Full-endoscopic Intradiscal Surgery: State of the Art
Article information
Abstract
Two types of full-endoscopic intradiscal surgery have been described in the literature. The first is full-endoscopic thermal annuloplasty, which was introduced in 2004 for discogenic pain. The proposed pain generator is a high signal intensity zone or a toxic annular tear, which can be treated by full-endoscopic thermal annuloplasty using a bipolar radio-pulse device. The second is full-endoscopic disc cleaning surgery, which is more recent and has been used to treat intractable chronic low back pain due to type 1 Modic change. In this review, we describe the current status of full-endoscopic intradiscal surgery.
INTRODUCTION
The basic surgical treatment for spinal disorders is decompression and fusion. By the late 20th century, spine surgery had become less invasive with the introduction of the microscope [1] and micro-endoscope [2]. Now, early in this new century, the establishment of full-endoscopic spine surgery (FESS) [3,4] and subsequent refinement of the technique has made it possible to perform minimally invasive discectomy [5,6], decompression for stenosis [7-9], and trans-Kambin lumbar interbody fusion surgery [10,11].
More recently, FESS has been proposed as a surgical strategy for pain management. Three types of FESS for pain management have been reported, namely, rhizotomy [12,13], radio-pulse thermal annuloplasty [14,15], and disc cleaning [16]. In this review article, we focus on the current status of intradiscal FESS, which includes thermal annuloplasty and disc cleaning.
THERMAL ANNULOPLASTY
1. Surgical Indications
Thermal annuloplasty is indicated for discogenic low back pain. Two features can help us to clinically understand discogenic pain: a high-intensity zone (HIZ) and a toxic annular tear (TAT).
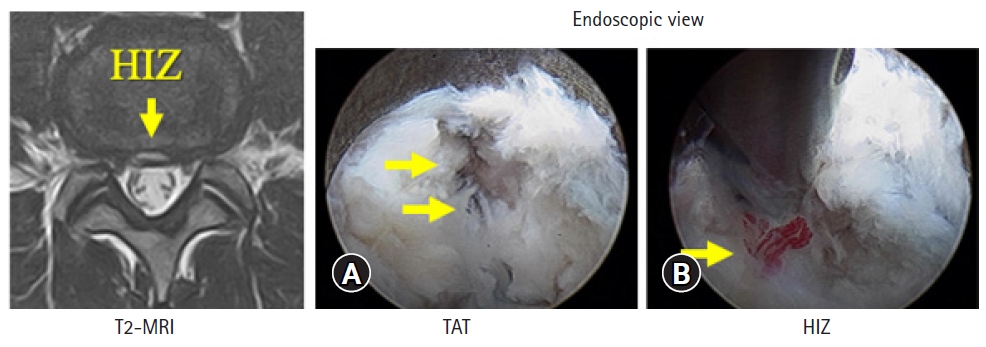
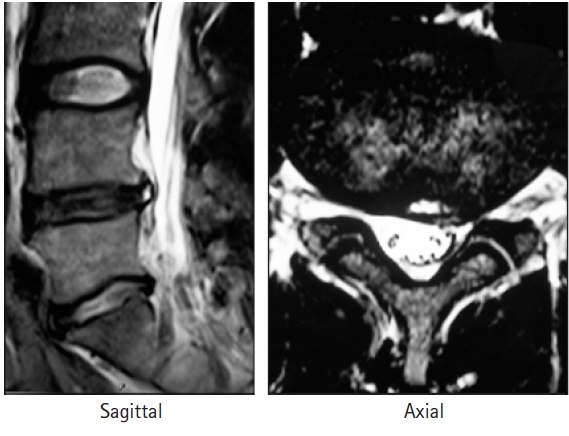
The HIZ is an area of high signal intensity at the posterior annulus seen on sagittal and axial T2-weighted magnetic resonance images (MRI) (Figure 1). It was first described in 1992 by Aprill and Bogduk [17], who found an 86% incidence of concordant painful discography in lumbar discs with an HIZ in patients with low back pain (LBP). They proposed a HIZ on MRI as a significant diagnostic sign of discogenic LBP. Figure 1 and 2 show representative cases of HIZ on MRI. Figure 1 shows the scans of a male professional baseball player who experienced severe LBP when playing. He was successfully treated by intradiscal injection for the pain. Figure 2 shows the scans of a female elite skier who was referred to us with severe LBP. Intradiscal injection relieved her pain and she was able to attend the subsequent Olympic games. Three years after the injection, although her disc degeneration had advanced, the HIZ was smaller and she had no LBP (Figure 2). There are several reports suggesting that an HIZ could be a marker of discogenic LBP [18-20]; however, its clinical significance remains controversial.
