experience” categories (Table 1).
Asked what kind of FESS surgery they encountered in their surgical practice, the vast majority (71.0%) replied lumbar endoscopic surgery, 7.9% lumbar and thoracic or cervical endoscopic surgery and 21.1% had never heard of FESS.
One-third (31.7%) of surgeons stated that they had learned and increased their knowledge about FESS from the promotional advertisements of endoscopic systems producers. Another 23.8% attended international and national meetings to learn about spinal endoscopy, 34.2% of surgeons performing endoscopic spinal surgery encountered FESS in workshops and training courses. Only 10.5% were informed by their respective national surgery society.
Thirty-six point one percent of surgeons questioned had never tried endoscopic surgery. Conversely, the experience of 82.6% of surgeons in the field was limited to the lumbar segment and only 8.3% to the cervical spine. No surgeon reported having tried thoracic full-endoscopic techniques.
Overall, 18.4% of responders were aware of the transforaminal technique, 15.8% of the interlaminar one, and the majority (52.6%) were aware of both approaches. Only 13.2% had never heard about different kinds of approaches applicable to FESS.
1. Solutions to the Cases
In the first case, most responders (52.6%) said they would adopt a full-endoscopic transforaminal endoscopic approach. The rest would all prefer a traditional microscopic extraforaminal microdiscectomy.
In the second case, 26.3% of surgeons chose to fuse the levels concerned, and 34.2% opted to perform an open microdiscectomy. Most (36.9%) would choose a full-endoscopic transforaminal discectomy. Only 1 surgeon (2.6%) would have performed endoscopic interlaminar discectomy and foraminotomy.
In the third case, 31.6% opted for interbody fusion and posterior arthrodesis. In comparison, 34.2% would perform a traditional open or mini-invasive laminectomy and foraminotomy, and 26.3% would have used a uniportal endoscopy. Among the latter, 1 surgeon (2.6%) would have chosen an endoscopic interlaminar discectomy and foraminotomy approach. Three surgeons (7.9%) did not reply.
In the fourth and last case, 47.4% of surgeons would have performed an interbody fusion and posterior arthrodesis, 21.0% opted for a repeated open microdiscectomy, and the remaining 26.3% a full-endoscopic transforaminal discectomy. Two surgeons (5.3%) did not reply.
The decisions in the cases are summarized in Table 2
DISCUSSION
This survey set out to understand and demonstrate FESS distribution among spine surgeons in Italy, its field of application and the reason for its slow take-up among practitioners. Over 160 nationwide clinics, including public or private facilities, have a dedicated spine team and treat spine disease selectively at different complexity levels. Of these facilities, 51 were reachable and were appropriately invited to respond. Eventually, the response rate was approximately 75%, possibly due to the lack of formal investigation support and spine center presentation from the orthopedics and neurosurgical societies. In addition, endoscopic surgery is still a novelty in Italy, and some surgeons may not be able to fill adequately the survey, thus discouraging them from responding. Most responders reflected the dichotomy underlying the training of spine surgeons: Neurosurgery versus Orthopedics. In Italy, neurosurgeons seem more like to perform endoscopic spine surgery than orthopedists. This trend contrasts with the registered worldwide prevalence of orthopedists operating in the endoscopic field [7]. However, it may just be a consequence of the significant differences in surgical procedures performed on the spine, where neurosurgeons deal with milder degenerative conditions daily [7,14].
We also highlight that public and private centers have surgeons operating in the endoscopic spinal field, although public centers have a higher caseload, probably due to the initial high costs of spine endoscopy and an imprecise reimbursement system that, in past years, may have discouraged spine surgeons from applying this technique in a private setting [15]. Recently, however, the cost of materials and instruments has fallen dramatically, encouraging more surgeons to consider FESS in private practice for treating minor degenerative spine problems. However, endoscopic approaches are not yet coded, possibly generating confusion regarding reimbursement for health facilities. In countries with insurance-based health systems, spine surgeons happily embraced a technique with comparable outcomes but lower operation times and fewer adverse events than traditional open procedures [16,17]. FESS can also safely be performed under local anaesthesia and conscious sedation, preferably with neuromonitoring, thereby extending its applicability to elder and polymorbid patients [18-21].
In surgical practice, we confirmed that most surgeons are confident with the mini-invasive technique with or without endoscopic assistance. However, less than a third employ FESS to some extent in everyday practice. Despite several randomized trials proving that the rate of adverse events in endoscopic surgery is lower than the microsurgical approach [22-25], along with lower operation and discharge times [25,26], the dissemination of research and operational application is limited in the Italian endoscopic spinal landscape. Over a third of responders had never tried FESS or even heard of it. Most of those who had heard of FESS had only done so due to workshops; the rest attended international or national meetings, and many were informed by endoscopic system producers. For years, the dissemination and advertising of endoscopic surgery was limited to producers who mainly offered training courses abroad. Today, Italy still lacks FESS courses or labs where surgeons can adequately train in endoscopic techniques.
