INTRODUCTION
Low back pain and leg pain originated from a lumbosacral transitional vertebra (LSTV) known as Bertolotti’s syndrome (BS). It was first described by Mario Bertolotti in 1917 and it features an increase in size of unilateral or bilateral transverse process (TP) of the most caudal lumbar spine. In addition, it also forms pseudo-articulation or bony fusion between enlarged TP and the ala of sacrum [1].
While BS is not recognized enough in clinical practice by plenty of physicians, some reports suggest that it is not known to be a rare condition. There was a study that 35.6% as positive for a LSTV in 211 radiographs [2]. Moreover, it was reported that neural compression by LSTV was demonstrated in 13% of 74 patients whose transitional vertebrae were found in the report of MRI scan [3]. Despite the prevalence rate like those as several reports have shown, symptomatic patients who have BS often receive inadequate treatment, owing to misdiagnosis at an early stage [4,5].
Current operative techniques for treating BS are normally based on the procedure including decompression of L5 nerve root as well as resection of the pseudo-articulations or the part of TP which contact with ala of sacrum. In recent years, minimally invasive techniques have been reported by a large number of authors [6-9]. However, there are still only a few reports on percutaneous full endoscopic surgery for BS.
In recent years, endoscopic techniques for spinal surgery have been surprisingly developing and gradually replacing conventional surgical techniques. In line with this trend, we tried to perform a full endoscopy for treating BS and finally we have achieved a successful outcome in a case. This report offers a detailed description about the operative procedure and technical differences with full percutaneous endoscopy compared to other previous skills.
CASE DESCRIPTION
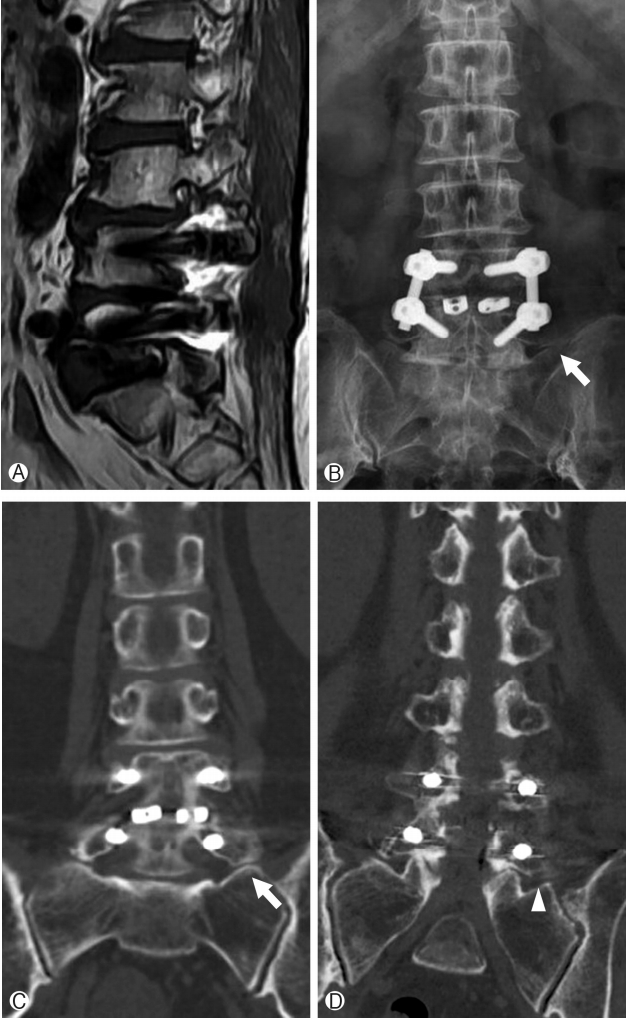
A 64-year-old woman with a few years history of left leg pain which got severely worsened a week ago visited at the spine center. In a neurologic examination, there was no abnormal sign such as decreased anal tone, muscle weakness or sensory change. The patient had already received numeral spine surgeries several years ago —decompressive ligamentectomy at L3-L4 and posterior lumbar interbody fusion at L4-L5 for spinal stenosis eight years earlier. In spite of those surgeries, she suffered from remained low back pain and radiating pain over the years. For that reason, she had received countless times of medial bundle branch block or facet block at lumbar spine. Furthermore, two years earlier from the visit, she had severe right leg pain and sought intra-discal electrothermal therapy for foraminal disc herniation at the right side of L5-S1. After she was examined by lumbar MRI scan in our institute, foraminal stenosis either L3-4 or L5-S1 at the left side (Fig. 1) was discovered. Because the stenosis at the L5-S1 seemed to be dominant rather than the one at the L3-4, a diagnostic lidocaine injection was selectively provided on the left L5 nerve root. Then the patient experienced temporary relief of leg pain. Thus, we were able to make a diagnosis that the left leg pain had been originated from the left foraminal stenosis of L5-S1 causing L5 radiculopathy. Before long the patient had a foraminotomy at the left foramen of L5-S1 by percutaneous full endoscopy using a uniportal spine endoscopic device. In