Sagittal and axial T2-weighted magnetic resonance images showing a high-intensity zone at the posterior annulus. The patient is a professional baseball player who experienced severe low back pain when playing. His pain was successfully treated by intradiscal injection.
Magnetic resonance images showing a high-intensity zone before and after intradiscal injection in a female elite skier and Olympian. Intradiscal injection was effective in decreasing the pain, and she was able to attend the next Olympic Games. Three years after the injection, although her disc degeneration had advanced, the high-intensity zone was smaller.
The TAT, named by Yeung [21], refers to an annular tear that is symptomatic. It is characterized by pain-sensitive granulation tissue within the tear. Bernard [22] investigated 250 patients with chronic LBP using both computed tomography (CT) discography and MRI and concluded that CT discography is more sensitive, especially for a painful annular tear with a normal disc on MRI. Discography continues to be a useful functional test for understanding discogenic pain. Manchikanti et al. [23] reviewed the role of discography in the diagnosis of discogenic LBP and found it to be useful for identifying a subset of patients with chronic LBP secondary to an intervertebral disc disorder.
2. Surgical Technique
Radio-pulse thermal annuloplasty is a surgical technique that was first performed by Tsou et al. [15]. It involves utilization of full-endoscopic discectomy [3-5]. A cannula is installed into the disc space under local anesthesia via the transforaminal approach. An outside-in foraminoplasty technique is used when the intervertebral foramen is narrow or there are concerns about exiting nerve root injury [24]. First, the area of the TAT is ablated using the bipolar radio-pulse device. The cannula is then advanced towards the posterior annulus to determine if there is an HIZ. Figure 3A shows the endoscopic view of a TAT. In Figure 3B, a vascularized disc fragment can be seen in the area showing an HIZ. After ablation of the TAT and HIZ, the radio-pulse thermal annuloplasty is completed.
3. Clinical Results
In the initial report by Tsou et al. [15], the outcome was excellent in 17 of 113 patients (15%) and good in 32 (28.3%). Therefore, only 43.3% of patients in their series has favorable results. On the other hand, Pan et al. [25] reviewed 62 consecutive patients who underwent thermal annuloplasty and reported an overall success rate of 75.8%. Ahn and Lee [26] reported a similar success rate of 70% and better clinical results in patients who also had central disc protrusion. Manabe et al. [14] reviewed 12 elite athletes who underwent radio-pulse thermal annuloplasty. Nine (75.0%) were found to have an HIZ at the level of the affected disc. The LBP disappeared soon after the surgery in 10 patients (83.3%), all of whom could returned to play within 3 months of surgery.
4. Representative Case
Figure 4 shows the preoperative MRI and CT discography findings in another male baseball player with a clinical diagnosis of chronic discogenic pain. MRI indicates disc degeneration at L4/5 and L5/S1. Slight HIZ is seen at L4/5 and a clear annular tear is evident at the same level. The patient’s LBP disappeared immediately after surgery. He has been very active in the ensuing season and has achieved his best performance to date.
