Full Endoscopic Translaminar Approach Using 7 mm Working Endoscope for High Up Migrated Disc Herniation with Severely Collapsed Disc Space: Technical Note
Article information
Abstract
The clear indication for the transforaminal approach is simple or low migrated lumbar disc herniation (LDH). The incidence of migration of the disc fragment in LDH varies from 35% to 72%. The high up migrated disc herniation into MacNab’s hidden zone remains technical challenge. We provide a technical note of seldomly performed full endoscopic translaminar approach with its potential indications. A 52 years male patient presented with low back pain with left lower limb radiculopathy for 2 months. Visual analogue scale for back and leg was 2 and 8, respectively. MRI examination revealed high up migrated disc herniation with collapsed disc space at L4-5. Dynamic radiograph was not showing any instability. Based on the preoperative surgical planning working cannula was docked over left L4 lamina perpendicular to horizontal plane. With the help of 3.5 mm endoscopic burr translaminar keyhole was drilled in a concentric manner. The distance between lateral margin of pars and keyhole was intermediately inspected for preservation of adequate bone in pars interarticularis. Though the translaminar key hole subluxated tip of SAP, up-migrated disc fragment was removed. The VAS score of leg reduced significantly from 8 to 2 in immediate postoperative period. At the end of 6 months follow up period patients leg symptoms completely improved with minimal back pain. We measured the width of remaining pars postoperatively and found to be 5 mm. The full endoscopic translaminar approach is valid alternative approach for the high up migrated HNP.
INTRODUCTION
Endoscopic spine surgery has evolved over last few decades due to constant improvement in the optics, endoscopic instruments and technique. The full endoscopic transforaminal approach rapidly gained popularity due to its minimal invasive approach, ability to performed under Local anaesthesia, shorter hospital stay and early rehabilitation [1]. However, the clear indication for the transforaminal approach is simple or low migrated lumbar disc herniation (LDH). The L5-S1 LDH, high grade migrated LDH and coronal deformity with Significant foraminal stenosis are relative contra indications for the transforaminal approach due to various bony obstacles. The incidence of migration of the disc fragment in LDH varies from 35% to 72% [2,3]. Many spine surgeons modified transforaminal approach to reach the migrated disc fragment such as outside in technique, foraminoplasty or transpedicular approach etc.; with various degree of success. However high up migrated disc herniation into MacNab’s hidden zone remains technical challenge due to presence of bony and neural obstacles. Application of same endoscopic principles to interlaminar approach expanded the spectrum of pathologies which can be tackled with ESS. As compared to transforaminal approach the interlaminar approach is much anatomical and versatile. The following case report describes the patient with high up migrated disc herniation with severely collapsed disc space managed with full endoscopic translaminar approach. We provide a technical note of this seldomly performed endoscopic procedure with its potential indications for use.
CASE REPORT
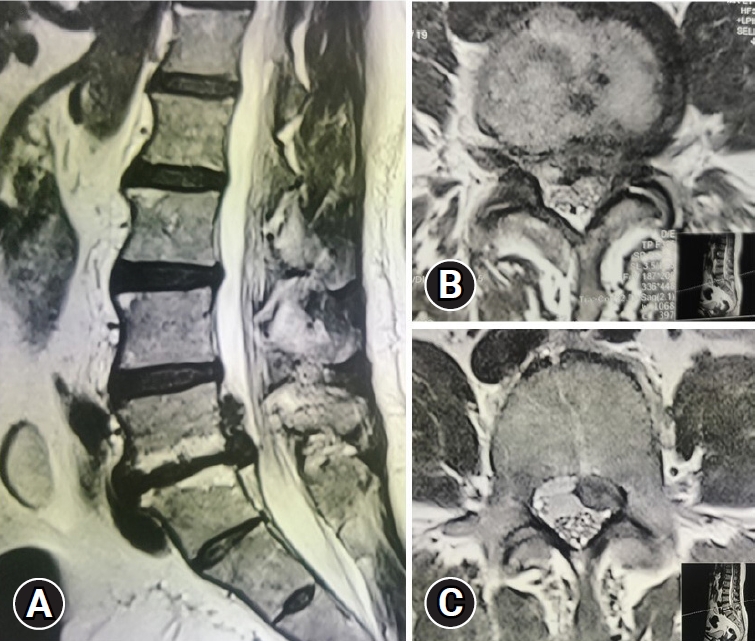
A 52 year male patient presented with low back pain with left lower limb radiculopathy since 2 months. Patients pain severity on visual analogue scale for back and leg was 2 and 8, respectively. The neurological examination was normal. MRI examination revealed high upmigrated disc herniation with collapsed disc space at L4-5 level (Figure 1). Though end plate was showing type 2 modic changes, dynamic radiograph was not showing any segmental instability. Initially patient was tried with conservative line of treatment in form of analgesics, physiotherapy and epidural injection which failed to response hence, patient was planned for full endoscopic translaminar discectomy.
