Comparative Study of the Outcomes of Unilateral Biportal Endoscopic Discectomy and Tubular Microdiscectomy Based on the Visual Analogue Scale, Oswestry Disability Index, and Short-form 36
Article information
Abstract
Objective
Unilateral biportal endoscopic (UBE) discectomy and tubular microdiscectomy (TMD) are widely practiced methods for treatment of lumbar disc herniation. Good clinical outcomes of these methods are reported in many papers, but there are a few comparative studies. This study reports the clinical outcomes of UBE and TMD as minimally invasive surgery methods for lumbar disc herniations and discusses the effectiveness of UBE.
Methods
Sixty-seven patients who had undergone single-level discectomy using one of two methods, UBE or TMD, underwent a prospective follow-up examination. Thirty-four of these patients underwent discectomy using UBE, and the remaining 33 patients underwent TMD. In addition to the traditional measures of outcome, the improvement of generic health-related quality of life and disease-specific measurements like Visual Analogue Scale (VAS) score, Short-form 36 (SF-36), and Oswestry Disability Index (ODI) were evaluated and compared.
Results
Sixty-seven patients with more than 6 months of post-operative follow-up evaluations were included. The mean improvements in the VAS scores for back pain and leg pain and ODI were 2.0, 3.7, and 26.5 for the UBE group and 1.6, 3.0, and 19.4 for the TMD group. The SF-36 physical health component subscale score improved from 35.4 pre-operatively to 54.8 at the last follow-up in the UBE group, and the mental health score improved from 43.5 to 55.1 (TMD group: from 34.9 to 54.3 and 44.2 to 57.1, respectively).
Conclusion
The clinical outcomes of the UBE group are comparable to those of the TMD group. The results indicate that UBE for lumbar disc herniation can be performed safely and effectively as a treatment modality.
INTRODUCTION
Lumbar microdiscectomy is a gold standard surgical procedure performed to relieve pain and improve neurological deficit. For decades, several minimally invasive spinal surgical techniques have been developed and they are considered an alternative to conventional open techniques [1]. The use of tubular retractors in conjunction with an operating microscope or endoscope has become popular throughout the world [2]. Through fixed or expandable retractors, physicians could use conventional microsurgical techniques of open surgery. Several randomized controlled trials have shown that tubular microdiscectomy is safe and effective compared to well-established traditional techniques.
After the concept of endoscopic spinal surgery became more popular, transforaminal percutaneous endoscopic lumbar discectomy (TELD) along with percutaneous endoscopic interlaminar discectomy (PEID) has been widely used for the treatment of lumbar disc herniation [3]. The development of the percutaneous endoscopic technique for lumbar disc disease represents an attempt to improve the operating efficacy, reduce the post-operative pain, limit the length of the patient’s hospitalization, reduce perineural fibrosis, and minimize the development of spinal instability [4,5]. However, restricted space and uncomfortable manipulation have limited their effectiveness [6].
Unilateral biportal endoscopy (UBE)-assisted discectomy was recently introduced, and it combines the advantages of endoscopic spinal surgery and conventional spinal surgery. The technique has shown favorable results for treatment of lumbar disc herniation in many previous reports. Most previous studies used perioperative parameters (blood loss, hospital stay, operative time) and qualitative scales (e.g., the modified Macnab criteria and the Odom scale) which are surgeon-based outcomes. They showed good-to-excellent clinical outcomes relevant to improvement in disease-related symptoms after UBE discectomy. However, it is also important to measure patient view of their health-related quality of life, like SF-36. The disease specific measurement like ODI would be also helpful to evaluate the effectiveness of the procedure. To knowledge of authors no prospective study that compared the effectiveness of tubular microdiscectomy and unilateral biportal endoscopic discectomy using all the parameters above has been previously conducted.
In this study, the clinical outcomes of UBE discectomy are compared with those of microscopic discectomy using a tubular retractor; VAS, ODI, SF-36, and perioperative parameters were collected prospectively.