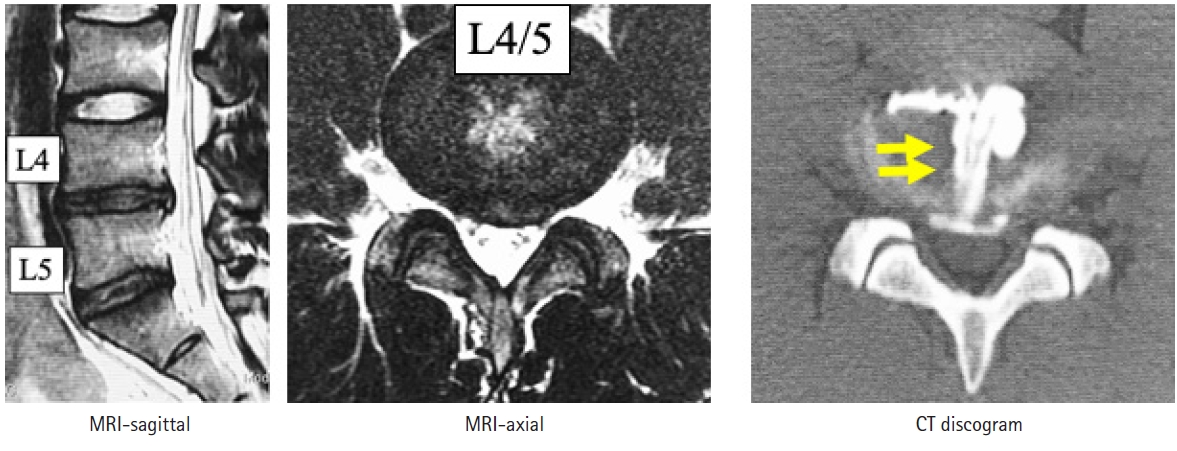
Findings on MRI and CT discography before thermal annuloplasty in a male baseball player with a clinical diagnosis of chronic discogenic pain. MRI shows disc degeneration at L4/5 and L5/S1. A slight high-intensity zone can be seen at L4/5 and a toxic annular tear is evident in the same level (arrows).
DISC CLEANING
1. Surgical Indication
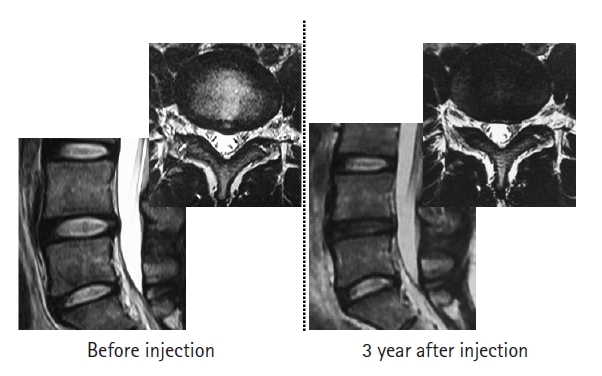
Disc cleaning is a recently reported technique and there is as yet no consensus about it in the literature. Based on the initial report by Sairyo et al. [16], disc cleaning is indicated for intractable chronic LBP due to type 1 Modic change. Of the three types of Modic change—type 1 (inflammation), type 2 (fatty marrow), and type 3 (bone sclerosis)—only type 1 is painful [27]. Intradiscal injection would be the non-surgical treatment for painful Modic type 1 change [28,29]. Figure 5 shows MRI scans obtained before and after intradiscal therapy in a former world martial arts champion. His LBP disappeared after a couple of intradiscal injections and MRI scans revealed conversion from type 1 to type 3 Modic change.
