Clinical Results and Review of Techniques of Thoracic Endoscopic Unilateral Laminotomy with Bilateral Decompression (TE-ULBD) Using the Outside-In Technique for Thoracic Ossified Ligamentum Flavum
Article information
Abstract
Objective
Uniportal full endoscopic thoracic endoscopic surgery can be performed through transforaminal and interlaminar approaches. The interlaminar approach is commonly described as thoracic endoscopic unilateral laminotomy for bilateral decompression (TE-ULBD), which is typically indicated for pathologies such as ossified ligamentum flavum and other posteriorly based compressive pathologies. TE-ULBD decompresses the central and lateral recesses of the thoracic spinal canal. Both the outside-in (over the top of ligamentum flavum) and inside-out (under the ligamentum flavum) approaches can decompress the thoracic spinal canal through the uniportal interlaminar endoscopic route.
Methods
A retrospective clinical cohort evaluation of patients who underwent TE-ULBD was performed from January 2018 to December 2021
Results
A cohort of 50 cases of TE-ULBD with a mean age of 65 years old were evaluated. The complication rate was 5.4% and the reoperation rate was 2%. Statistically significant mean VAS improvements were found at 1 week, 6 months, and the final follow-up, with changes of 3.95±1.49, 4.95±1.7, and 5.2±1.8 points, respectively. Likewise, the mean Oswestry Disability Index improvements at 1 week, 3 months, and the final follow-up were 33.8±9.05, 40.12±10.38, and 41.92±11.26, respectively (p<0.001). Significant improvements were found in the cross-sectional area of the spinal canal in the upper endplate, mid-disc, and lower endplate (57.62±50.6, 89.86±55.93, and 64.93±60.91 mm2, respectively; p<0.001).
Conclusion
TE-ULBD using the outside-in technique could achieve good clinical outcomes and a low rate of complications in our cohort of patients.
INTRODUCTION
Thoracic myelopathy is an insidious and debilitating spinal condition leading to gait instability, thoracic back and radicular pain and lower limb weakness and numbness. One of the common causes of thoracic myelopathy is thoracic ossified ligamentum flavum (OLF). The incidence of thoracic OLF is low [1]. Open posterior thoracic decompression of thoracic OLF is associated with significant surgical risks and perioperative comorbidities [2,3]. Osman et al. [4] described the rate of complication for open laminectomy of thoracic OLF is approximately 18.4%. One of the common complications of decompressive thoracic OLF surgery is dura tear. Kim et al. [5] and Wu et al. [6] described in separate literature of the use of uniportal Thoracic Endoscopic Unilateral Laminotomy With Bilateral Decompression (TE-ULBD) with good clinical results and lower complication rates. There is an increasing demand for endoscopic spine surgery as a form of minimally invasive surgery with potentially less perioperative morbidities and early mobilization which leads to improved early postoperative surgical outcomes [7,8]. There are limited literature describing the technique of TE-ULBD in the literature [5,6,9]. Most of the literature on thoracic endoscopic decompression focuses on the anterior transthoracic retropleural transforaminal endoscopic thoracic discectomy.
Difference between Inside-Out versus Outside-In Thoracic Endoscopic Unilateral Laminotomy with Bilateral Decompression
In lumbar spinal stenosis with posterior compressive pathologies such as thickened ligamentum flavum and facet cysts, there are several technical approaches described for LE-ULBD to achieve the same target of spinal decompression [10-13]. The main difference focuses on the over the top of ligamentum flavum decompression and under the ligamentum flavum decompression approach of LEULBD, which recently coined as Outside-in by Kim et al. [11] and Inside-out by Lim et al. [14]. In this study, we evaluated the efficacy and outcomes of Outside-in thoracic endoscopic unilateral laminotomy with bilateral decompression.
MATERIALS AND METHODS
This retrospective study was reviewed by institutional review board of Nanoori Hospital, Seoul, Republic of Korea. All patients signed consent to have their data collected for study.
Retrospective clinical evaluation of patients who met indications of Thoracic endoscopic unilateral laminotomy with bilateral decompression (TE-ULBD) were included in the study. These are patients who were included presented with thoracic back pain and/or myelopathy with MRI and CT demonstrated clinically significant thoracic ossified ligamentum flavum. We excluded revision surgery, patients who had concurrent tumor, infection, instability of thoracic spine and fractures. Collection of pre and postoperative clinical data of Clinical Visual Analog Scale and Oswestry Disability Index, MJOA, Motor Power was done retrospectively in clinical consultation at 1 week post-operative, 6 months post-operative and final follow up. All the included patients underwent Thoracic Endoscopic Unilateral Laminotomy With Bilateral Decompression Using Outside-In Technique.