MATERIALS AND METHODS
1. Patient Population
This study was approved by Institutional Review Board of Daegu Catholic University Medical Center (IRB No. CR-22-065). This is a prospective clinical study that involves 67 patients who had undergone single-level discectomy in our department. The patients were divided into two groups by surgical method: 33 patients underwent tubular microdiscectomy (TMD) (Group I), and 34 patients underwent UBE-assisted discectomy (Group II). The inclusion criteria were (1) general symptoms of lumbar radiculopathy, (2) no improvement after conservative treatment for 6–8 weeks, (3) single-level pathologic lesion with no previous back surgery at the same level, (4) no segmental instability in the dynamic flexion-extension radiographs, and (5) documented pre- and post-operative evaluation for at least 6 months. Patients who had a severe neurologic deficit or spinal instability that required fusion and other pathologic conditions, such as fractures, tumors, or infections, were excluded from this study (Table 1).
2. Clinical Evaluation and Follow-up
Patient data on back pain, radiating pain, motor deficit, sensory deficit, reflex deficit, and bowel/bladder dysfunction pre-operatively and at the post-operative office visits were analyzed prospectively. Follow-up examinations were conducted 6 weeks, 3 months, 6 months, 12 months, and then annually after the operation. In addition to a general examination, other information was obtained using the following parameters: VAS scores for back pain and leg pain, ODI for condition-specific measurement, and Short-form 36 (SF-36) for the quality of life, mean blood loss, mean operative time, and length of hospital stay time. All surgeries were performed by 1 surgeon, to eliminate the risk of minor variations in clinical outcomes due to the surgeon’s technique and expertise. The result of last follow-up had been analyzed. If a patient was not followed up at the authors’ institution, he or she reported the results to the authors post-operatively via a mail survey.
3. Statistical Analysis
Statistical analysis was performed with SPSS version 25.0. A paired sample t-test was used to compare the differences between the pre- and post-operative parameters of the clinical outcomes for each group. The independent two-sample t-test and chi-square test were used to compare the differences between the clinical results of the two groups. A p-value less than 0.05 was considered statistically significant.
4. Surgical Techniques
In the TMD group, all procedures were performed under general anesthesia in the prone position on a radiolucent table. After creating a 2.5 cm skin incision, the paravertebral muscles were dissected using a serial dilator. The operating field was exposed using a tubular retractor. Under microscopic view, partial hemilaminectomy and targeted fragmentectomy with discectomy were performed with retraction of the nerve root. After thorough decompression of the nerve root and the thecal sac, closure was performed conventionally.
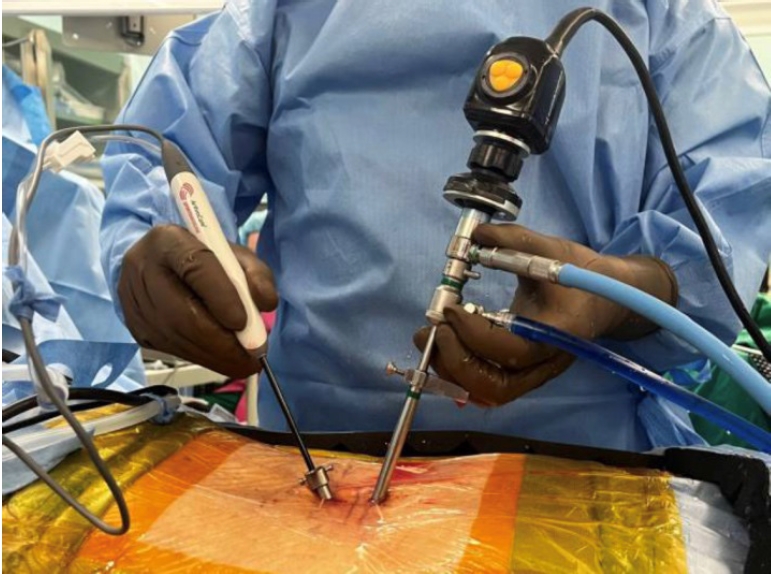
In the UBE group, all procedures were performed under general anesthesia in the prone position on a radiolucent table. The target pathological disc level was identified under fluoroscopic guidance. A waterproof surgical drape was applied after anesthesia was induced. Two skin incisions were made 1–1.5 cm lateral to the midline. Two portals were used: one for continuous irrigation and endoscopic viewing and the other portal for insertion and manipulation of the instruments used in the decompression procedures (Figure 1). The soft tissue was endoscopically cauterized with radiofrequency ablation to create working space. Next, the spinolaminar junction at the target intervertebral site was identified, a partial laminotomy was performed, and parts of the inferior lamina of the upper lumbar spine and superior lamina of the lower lumbar spine were removed using an electric drill. The interlaminar ligament was dissected and removed using a Kerrison punch and radiofrequency probe, followed by dissection and exposure of the annulus of the protruding intervertebral disc. The ruptured fragments were removed, and decompression of the nerve root and pulsation of the dura mater were confirmed. A drain was then inserted, and the surgical incision was closed.
