Endoscopic Approach for A Difficult Cervical Area: Fully Endoscopic Uniportal Transcervical Approach for Ventral Pathologies of the Craniovertebral Junction
Article information
Abstract
Objective
Various pathologies can occur at the craniovertebral junction (CVJ). Posterior decompression with occipitocervical fixation can improve many of these conditions, but anterior decompression is required in some cases. Anterior decompression of a CVJ lesion is very difficult to perform. The transoral approach has been considered the gold standard, but it has the disadvantage of a deep and limited operative field, and many complications are associated with this procedure. Three endoscopic approaches (transoral, transnasal, and transcervical) have been reported previously. Transcervical endoscopic odontoidectomy is a familiar approach for spinal surgeons and can be performed using a uniportal full-endoscopic spinal surgery system.
Methods
As described in the present study, 12 patients underwent surgery, and their clinical records were reviewed retrospectively.
Results
All patients had good recovery without complications.
Conclusion
Fully endoscopic uniportal transcervical odontoidectomy has many advantages for ventral pathologies of the CVJ. In particular, it can avoid heat injury despite drilling very close to the brainstem in deep closed lesions.
INTRODUCTION
The craniovertebral junction (CVJ) is one of the most complex cervical areas. Decompression of this area is difficult, and consensus on the surgical methods is yet to be reached. The open transoral approach has for long been the only technique for ventral pathologies at the CVJ, but other minimally invasive techniques have been developed. Endoscopic procedures are especially common in this field. In particular, Full-endoscopic uniportal transcervical endoscopic odontoidectomy is a highly useful method, and we report this surgical method compared to other surgical treatments.
MATERIALS AND MEYHODS
1. Indication
The surgical strategies vary depending on the pathology. Pseudotumors usually increase in size in the presence of CVJ instability or overload. Therefore, recurrence may occur after direct anterior decompression. Transcervical odontoidectomy is indicated in cases in which posterior decompression and fixation are performed; however, a decrease in the pseudotumor size is not observed. In the case of bony compression, such as a basilar impression, transcervical odontoidectomy is indicated when symptoms cannot be improved via posterior decompression and fixation. Bony compression, which does not require fixation, is also indicated.
2. Surgical Procedures
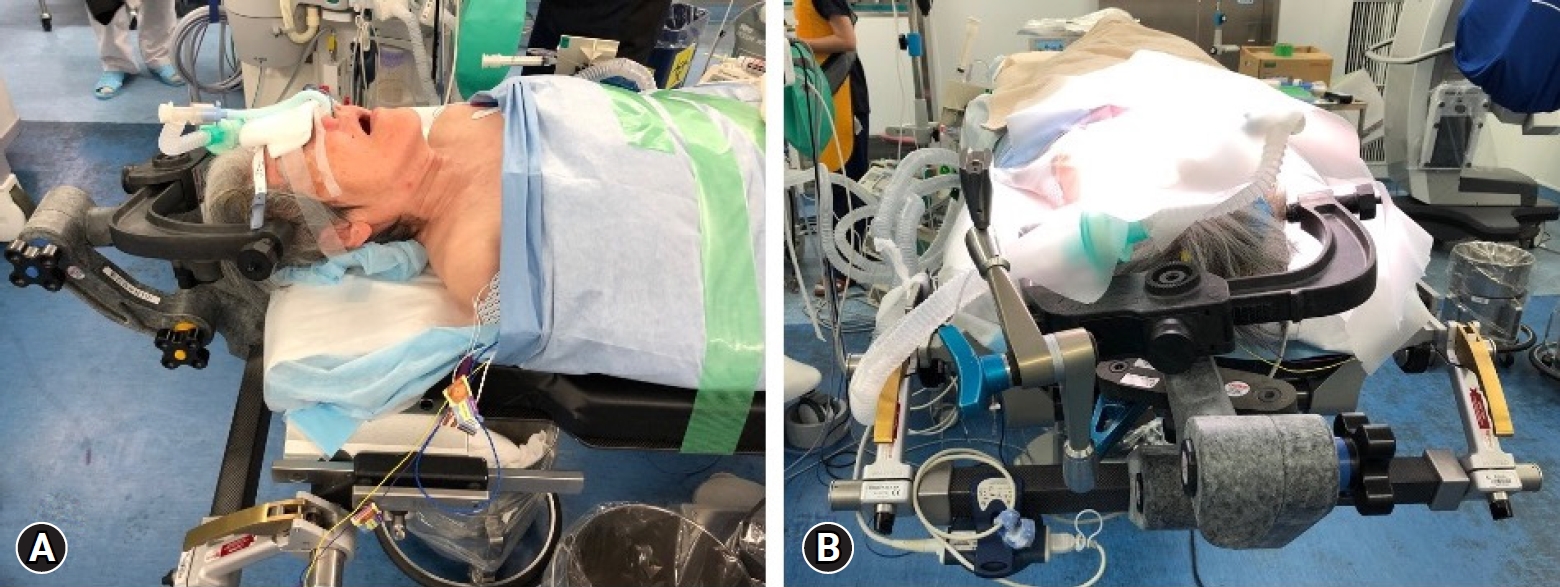
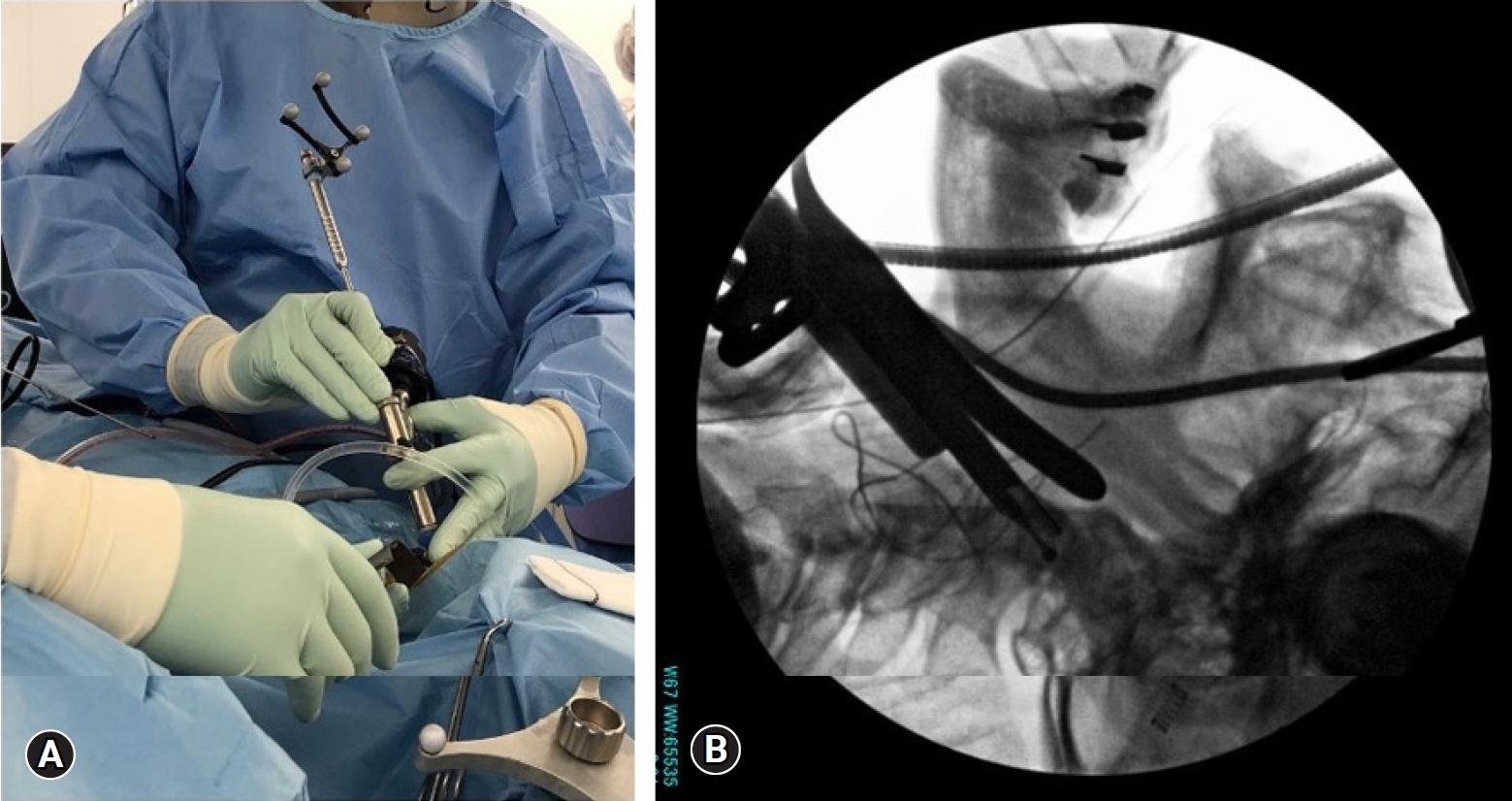
1) Anesthesia and Patient Position
The patient was placed in the supine position under general anesthesia (Figure 1A). In this position, it is easier to manipulate the endoscope during transnasal intubation. The head was fixed by a Mayfield head clump. When a patient has posterior occipitocervical fixation (OCF), the neck should be in a neutral position. The neck position of the patient without a previous OCF should be slightly extended.