1. Thoracic Endoscopic Unilateral Laminotomy with Bilateral Decompression Using Outside-In Technique
1) Preparation
All patients in our cohort underwent general anesthesia and positioned prone on Wilson frame on a radiolucent operating table. The patient’s arms were padded and positioned next to the patient.
2) Surgeon Position and Skin Marking
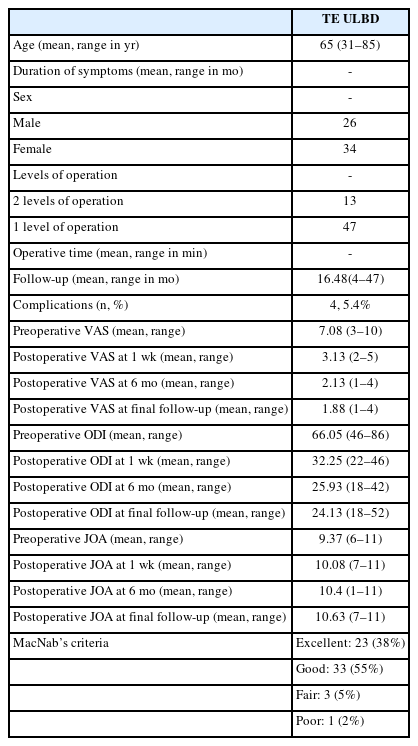
The surgeon stood on the side with the symptoms or the side with more significant stenosis shown on the CT and MRI scan. Careful counting of the correct level of thoracic spine under the fluoroscopic guidance of anteroposterior (AP) and lateral view were performed. The planned skin incision located at the intersection of medial pedicle line and mid disc line on the AP view and on the lateral view of the mid disc of the correct surgical level is described as the “V” point (Figure 1).
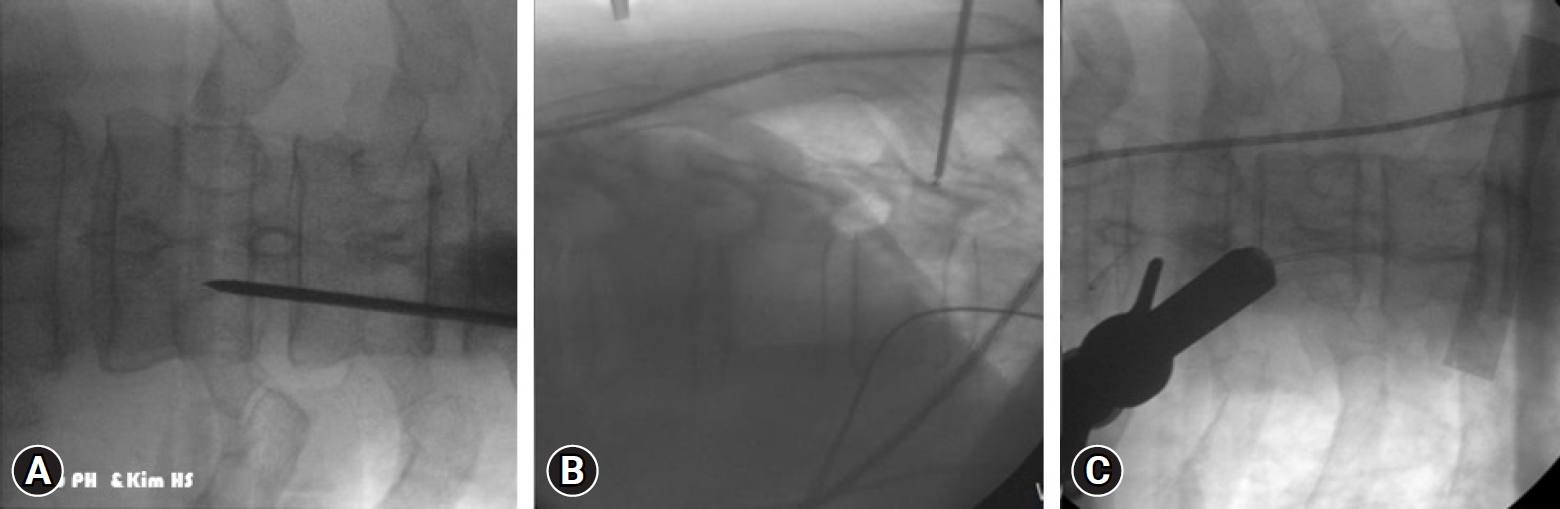
Intraoperative fluoroscopic pictures of right T7/8 thoracic endoscopic unilateral laminotomy with bilateral decompression (TE-ULBD). (A) A skin incision is marked on the medial pedicle of right T8 on anteroposterior view. (B) Corresponding lateral view with a guide wire placed on the medial and mid-pedicle region of right T8. (C) Serial dilation and docking of the retractor tube and endoscope on the right T8 pedicle to prepare for a sublaminar approach in TE-ULBD.