RESULTS
1. Baseline Characteristics
Data from 67 patients (33 in the TMD group and 34 in the UBE group) were included in the follow-up data, spanning at least 6 months post-operatively. In the TMD group (Group I), there were 20 men and 13 women, and their mean age was 57.6 years (range, 15–77 years). The mean duration of radiculopathy was 4.7 months, and their mean post-operative follow-up period was 20.1 months (range, 6–40 months). Forty-eight percent (16/33) of the patients experienced back pain post-operatively, 100% of patients (33/33) experienced radiating pain; 88% of patients (29/33) experienced motor deficit, 70% of patients (23/33) experienced sensory deficit, and 6% of patients (2/33) experienced bowel/bladder dysfunction (Table 1).
In the UBE group (Group II), 19 men and 15 women underwent UBE-assisted discectomy. Their mean age, duration of radiculopathy, and mean post-operative follow-up duration were 54.9 years (range, 23–80 years), 5.2 months, and 9.3 months (range, 6–33 months), respectively. Clinical symptoms of back pain, radiating pain, motor deficit, and sensory deficit were noted in 75% (25/34), 100% (34/34), 97% (33/34), and 59% (20/34) of patients, respectively. There was no bowel/bladder dysfunction or reflex deficit pre-operatively. The most common symptom was radiating pain in the leg, and the most affected level was L4-5 in both groups (Table 1).
2. Clinical Outcomes
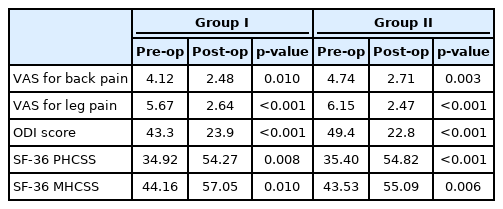
Measured pre-operatively and at the last post-operative office visit, the mean VAS regarding pain discomfort scores for back pain were 4.12 and 2.48, respectively, in Group I and 4.74 and 2.71 in Group II. The mean improvements in the VAS scores for back pain were statistically significant in both groups (p=0.010 and 0.003), but the differences between the two groups were not significant. The mean pre-operative and post-operative VAS scores for leg pain were 5.67 and 2.64, respectively, in Group I and 6.15 and 2.47 in Group II. The mean improvements in the VAS scores for leg pain were statistically significant in both groups (p<0.001 and p<0.001), but differences between the two groups were not statistically significant. The mean ODI scores recorded pre-operatively and at the last follow-up were 43.33 and 23.9, respectively, in Group I and 49.35 and 22.8 in Group II. The mean improvements in ODI scores were statistically significant in both groups (p<0.001 and p<0.001), but differences between the two groups were not statistically significant. The mean SF-36 physical health component scales recorded pre-operatively and at the last follow-up were 34.9 and 54.3, respectively, in Group I and 35.4 and 54.8 in Group II. The mean improvements in the SF-36 physical health component scales were statistically significant in both groups (p=0.008 and p<0.001), but differences between the two groups were not statistically significant. The mean SF-36 mental health component scales recorded pre-operatively and at the last follow-up were 44.2 and 57.1, respectively, in Group I and 43.5 and 55.1 in Group II. The mean improvements in the SF-36 mental health component scales were statistically significant in both groups (p=0.010 and 0.006), but there were no significant differences between the two groups (Table 2, Figure 2).