These patterns may reflect an inherited cultural among Italian spine surgeons of avoiding any change to traditional surgery paradigms and the tardiness of national and international spine surgery committees in recognizing the versatility and applicability of FESS.
Indeed, one reason for the poor dissemination of FESS may be linked to the lack of structured training and formal fellowships. Unlike other countries with proper training, FESS surgeons in Italy mainly improve their skills by teaching themselves. This lack of training makes it especially difficult for young residents to properly access endoscopic surgery under guidance. While improving his surgical anatomical orientation, a young surgeon may significantly take advantage of endoscopic reasoning, anatomical point of view, and surgical coping strategies.
A common misconception is that the learning curve of FESS is very steep and it requires more than 70 cases to be considered skilled. In addition, a specific study of surgical anatomy of the foramen area and spine orientation through x-ray imagining is mandatory [27-30]. This may discourage surgeons from applying this new technique [13]. It was demonstrated that only a few survey responders have adequate FESS experience. More than half have “some” or “no experience”. In our opinion, these terms could only be applied to surgeons who were pioneers in this field. Learning from a master endoscopic surgeon would help speed up learning and avoid failures [14].
Furthermore, of those who took part in the survey, not all were aware of transforaminal and interlaminar techniques, which underlines the lack of adequate information about FESS. Such a lack of knowledge about FESS approaches could limit the perceived applicability of the technique. In Asian countries and the United States, which are leading the research into and use of FESS, a well-trained endoscopic surgeon can recognize an appropriate patient for the interlaminar and transforaminal route either in the lumbar, thoracic, or cervical segment [1,3,12]. Among Italian surgeons operating in endoscopic spine surgery, none of the responders had experience in uniportal thoracic endoscopy, the majority only with the lumbar spine, and only a small subgroup of surgeons had treated cervical segment pathologies.
The last part of our survey presented 4 different clinical cases in order to emphasize the value of FESS. The authors had successfully treated all those cases with a transforaminal approach. Although some respondents chose FESS, most still preferred the non-endoscopic approach. In the third case of a 74-year-old patient, the age should have indicated time-saving surgery in order to reduce the anaesthesiologic risk in more fragile patients. The same applies to the fourth case. To avoid the third operation through scar tissue, a virgin lateral route would have been an option, such as the transforaminal one, to prevent tissue adhesions. The answers to the cases suggest that FESS is not yet recognized in Italy as an alternative to traditional, but more invasive, techniques. This lack of knowledge about different approach routes limits its potential applicability only to soft disc herniation.
Uniportal endoscopic transforaminal endoscopy has the advantage of a virgin lateral access route that allows all the compression pathology to be reached from the recess/foraminal entry zone to the extraforaminal area, while minimizing the risk of cerebrospinal fluid leakage [18,31-33]. At the same time, some surgeons have also gained extensive experience in cases of severe foraminal stenosis and migrated disc herniation from L1 to S1 [34-36]. Yet, at conferences and meetings attended by authors, the interlaminar approach focused on soft disc herniation was presented the most. The transforaminal route and its applications in treating intra-/extraforaminal disc herniation and stenosis are sometimes disregarded, possibly because the interlaminar route resembles more of a mini-invasive tubular approach. Meanwhile, worldwide, indications for FESS are moving from mild degenerative spine conditions to nerve-sheath tumour removal and infection debridement [22,37,38]. From our perception, by analyzing the age of the respondents, it seems that experienced surgeons, except for a few ones (i.e., less than a third who are experts in the endoscopic field, 8.8% of responders), seem reluctant to shift to endoscopic surgery and, in this way, limiting access to younger colleagues and residents. This is due to a combination of factors as listed above. However, the small group of endoscopic surgeons who believe in the technique are trying to promote their knowledge through congresses, inviting surgeons for live training in their centers and publishing their case series.
The main limitation was the limited size of the sample, which makes it impossible to give an accurate assessment of the exact extent of the endoscopic phenomenon in Italy. The small number of responders also meant that we could not further stratify the analysis, sometimes resulting in a relatively shallow description of FESS dissemination and usage. However, a survey like this does not require a comparison or stratified analysis of the results. Still, describing the phenomenon in its starting phase is good enough to ask for an initial awareness of the endoscopic phenomenon. Furthermore, the survey should also be extended to neurosurgical and orthopedic residents in order to define the teaching status of endoscopy in Italy during residency. Despite these limitations, the survey covered a wide area of Italy, with a reasonable number of respondents, sufficient to reflect the current FESS phenomenon in Italy.
CONCLUSION
Our survey arose from a desire to understand the current limits of FESS dissemination in Italy and provide a starting point to boost the use of the technique as an extra tool in clinical practice, in particular to reduce anaesthesiological and surgical risk, with the same rate of complication as classic surgery. Our secondary aim was to provide young spine surgeons with a new field of knowledge that today can no longer be ignored.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.