that operation, the herniated disc on the foraminal side was resected by forcep along with intradiscal nucleus pulposus more inside, the ligaments which may compress nerve root were totally removed and the ipsilateral superior articular process was partially drilled out. Through all these procedures without any complications, we made sure that the left L5 nerve root had been totally decompressed by a skilled technique. However, despite the complete neural decompression, the patient still felt sustained leg pain. She complained that her leg pain had not improved at all. Soon, all the radiologic images were fully reviewed again to find out any other missed lesion since our initial diagnosis might have been wrong. Finally, on anteroposterior view from a simple radiograph of lumbar spine, we identified that the left TP of L5 vertebra seemed to contact with the ala of sacrum suggesting the BS. Thus we performed a pseudo-articularis lidocaine injection so as to exclude it. As a result, it turned out to be strongly effective in reducing leg pain. Then, we were able to make a definite diagnosis with BS for this patient. In a few days, she underwent a transverse processectomy by percutaneous full endoscopy using a uniportal spine endoscopic device. By a posterolateral approach, the left TP of L5 was simply cut at the base part of it. Consequently, any complications were not found during the surgical procedure. At last, the patient’s symptoms got relieved right after the surgery and she recovered in a few days.
OPERATIVE TECHNIQUE
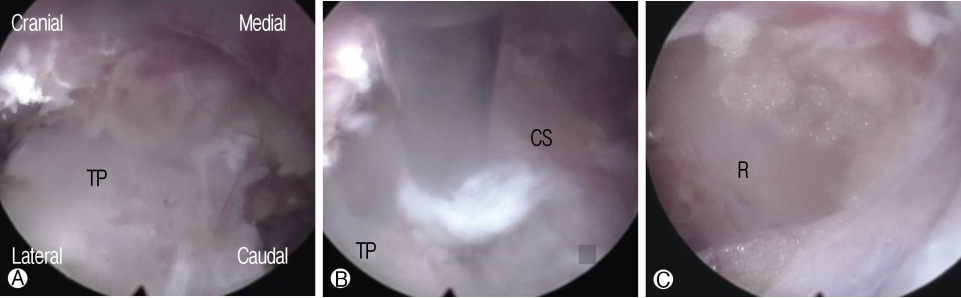
Firstly, under local anesthesia and C-arm visualization, the needle and guidewire were placed over the L5 TP. In the same manner, as a percutaneous endoscopic transforaminal lumbar discectomy, an obturator, a cannula, and a uniportal endoscopy were sequentially introduced to the L5 TP. By an endoscopic operative view, cranial and caudal margin at the base part of the TP were clearly identified. Secondly, the base of the L5 TP was simply cut in cranial to caudal direction using a high-speed drill. Thirdly, connective tissue and ligament on the anterior side of the TP were visualized which were dissected and removed by a forcep and a Kerrison punch. Upon that the L4 nerve root passing through the ventral side of TP and surrounded by fat tissue was visualized and we confirmed that it was free (Fig. 2). Moving the view of the endoscope to the caudal side, the L5nerve root traversing caudal to the TP was also identified and confirmed that it was free. After checking thoroughly, in the field of the endoscopic vision whether the TP of L5 was completely resected and the L4 and L5 nerve roots were free from neural compression, we finished the operation
DISCUSSION
LSTV is a congenital anomaly and has two types of abnormal vertebrae. The first type is that the L5 vertebra is fused with the S1 vertebra which called “sacralization of L5”. And the other one is that the S1 vertebra is separated from S2 without fusion which is called “lumbarization of S1” [10,11]. The features of the correlation between the TP of LSTV and the uppermost sacral bone may vary. They were classified into four types morphologically by Castellvi et al. [12]. According to whether they form a pseudo-articulation or bony fusion. Where the pain comes from in BS depends on how the LSTV and the sacrum forma intersegmental relationship according to those morphological types.