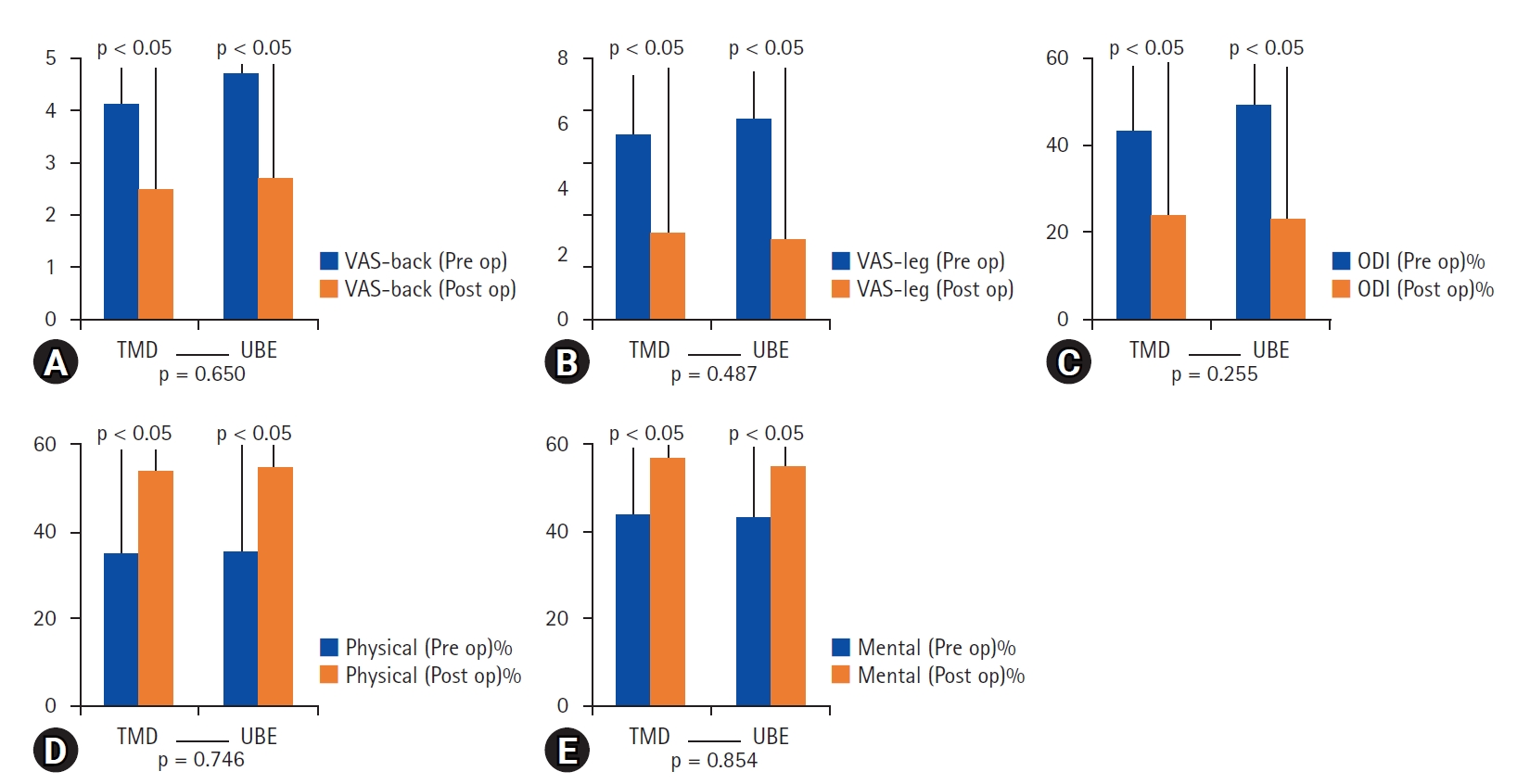
Comparison of clinical outcomes between tubular microdiscectomy and unilateral biportal endoscopic discectomy. (A) Visual Analogue Scale (VAS) score for back pain, (B) VAS score for leg pain, (C) Oswestry Disability Index, (D) Physical health component subscale score, and (E) Mental health component subscale score.