Surgical Technique
The preoperative planning is necessary for the translaminar approach. On plain AP radiograph, width of the isthumus and length of L4 lamina was measured to determine the safe dimension of translaminar keyhole which can be drilled into left L4 lamina. The lateral radiograph was examined to plan docking point and trajectory of bone drilling towards the targeted disc fragment. MRI scan was assessed for the extent and migration of disc fragment from a disc space. Procedure was performed under general anaesthesia. Patient was placed in prone position over a radiolucent table with lumbar spine in flexion. Based on the preoperative surgical planning 18G spinal needle was passed percutaneously over left L4 lamina perpendicular to horizontal plane. The appropriate trajectory and target point of the needle was confirmed in AP and lateral fluoroscopy. A needle was replaced with guide wire followed by serial dilator and finally 7 mm working cannula. A 25 degree endoscope with OD 6.9 mm, ID passed into working cannula (Vertebris; RIWOspine, GmbH, Knittlingen, Germany) and further procedure carried out under full endoscopic vision. The soft tissue dissection and hemostasis was carried out with a RF probe until outer cortex of lamina was visualized. The bony drilling was started with 3.5 mm endoscopic burr in a concentric manner. The colour change of bone was visualized from white outer cortex to red spongy bone to white inner cortex. The distance between lateral margin of pars and keyhole was intermediately inspected for preservation of adequate bone in pars interarticularis. Once the inner cortex is penetrated endoscopic hook is used to separate the ligamentum flavum from under surface of L4 lamina. The ligamentum flavum and subluxated tip of superior articular process is resected with endoscopic punches. The scope was partially advanced into the keyhole for better visualization and accessibility. The bleeding from lateral recess and foramen was controlled with RF probe. The subligamentous part of disc herniation was teased out with the help of endoscopic hook and expulsed fragment was removed with the forceps. The hidden zone was explored with the help of flexible instruments such as RF probe and articulated forceps. The loose disc fragment underlying the exiting nerve root was pulled into operative field with flexible forceps and later removed under endoscopic vision. The final decompression was verified with free floating traversing and exiting nerve root along with empty axillary space. An endoscope is withdrawn slowly to examine the translaminar keyhole, intramuscular bleeding points. The wound was closed with a single stich. The VAS score of leg reduced significantly from 8 to 2 in immediate postoperative period. Patient was ambulated from day 1 with corset belt. At the end of 6 months follow up period patients leg symptoms completely improved with minimal back pain(Figure 2).
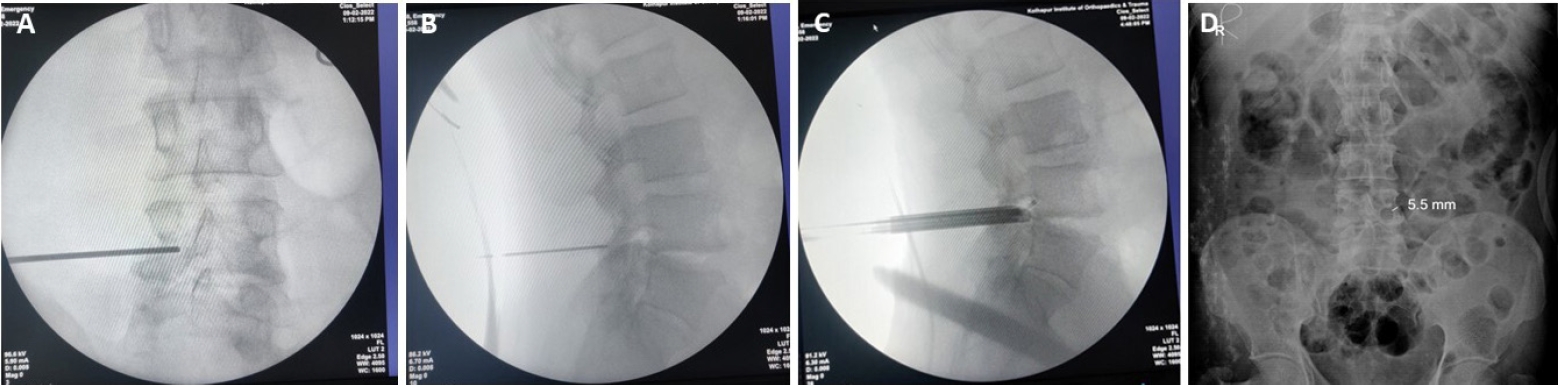
(A) Intraoperative fluoroscopic AP and (B) lateral image showing precise docking of spinal needle over left L4 lamina. (C) Intra-operative lateral fluoroscopic image showing partial advancement of bevel into keyhole. (D) Postoperative AP radiograph showing keyhole with preservation of pars interarticularis (5.5 mm).