2) Preoperative Procedures
Biplane fluoroscopy is sufficient to confirm the intraoperative orientation; however, a navigation system with intraoperative corn-beam CT is quite useful (Figure 1B). The navigation reference was attached to a Mayfield head clump. We used a lateral fluoroscope and navigation system simultaneously.
3) Skin Incision and Insertion of Endoscope
A 4-cm transvers linear skin incision was made on the right side of the anterior cervical, which position was majored by preoperative radiography, depending on the insertion angle of the endoscopic approach. The ventral surface of C2 to the subaxial vertebrae was exposed, as in the open anterior cervical approach. A single-port endoscope was inserted through an open-skin incision.
(1) Surgical procedures
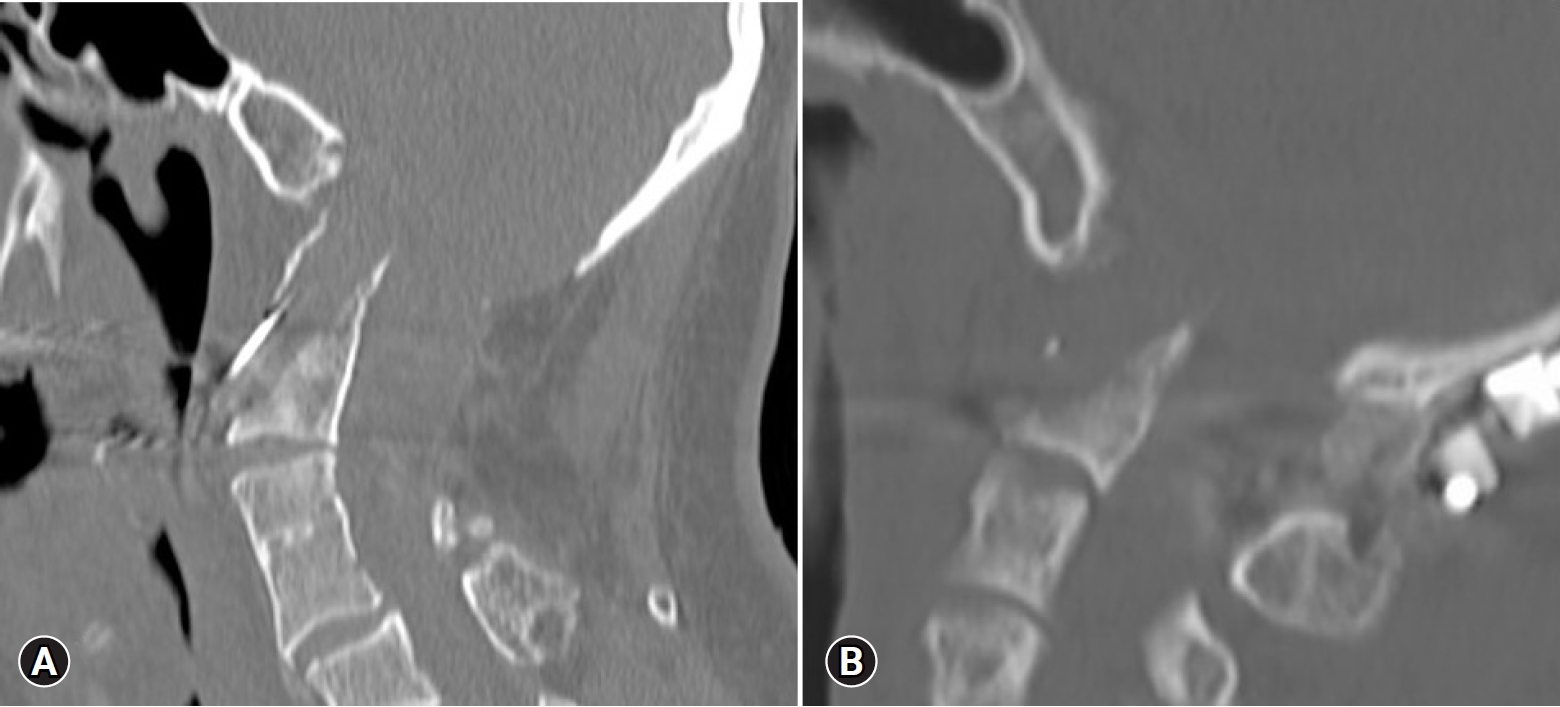
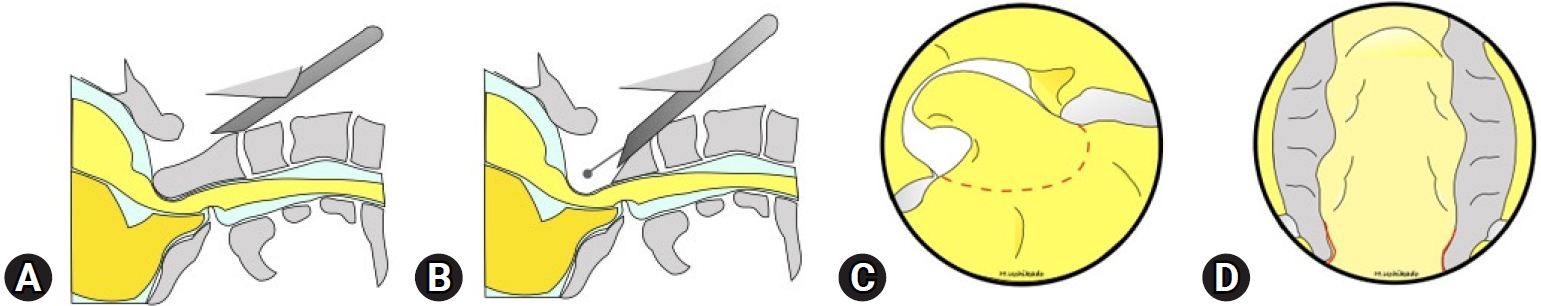
There are two strategies that depend on the decompression area: partial and total odontoidectomy (Figure 2).
(2) Partial odontoidectomy