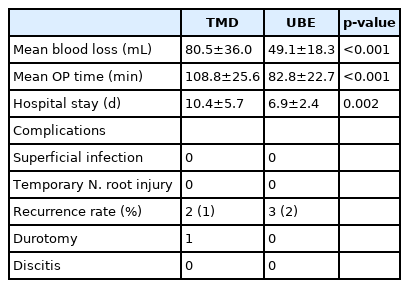
The mean blood loss was 80.5 mL in Group I and 49.1 mL in Group II, significantly lower in Group II than in Group I (p<0.001). The mean operative times were 108.8 minutes in Group I and 82.8 minutes in Group II, significantly shorter in Group II than in Group I (p<0.001). The mean hospital stay was significantly shorter in Group II than in Group I (p=0.002) (Table 3).
Complications occurred in 3 patients in Group I and 3 patients in Group II. Recurrence of herniation at the same level and at the ipsilateral side required reoperations in 1 and 2 patients, respectively, over both groups. Dural tear, which occurred in 1 patient in Group I, presented no neurologic deficit and was successfully managed after 48 hours of bed rest.
DISCUSSION
Conventional microdiscectomy remains the gold standard for lumbar intervertebral disc herniation. However, conventional open lumbar microdiscectomy would inevitably disrupt the posterior paraspinal muscles and lead to long-term muscle atrophy and chronic back pain [7,8]. Therefore, minimally invasive spine surgery (MISS) has been developed to avoid them, with the progress of technology.
With the integration of the microscope and tubular system, the MISS with tubular retractor gained popularity with minimally invasive spine surgeons, and numerous reports emerged for lumbar microdiscectomy. On the other hand, TELD along with PEID has a less invasive modality, and several advantages over other forms of MIS: it more extensively preserves normal paraspinal structures during surgery, reduces post-operative pain to allow early discharge, and can be performed under local anesthesia [5,9]. However, the uniportal system uses combined channel (viewing and instrumental) that limits the independent movement of instruments. Furthermore, although it can remove soft disc herniation and ruptured disc materials without foraminal obstruction, restricted movements of the instruments and obstructed intervertebral foramen following degenerative changes could disturb the procedure [1,3].
The UBE technique was first described by Soliman [10] as irrigation endoscopic discectomy (IED) in 2013 and by Eum et al. [11] as percutaneous biportal endoscopic decompression (PBED) in 2016 and was reported to be feasible for lumbar spinal surgery, including lumbar fusion, by many authors in the following years [1,12,13]. The advantages of UBE are increased surgical movement of the instruments with independent visualization and working portals, good and wide field of visualization conferring unrestricted access to contralateral and foraminal areas, less bleeding because of continuous irrigation, visual similarity between the surgical field and that of conventional microscopic surgery, and a reduced armamentarium because the UBE system uses separated channel for instruments and only 0° or 30° arthroscopy for the knees or shoulders are used for standard laminectomy.
A systematic review of UBE spinal surgery collected 556 patients and 679 levels from the selected 11 studies in 2019 by Lin et al. [1] They concluded that UBE may be a feasible option for lumbar spinal surgery. However, the existing studies were limited to small cohorts and short-term follow up.
Kim et al. [12] reported a comparative study of clinical outcomes of single-lumbar discectomy using UBE and open lumbar microdiscectomy (OLM). This study showed superiority in terms of short-term back pain recovery, a small volume of intraoperative blood loss, and less hospital stay. On the other hand, improvements in short-term leg pain and long-term back and leg pain, modification of the quality of life (ODI), patient satisfaction (modified MacNab score), and complication rate were similar to that of OLM. They were satisfied with the result because despite the statistically significant prolonged operation time, patient satisfaction was equivalent to conventional open procedure. That would be due to the tissue-sparing nature of the procedure, rapid pain recovery, short hospital stay, favorable pain outcomes, and improved quality of life.
Aygun and Abdulshafi [14] reported a prospective clinical study comparing UBE and tubular microendoscopy in the management of single-level degenerative lumbar canal stenosis. Their study was conducted to test the feasibility of the UBE technique in management of lumbar canal stenosis using ODI, Zurich Claudication Questionnaire (ZCQ), and Modified MacNab Criteria (MMC). In this study, UBE cases had statistically superior results in ODI and ZCQ scores that represents the superiority of UBE over tubular microendoscopy in management of single degenerative lumbar canal stenosis. They thought that tubular microendoscopy has its limitations attributable to changing the working cannula direction, narrow visualization field, difficulty in bleeding control, and inadequate achievement of contralateral neural decompression. In contrast, UBE provided a clear visualization of neural elements, degenerative surrounding structures, and congested epidural venous plexus, which are crucial for achieving the best operative results.