DISCUSSION
The full endoscopic transforaminal approach has evolved over last 2 decades for management of degenerative disc diseases. However, there are some limitations for the approach due to presence of natural anatomic barriers [4]. A high-grade migration of disc imposes greater difficulty for the transforaminal approach due to presence of exiting nerve root cranially and pedicle caudally. The incidence of fragment migration in HNP varies from 35% to 72% [2,3]. Lee et al. [5] classified migration of the disc depending upon the extent of migration into near migrated disc and far migrated disc herniation. Also, they concluded that open microdiscectomy may give superior results compared PTED for far migrated disc herniation. Uniyal et al. [6] first described transpedicular approach for high down migrated disc herniation. Similarly, various spine surgeons tried transpedicular approach with significant success rate [7-9]. Kim et al. [10] narrated 3 routes of transforaminal approach to approach the high migrated HNP. The development of posterior interlaminar approach by Ruetten et al. [11,12] has expanded the spectrum of lumbar pathologies which can be managed with full endoscopic technique. However, the up migrated HNP into hidden zone remains a technical challenge for the transforaminal approach. Though it can be managed with the interlaminar approach; it needs extensive bony drilling which increases soft tissue resection and surgical time. Di Lorenzo et al. [13] first proposed the translaminar approach using microscope in 1998 which was later supported by case series by Soldner et al. [14] in 2002. The critical comments for the translaminar approach were technical difficulty of a technique, inability to clear the disc space and iatrogenic fracture of pars interarticularis. All these difficulties can be overcome with the use of working endoscope as done in this case. It improves the visualization through translaminar keyhole which reduces the amount of bone resection and effectively chance of iatrogenic pars fracture. In 2012, Dezawa et al. [15] reported percutaneous endoscopic translaminar approach (PETA) for disc herniation with satisfactory results. Lin et al. [16] published preliminary results of 13 patients having high (n=8) and very high (n=5) grade migration. The mean operative time was 79.2 minutes with 92.3% of success rate. The operative time for the current case report was 98 minutes with negligible blood loss. We measured the width of remaining pars postoperatively and found to be 5 mm. According to Papavero and Kothe [17] at least 3 mm lateral border of pars need to be spared to avoid delayed pars fracture. The 25-degree optical angle of endoscope allows the clear visualisation of the hidden zone between the exiting nerve root and dural sac. The articulated instruments helped to deliver the fragment lying inferior to the exiting nerve root. As the disc space was collapsed the disc space exploration was not performed. However, the subluxated tip of superior articular process compressing on exiting nerve root is resected. The annuloplasty was performed with RF probe. The advantages of the translaminar approach are 1. It is minimal invasive; 2. It has shorter operative time as compared to routine translaminar approach; 3. Shorter hospital stay with early mobilization. The relative contra indication for present technique is LDH associated with ligamentum flavum hypertrophy, moderate to severe canal stenosis or facet cyst which absolutes the use of interlaminar approach [18]. The key surgical points while performing translaminar approach are 1. Precise docking of working cannula over target point; 2. Maintaining accurate trajectory of concentric drilling with preservation of lateral bony bridge; 3. The exiting nerve root decompression with the help of flexible forceps with minimal neural retraction [19]. It can be applied for down migrated disc herniation; however modified transforaminal approach or transpedicular approach can be used with the same precision. Current technique has its own limitations such as it has significant learning curve and limited indication, it needs precise docking and trajectory of bony drilling to reach the migrated fragment of disc and possibility of intra/postoperative pars fracture cannot be ruled out.
CONCLUSION
The full endoscopic translaminar approach is valid alternative approach for the high up migrated HNP. It has certain advantage over routine interlaminar approach as it preserves the motion segment with shorter operative time. However, the technique has significant learning curve with limited indications.
Notes
Ethical statements
The patient and relative has given informed written consent for the submission of a case report to the journal.
Conflicts of interest
Hyeun-Sung Kim is the Editor-in-Chief of the Journal of Minimally Invasive Spine Surgery and Technique and was not involved in the review process of this article. All authors have no other potential conflicts of interest to declare relevant to this article.
Supplementary Materials
Supplementary Video 1.
Full endoscopic translaminar approach for far up migrated L4-5 disc herniation. (https://doi.org/10.21182/jmisst.2023.00682.v001).