3) Serial Dilation and Docking
Typically, we made a 1 cm skin incision and fascia cut followed by serial dilation and an endoscopic working retractor cannula slide through the dilators to allow smooth insertion of an endoscope (Figure 1). We recommend using a uniportal stenosis scope with approximately 8–10 mm outer diameter endoscope and a 5–6 mm working channel to facilitate the use of endoscopic drill, radiofrequency ablator and Kerisson rongeur. The recommended continuous irrigation pressure of normal saline is 25–30 mmHg.
4) Soft Tissue Dissection and Exposure of Bony Anatomy
Once docking of working cannula on the V point was confirmed on fluoroscopic images, radiofrequency ablation device was used to dissect the muscle and soft tissue to expose the capsule of the facet joint, cephalad and caudal lateral part of the bony lamina surrounding the bony “V” point. Using the endoscope we carefully evaluate the facet joint size so that resection is not taken beyond the midpoint to prevent over resection of the facet joint. We take care not to violate the pars interarticularis to maintain segmental stability of the affected level of thoracic spine.
5) Outside-In Bony Decompression Endoscopic Drilling
Endoscopic drilling was performed to widen interlaminar space from medial to lateral and cephalad to caudal direction in order to expose the attachment of ossified ligamentum flavum. Care was taken to preserve at least half of the inferior articular facet. The cephalad lamina and the base of spinous process base was drilled in a sublaminar approach to the free edge of ossified ligamentum flavum. Once only paper thin membrane of ligamentum flavum covering the ipsilateral epidural space is seen. We continued to perform endoscopic drilling over the top of ipsilateral and contralateral ossified ligamentum flavum to approach the contralateral cephalad lamina and contralateral ventral portion of inferior articular process and medial half of contralateral superior articular process to the contralateral lateral edge of ligamentum flavum. This is followed by endoscopic drilling on the ipsilateral and contralateral caudal lamina till the contralateral edge of the ligamentum flavum was paper thin. Ossified ligamentum flava of both sides were kept during endoscopic bony drilling to prevent inadvertent dura puncture.
2. Gentle Seperation of Ligamentum Flavum from Dura and Removal of Ossified Ligamentum Flavum
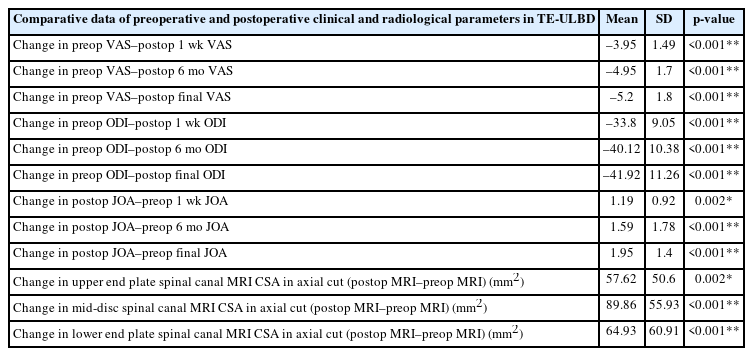
The exposed thinned-out edges of bilateral OLFs are carefully lifted off from the underlying dura by a blunt endoscopic penfeel. Any underlying adhesion of the OLF is separated by the combination of radiofrequency ablation and penfeel. We retrieved ligamentum flavum en bloc with forceps or Kerrison rongeurs once the OLF is free of all attachments. If OLF is tightly adhered to the dura, we thin out the OLF by endoscopic drilling and left it as an island of OLF free of attachment to surrounding structures (Figure 2A).