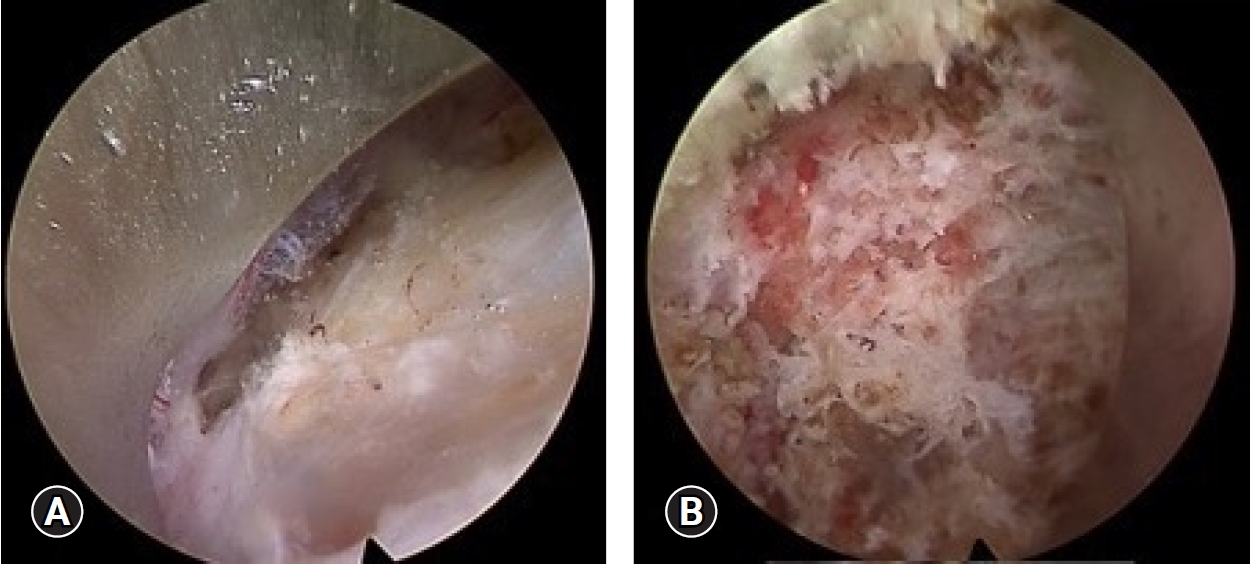
This strategy is for cases with pseudotumors or compression by the odontoid tip or dorsal wall (Figure 3). The starting point of drilling was the midline just above the C2/3 disc space (Figure 4A). After making an 8-mm hole to insert the outer sheath, the cancerous bone was drilled by rotation of the outer sheath (Figure 4B) and an electrical drill under direct endoscopic view and biplane fluoroscopy (navigation is helpful in this procedure). The cortical bone (dorsal wall of the dens) was then recognized. The selected area that was planned preoperatively was drilled to decompress under a lateral fluoroscope. The pseudotumor was located behind the transverse ligament. For patients with pseudotumors, the odontoid tip was drilled to the dorsal wall of the dens. Yellowish connective tissue, like hypertrophied yellow ligament, was found behind the dens. Decompression of the soft tissue, including the cyst, was performed. After complete hemostasis, a drain tube was inserted into the dens, and the wound was closed in the usual manner.