The mechanism that BS causes pain is diverse. Some studies indicated that it was caused by the degeneration of pseudo-articulation between a LSTV and an ala of sacrum [13-15]. It was also proved that the pain came from L5 nerve root entrapment by extraforaminal stenosis on account of enlarged TP of LSTV, called far out syndrome [16-19]. Disc degeneration above LSTV subsequent to BS was also reported as a possible cause of pain [11,20]. In addition, it was suggested that facet joint on the opposite side of the fused pseudo-articularis could cause pain [21,22]. As such, the pain of BS might occur in various lesions around the TP of LSTV and ala of sacrum. Therefore a definite differentiation to clarify whether the pain originated from has to precede surgery.
There are variable surgical techniques for symptomatic BS which is untreatable by conservative treatment. They consist of two main methods such as an intersegmental fusion between LSTV, sacrum and a resection of the pseudo-articulation. Santavirta et al. [23] reported clinical outcomes of patients who underwent posterolateral fusion for symptomatic BS. Their clinical results were only a moderate level, and problems were indicated about the second operation and adjacent segment degeneration. And the authors pointed out that the results with posterolateral fusion were only slightly better than those with conservative treatment in a comparable group. Whereas, many authors reported favorable results of technique to simply resect the pseudo-articulation or decompress entrapment of the L5 nerve root [6-8,13,24-26]. Some of them reported minimal invasive technique using a tubular retractor and suggested that it was recommended as an effective procedure. Additionally, Ko Ikuta et al. [6] applied a spinal endoscopy through the tubular retractor, and reported that it provided a well-illuminated operative field and surgical safety. It is true that those techniques were less invasive than pre-existing other conventional techniques. In fact, they are not able to be recognized as a true minimally invasive surgery. The first report introduced a percutaneous full endoscopic surgery for BS was given by Paudel et al. [27] in 2017. A uniportal spine endoscopic device was used without a tubular retractor to resect the pseudo-articulation and decompress the nerve root with a high-speed drill by direct dorsal or posterolateral approach. Then, they proposed this technique as an alternative treatment method in cases of symptomatic BS, as it preserves the iliolumbar ligament and provides early postoperative recovery compared to other existing techniques.
Meanwhile, in our institute, Ju et al. [28] reported somewhat unique surgical technique for BS in 2017. With a 2 cm skin incision and through the anatomic paraspinal intermuscular approach, the basal part of L5 TP and the ala of sacrum was exposed. Using a microscope, just cutting the base of TP was performed with a high-speed drill in cranial to caudal direction. This technique provides a permanent blocking the path of mechanical stress from the vertebrae to the pseudo-articulation via the TP, then it makes the pain in the pseudo-articulation get improved. This simple procedure has a few more advantages. Since articular surface of the pseudo-articulation which has to be resected by surgery usually has a relatively more irregular structure, just cutting the base of TP is much easier than the direct resection of pseudo-articulation. In addition, this method facilitates decompression of nerve roots. Just below the extension line of the TP incision line, the L5 nerve root can be identified and decompressed without difficulty. In particular, the author emphasized that L4 nerve root, as well as L5 nerve root, could be affected unexpectedly by the enlarged TP of LSTV. After cutting the base of TP and dissecting the connective tissue, then the L4 nerve root crossing down the ventral side of TP is able to be visualized and decompressed right away.
In this study, we attempted to implement the technique which is described above as a percutaneous full endoscopy on a patient diagnosed with BS. After the surgery, the patient was satisfied with the pain relief that had suffered over the years and no longer complained of low back pain and leg pain. Moreover, there were no postoperative complications. Consequently, our innovative technique worked successfully. In comparison with conventional methods, the percutaneous full endoscopic transverse proccessectomy provides that a few advantages-much less invasiveness, shorter operating time, less bleeding, and feasibility under local anesthesia. Overall, it was fully able to be performed almost the same procedure that was done by classical approaches.
CONCLUSION
BS is a diagnosis of exclusion. All patients who have L4 radiculopathy as well as L5 radiculopathy or axial pain should be doubtful about having BS. The pain origins around the LSTV and sacrum have to be precisely differentiated before surgery. Percutaneous full endoscopic surgery is feasible, effective and safe for BS. In conclusion, we expect that our findings could probably replace the other current surgical methods.