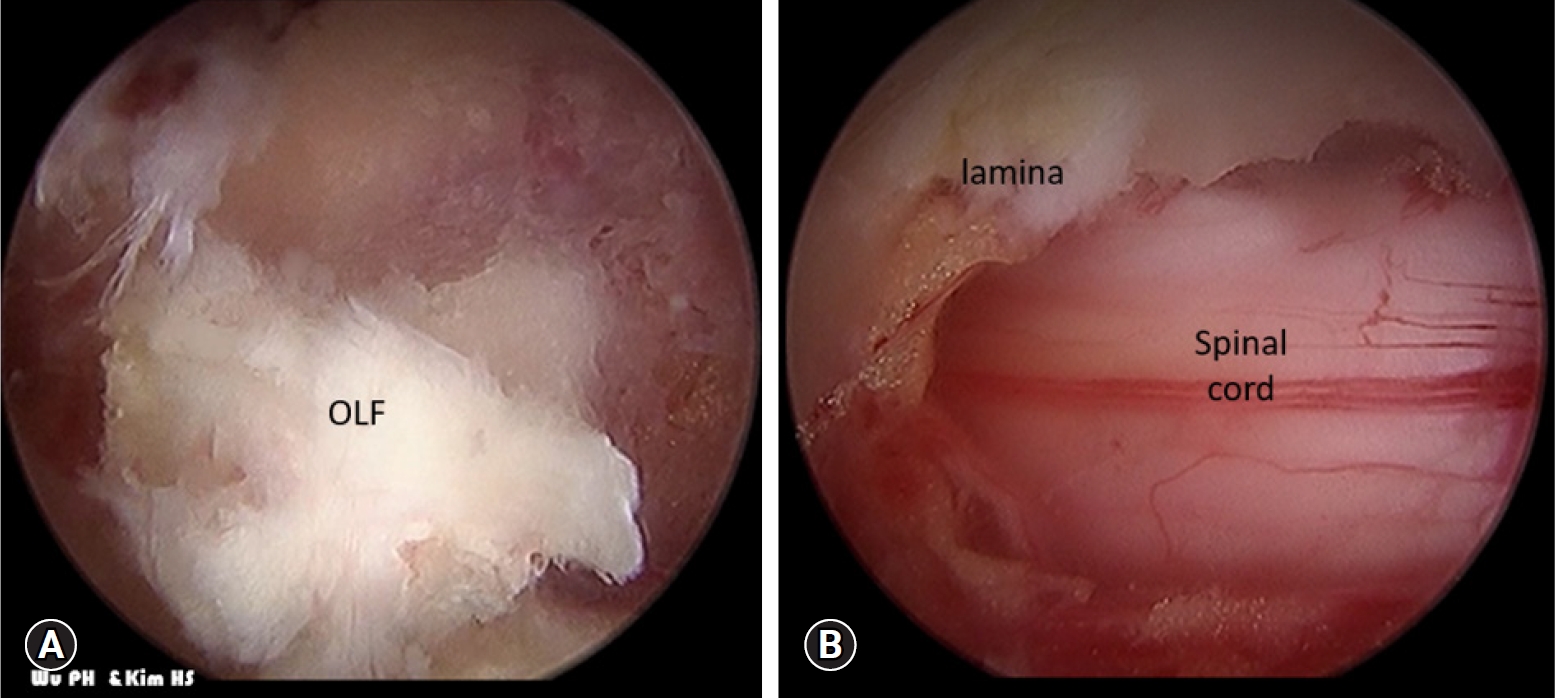
(A) Intraoperative picture demonstrates the isolation of thoracic ossified ligamentum flavum (OLF). (B) Complete en bloc removal of OLF with the spinal cord decompressed and pulsating. The authors used a similar approach in thoracic spinal compressive pathologies. A retrospective analysis of clinical outcome of our cohort of TE-ULBD outside in patient cohort was performed.
3. Final Assessment of Status of Neural Elements and Dura
Neural elements and dura is checked for any dura tear and the thoracic cord pulsation under irrigation fluid. We confirmed under endoscopic vision that bilateral lateral edge of the dura, cephalad and caudal part of dura were decompressed (Figure 2B). Unlike lumbar spine, throughout the entire surgery there should not be any attempt to retract the cord during any step of surgery. A drain was inserted and anchored and skin was closed in layers. We typically removed the drain on postoperative day 1 if drainage is less than 80 mL over 24 hours.
4. Statistical Analysis
Clinical data was analyzed with SPSS version 18 statistical analysis software (IBM corporation, New York). The continuous variables were expressed as mean and standard deviation (SD). The paired t-test was used clinical visual analogue scale (VAS), Oswestry Disability Index (ODI), Modified Japanese Orthopaedic Association Score (MJOA) measured at pre-operative, 1 week post-operative, 6 months post-operative and final follow up reported by the patients were analysed. A value of (p<0.05) considered significant within the cohort.