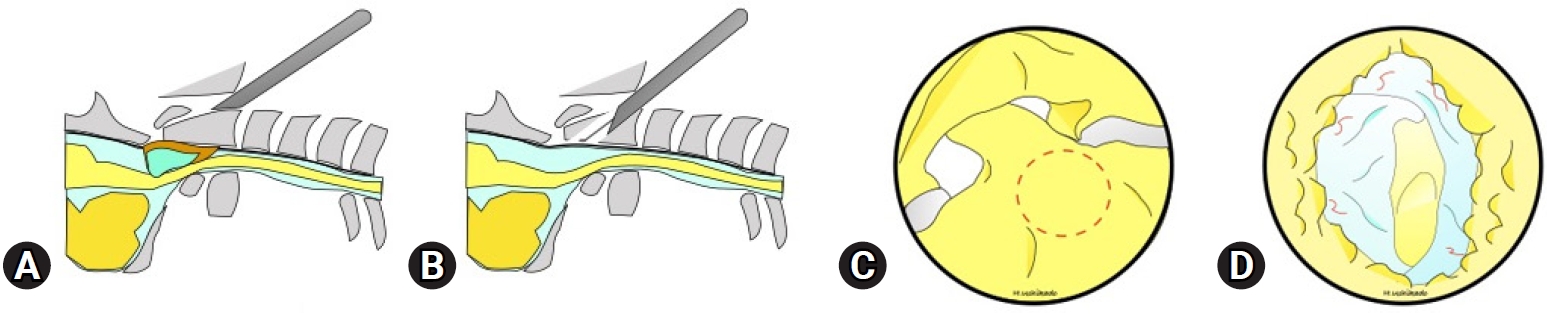
(A, B) Schema of the lateral view. (C) Drilling area. (D) After cyst resection. Pulsation of the soft tissue was confirmed.
(3) Total odontoidectomy
The first bilateral edge of the dens was confirmed. Drilling was started at the base of the dens. The decompression area was examined using a lateral fluoroscope (Figure 5). The caudal end of the clivus was confirmed after a complete resection. We do not cut tectal membrane or posterior longitudinal ligament to decompress to expose dura matter. A drain tube was inserted, and the wound was closed.
(4) Final checking point
After decompression, soft tissue pulsation was recognized. Decompression area was confirmed by direct tactile perception (Figure 6). The decompression area was also confirmed using a biplane fluoroscope or navigation system (Figure 7). Corn-beam CT is also useful for confirming the decompression.