According to the study above, we expected that UBE-assisted discectomy would have superior results in disease specific measurement and patients HRQOL measurement compared to tubular microdiscectomy. Therefore, this study focused on comparing the clinical outcomes of UBE-assisted discectomy and TMD as pain scales by VAS, disability-related outcome scales by ODI, and health-related quality of life scales by SF-36 [15].
The ODI questionnaire was published in 1980 by Fairbank et al. [16]. This questionnaire is widely used for patients with lumbar spinal pain due to its disease-specific nature and convenience [15]. Various outcome questionnaires have been developed to assess the impact on patient quality of life. The goal of these questionnaires is to measure patients’ views of their health and daily activities. Health-related quality of life refers to the effects of a patient’s health on his/her overall well-being [17]. The most commonly used generic health-related quality of life survey is the SF-36 [15,18].
FDA standards for good-to-excellent operative outcomes include a 15-point improvement in ODI plus maintenance or improvement in SF-36 score [19]. In our study, significant improvements in VAS scores for back pain and leg pain, ODI, and SF-36 across both physical and mental component subscales were achieved in both UBE and TMD groups. The mean decrease in ODI scores was 19.4 and 26.5 in Group I and II, respectively, at the final follow-up, with improvement of SF-36 score. This result could be interpreted as a significant improvement in the quality of life of the patients in both groups.
However, statistical difference between two procedures was not significant in VAS, ODI, and SF-36. Unlike the previous study of Kim et al. [12], the operative time was even shorter in UBE compared to TMD. There would be several reasons for the result. Firstly, tubular microdiscectomy would be less destructive than conventional discectomy. The paraspinal approach would maintain multifidus tendon attachment to the spinous process and integrity of dorsolumbar fascia and avoid injury to the posterior paraspinal muscles. Also, the tubular retractor is a “non self-retaining” system, which reduces the pressure on the tissues for holding the retractor in place. Furthermore, a tubular retractor maximizes the surface contact area which minimizes the pressure per unit area. Secondly, unlike the report of Aygun et al. [14] which was about decompression surgery, tubular microdiscectomy does not need to change the working direction of tubular retractor and it would result in less damage to posterior paraspinal muscles.
Choi et al. [20] compared the surgical invasiveness of lumbar microdiscectomy and UBE discectomy using differences in creatine phosphokinase (CPK), C-reactive protein (CRP), and MRI before and after surgery. The study showed significantly lower CPK, CRP, and MRI change in the UBE discectomy group, which indicates that there was less muscle injury following UBE discectomy than microdiscectomy, which eventually affects hospital stay duration and post-operative back pain in the early stages. In the present study, perioperative parameters of mean blood loss, mean operation time, and hospital day were significantly superior in the UBE group. The reduction of blood loss and operation time might have led to less tissue injury, resulting in reduction of hospital stay time in the UBE group. Immediate post-operative back pain data were not collected in this study, but the UBE group tended to require a lesser opioid dosage than the TMD group.
The limitations of this study is that it was nonrandomized nature, small size, and variant duration of follow up period due to the transitional period of surgical methods from TMD- to UBE-assisted discectomy in the authors’ department. However, the results show that UBE is a safe and effective procedure, compared with well-established minimally invasive technique. Adequate randomized prospective studies for UBE are required to verify the present study.
CONCLUSION
The outcomes of UBE-assisted discectomy, including VAS, ODI, and SF-36, are comparable to those of TMD. Meanwhile, the UBE technique has some advantages regarding blood loss, operation time, and hospital stay. Therefore, UBE can be considered an alternative surgical option as an MIS technique.
Notes
Ethical statements
This study was approved by Institutional Review Board of Daegu Catholic University Medical Center (IRB No. CR-22-065).
Conflicts of interest
No potential conflict of interest relevant to this article.