RESULTS
After meeting both inclusion and exclusion criteria, 60 levels of TE-ULBD performed in 60 (26 male and 34 female) patients. Forty-seven patients underwent one level, 13 patients underwent 2 levels of TE-ULBD. The patients were recruited from May 2018 to July 2022. The mean follow up was 16.5 (4–47) months. Mean age of the cohort was 65 years old (Table 1).
1. Clinical Outcomes
The overall complication rate of TE-ULBD was 5.4%. There was one case of incomplete decompression which was picked up in postoperative MRI, he underwent revision TE-ULBD with successful decompression. There were 2 dural tears were treated with patch blocking repair technique [15]. One of the dura tear patient had paraparesis with partial recovery to power 4 on bilateral lower limbs. The other patient with dura tear had no clinical sequelae. One patient had incomplete decompression and underwent revision TE-ULBD without clinical sequelae and one patient had developed facet cyst after 12 months which was treated conservatively. MacNab score 38% patients with excellent, 55% with good, 3% with fair and 2% with poor results (Table 1).
In TE-ULBD group, there was significant improvement in the mean±standard deviation as compared to preoperative VAS in postoperative 1 week (3.95±1.49), 6 months (4.95±1.7), and final follow up (5.2±1.8), p<0.001. There was significant improvement in the mean±standard deviation as compared to preoperative ODI in postoperative 1 week (33.8±9.1), 6 months (40.12±10.38), and final follow up (41.92±11.26), p<0.001. There was significant improvement in the mean±standard deviation as compared to preoperative JOA in postoperative 1 week (1.19±0.92), 6 months (1.59±1.78), and final follow up (1.95±1.4), p<0.001 (Table 2 and Table 3).
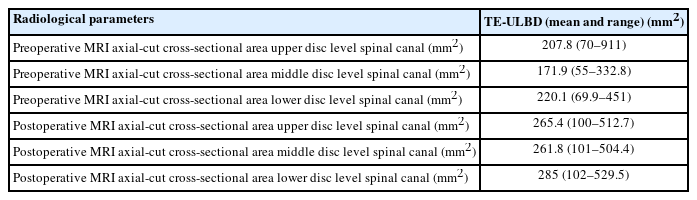
Radiological parameters with the MRI axial cut cross-sectional area at the upper, middle, and lower disc level in TE-ULBD
2. Radiological Outcomes
In TE-ULBD cohort’s radiological outcomes, there was significant statistical increase in decompression cross section spinal canal area (SCA) dimension in postoperative compared to preoperative MRI scan with mean and standard deviation increase of 1) upper disc 57.62 (±50.6) mm2, 2) middle disc 89.86 (±55.93) mm2, 3) lower disc 64.93 (±60.91) mm2, p<0.001 (Table 2).
DISCUSSION
There is an increasing incidence of thoracic OLF being treated surgically [8]. The traditional surgical treatment is posterior laminectomy along with flavectomy to increase spinal canal volume. The laminectomy is performed with open and tubular microscopic approach traditionally [16]. There are limited literature in thoracic endoscopic decompression. The steep learning curve in orientation of thoracic surgical anatomy and potential implications in incomplete decompression and significant complications are some of the reasons why there are limited publications on this topic [17]. The concept of TE-ULBD is an evolution of development of Lumbar Endoscopic Unilateral Laminotomy With Bilateral Decompression (LE-ULBD) technique, Lim et al. [14] described inside out (under the ligamentum flavum decompression approach and above the spinal cord) and Kim et al. [11] described outside-in (over the top of ligamentum flavum decompression) approach to decompress the bilateral epidural space lumbar spinal stenosis. The main instrument used in inside-out i.e., under ligamentum flavum decompression approach is endoscopic Kerisson Rongeurs to remove the ligamentum flavum and bony lamina together piecemeal, to gain early access to the epidural space in the procedure. While outside-in i.e., over the top decompression approach requires endoscopic drilling of lamina and medial facet leaving the ligamentum flavum intact in order to protect spinal cord from endoscopic drill. Both authors highlighted the pros and cons of their technique. Most surgeons however do a hybrid of both techniques hence it is a theoretical proposition for inside-out versus outside-in technique in lumbar spine. However the authors felt that in the case of thoracic OLF decompression performed with TE-ULBD technique, outside-in en bloc approach is preferable to reduce complications [5,6].