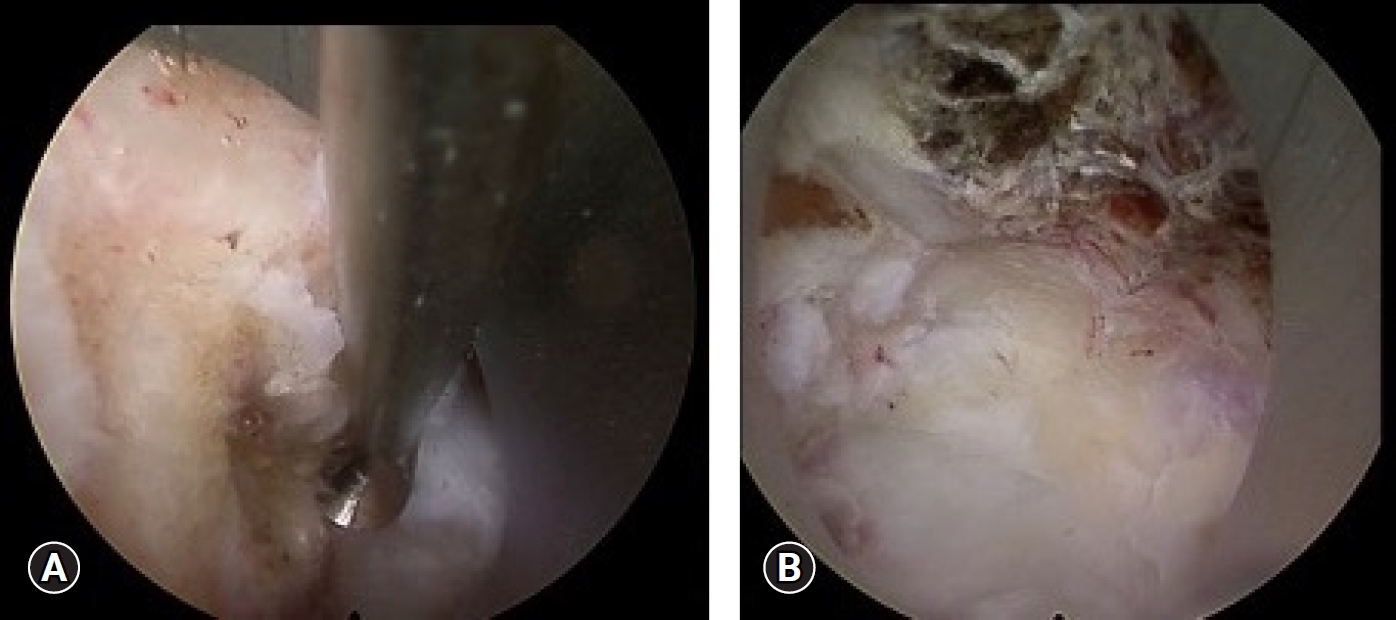
Intraoperative views step by step. (A) The right side of the bone edge was confirmed directly by a curved curette. (B) The odontoid tip and dorsal wall of the dens were resected.
RESULTS
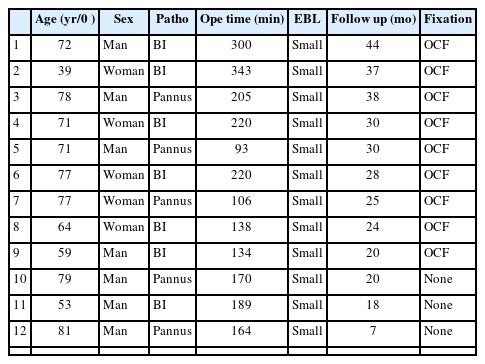
Twelve patients were operated on using transcervical endoscopic odontoidectomy (Table 1): seven cases of basilar impression (BI) and five cases of pseudotumor (cases 1–3 were reported in a previous case report [1]). There were seven men and five women (men/women=3/4 in BI, 4/1 in pannus). The mean age was 62.3 (39–77) years and 77.2 (71–81) years, respectively. Nine patients underwent surgery after OCF, and three patients did not undergo OCF. The mean operative time was 190.2 min (189 min in BI and 147.6 min in pseudotumor). Extra blood loss was not significant, and no complications were observed in all cases. All patients showed improvements in myelopathy and brainstem symptoms after surgery. Additional OCF was required in Case 12 because of pseudotumor recurrence. This patient rejected OCF first and wanted to undergo only decompression surgery but finally accepted OCF during the second surgery.