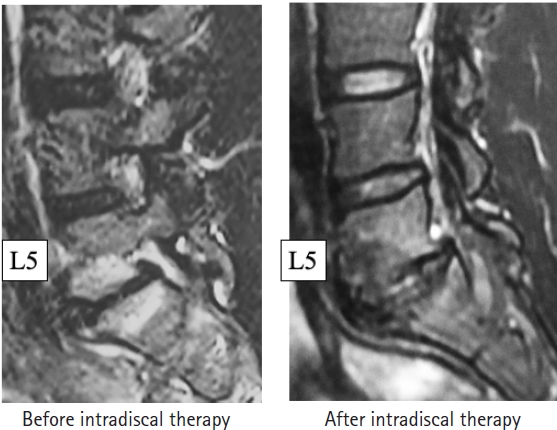
Short tau inversion recovery magnetic resonance images obtained before and after treatment for Modic change in a male martial arts fighter, who was a former world champion. Type 1 inflammation was clearly present before treatment but subsided following a couple of intradiscal injections. After intradiscal treatment, the Modic type was downgraded to type 3 sclerotic change.
Although fusion would be the gold standard surgical treatment for painful Modic change [30], full-endoscopic disc cleaning may be a new alternative for type 1 change.
2. Surgical Technique and Clinical Results
Full-endoscopic disc cleaning is another application of full-endoscopic discectomy [3-5]. Using either an outside-in or an inside-out technique, a cannula is inserted into the disc space, which normally contains cartilaginous tissue. However, a disc space with type 1 Modic change may contain fibrotic scar tissue instead [31]. This fibrous tissue should be removed and then be followed by copious irrigation and washing given that type 1 Modic change is thought to be caused by low-grade infection [32-36]. There have been two case reports in which disc cleaning was effective for alleviating LBP [16,31]. Kishima [37] reviewed his initial 10 cases of disc cleaning surgery for type 1 Modic change and found that the procedure was effective in 8 of them. Thus, it is necessary to clarify what kind of type 1 Modic change would be a good indication for disc cleaning.
3. Representative Case
Figure 6 shows short tau inversion recovery MRI scans obtained before and after disc cleaning surgery in a 37-year-old man with a history of severe LBP for more than a year. The preoperative image clearly suggests type 1 inflammation surrounding the L4 and L5 endplates. The image obtained 2 months after surgery shows a decrease in the high signal change, indicating that the inflammation has subsided. Clinically, the patient’s visual analog scale score for LBP when performing normal activities decreased from 8/10 to 1/10.
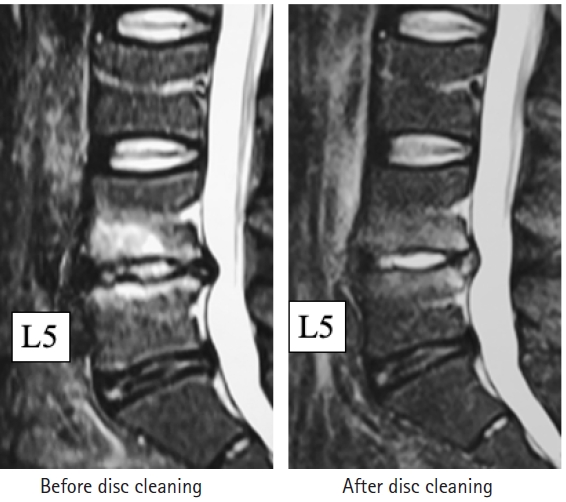
Short tau inversion recovery magnetic resonance images showing the effect of full-endoscopic disc cleaning surgery in a 37-year-old man. The image obtained before surgery clearly suggests type 1 change and another taken 2 months after surgery shows a decrease in the high signal change, indicating that the inflammation has subsided.
CONCLUSION
In this paper, we have reviewed two types of full-endoscopic intradiscal surgery. The gold standard worldwide for discogenic pain and type 1 Modic change is fusion surgery. However, full-endoscopic surgery could avoid the need for fusion and may surpass the present gold standard treatment. The clinical outcome is generally acceptable, although the exact indications for such surgery have yet to be confirmed.
Notes
No potential conflict of interest relevant to this article.