Dangers and Potential Complications
Both under the ligamentum flavum and over the top decompression of ligamentum flavum approaches, the common complications are dura tear, neck pain/headache due to water irrigation pressure and incomplete decompression [18]. Dura tear can happen in 3% to 10% of lumbar cases with a higher dura tear complication rate in thoracic spine [4]. We found in our series there is dura tear rate of 3.3%. Small incidental durotomy can be repaired by patch blocking repair technique using gelfoam and tachosil [15]. Neckache and headache can be prevented by limiting the duration of surgery with high irrigation pressure. Optimal irrigation pressure is in the range of 25–45 mmHg with the mean of 30 mmHg [11,19]. Incomplete decompression is a common risk in any decompression surgery. The steep learning curve in endoscopic spine surgery is one of the reason for these complications [8,17]. Spinal instability is a potential complication despite studies showed that endoscopic surgery may preserve more facet joints and potentially lower the risk of instability [16,20], more long term data is required to demonstrate the role of spinal endoscopy in preservation of facet joint. Small wounds and conservation of soft tissue in TE-ULBD may decrease infection risk compared to open surgery. Endoscopic decompression has higher risk of incomplete decompression compared to open decompressive surgery, we have a case of incomplete decompression which required revision TE-ULBD. With experience and intraoperative CT scan, we can potentially reduce the rate of inadequate decompression. The risk of devastating neurological deficit in thoracic spinal decompression is a dreaded complication. We have one case of incomplete recovery from paralysis. Ruetten et al. [21], Kim et al. [5], and Wu et al. [6] showed lower risk in neurological deficit in their series of Thoracic endoscopic decompression, however more studies are required to show reproducibility of their techniques.
In our cohort of patients who underwent the “outside-in approach” TE-ULBD, they demonstrated statistically significant improvement clinically and radiologically at various time point of follow up, with a relatively low rate of complications of 5.4%. (Figure 3)
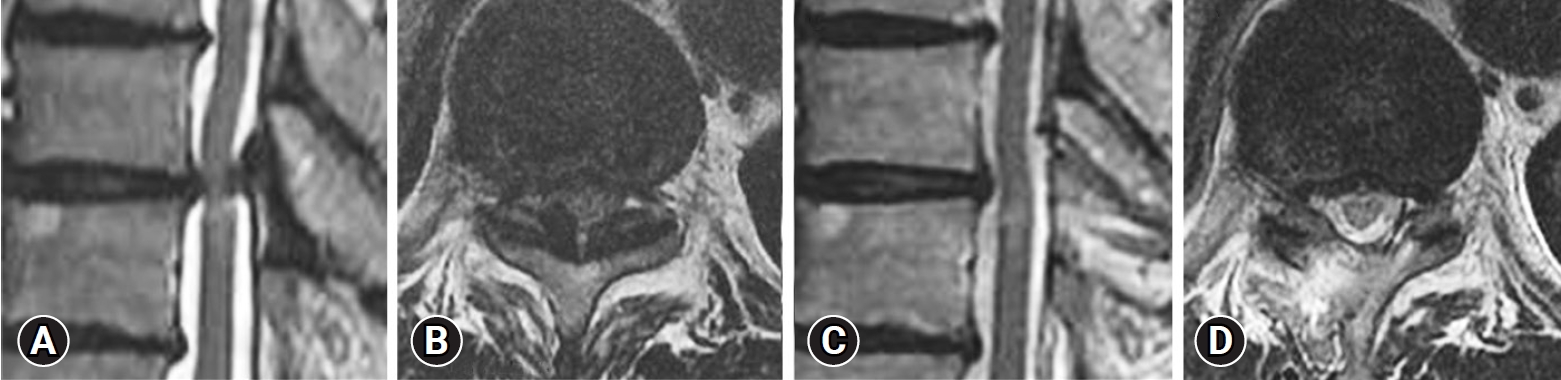
(A, B) Right T7/8 sagittal and axial MRI cut with thoracic ossified ligamentum flavum causing spinal cord compression. (C, D) Corresponding sagittal and axial cut with decompression by right T7/8 thoracic endoscopic unilateral laminotomy with bilateral decompression. MRI: magnetic resonance imaging.
CONCLUSION
Thoracic Endoscopic Unilateral Laminotomy Bilateral Decompression Outside-In Technique could achieve good clinical outcomes and low rate of complications in our cohort of patients.
Notes
Ethical statements
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Nanoori Hospital’s Ethics Committee and the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent from patients: All patients had given their informed consent for photographs, videos, and images for publication.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
No potential conflict of interest relevant to this article.