DISCUSSION
Reumatoid arthritis (RA) and its anomalies are the main pathologies of brainstem dysfunction at the CVJ. The pseudotumor increased not only the instability of the CVJ but also the overload at the CVJ caused by the stiffness of the subaxial cervical spine. Usually, compression pathologies at the CVJ arise from the anterior region, but many cases improve after posterior decompression and fixation [2]. Some cases required odontoidectomy after the posterior procedure, and the gold standard of ventral decompression at the CVJ, open transoral approach, was considered. Many authors have reported the disadvantages of the transoral approach [3], which include a limited operative view and a deep working distance. In addition, the transoral approach is associated with several risks, such as contamination by normal oral flora, dehiscence of the surgical wound, alteration in phonation, tongue edema, the potential need for prolonged intubation or tracheostomy, the requirement of avoiding oral intake, and postoperative enteral tube feeding.
Three approaches to endoscopic odontoidectomy have been proposed to resolve these complications of transoral approach [4]. First, the transoral endoscopic approach is useful for vertical long mass lesions at the CVJ to below C2 [5,6]; however, it cannot control the contamination of the oral flora. Second, the transnasal endoscopic approach [4,7-9], which was initiated by a skull base surgeon, allows many instruments to be used in large natural anatomical cavities, but the caudal view is limited. The third method is the transcervical approach and was first reported in endoscopic-assisted surgery using the METREX system [10]. Wolinsky et al. [10] reported many advantages of this approach: spine surgeons are familiar with the technique, it does not require traversing the oral mucosa, the deepest basilar invaginations can be decompressed because their trajectory is parallel to the odontoid itself, and it does not require resection of anterior arch of atlas. The transcervical approach has disadvantages that are almost the same as those of the anterior cervical open procedure. Odontoidectomy under full endoscopic spinal surgery was reported by Ruetten et al. [11]. They referred to this technique as “full-endoscopic uniportal technique using retropharyngeal approach.” They reported three papers on this approach [11-13], and another author reported a case series of the same procedure [1]. These studies mentioned that the merit of this technique is its large working area. The caudal limitation of mobility is in the lower jaw, and transnasal intubation is helpful. Occasionally, cranial limitations are encountered in patients with barrel chest. Resection of the C1 anterior arch is useful in solving this problem. Expected complications are almost the same as those of open anterior cervical approach, such as the original transcervical odontoidectomy using METREX system by Wolinsky et al. [10].
In addition to familiarity to spine surgeons, transcervical has many advantages compared to other decompression procedures. Complications associated with the anterior cervical approach are easily imaged and avoided. The decompression area can be selected depending on the pathology of each patient in this approach. Some patients, such as those with BIs, require total odontoidectomy, but not all patients require total odontoidectomy. If the anterior arch of C1, the anterior wall, and part of the lateral wall of the dens are preserved, the risk of instability at C1/2 might be decreased. Heat injury might occur by drilling deep-sheeted lesions. The uniportal endoscope provided a closed, clear view under saline irrigation. Continuous saline irrigation helps with cooling. This system is the most suitable instrumentation for deep closed site drilling.
No complications were observed in this case series; however, the number of cases in this study was small. Cases with ventral pathologies are very rare, especially those that cannot be improved by posterior decompression and fixation. Further studies are required to determine the efficacy and safety of this approach.
CONCLUSION
Pathologies of the CVJ are usually treated using the posterior approach. However, some cases cannot be improved by posterior decompression and fixation because of severe ventral compression pathologies. Full-endoscopic transcervical ventral decompression of the CVJ is useful in these cases. This procedure does not require a special approach and is familiar to spine surgeons. The main point of this technique is the strategy for decompression. It is important to understand which cases require partial or total decompression of the odontoid. In addition, the characteristics of each instrumentation should be understood to ensure selection of good indications for instrumentation.
Notes
Ethical statements
This study was approved from the ethical committee of Juntendo University (C21-0065).
Conflict of interest
Yukoh Ohara is the Editor of the Journal of Minimally Invasive Spine Surgery and Technique and was not involved in the review process of this article. All authors have no other potential conflicts of interest to declare relevant to this article.