Intraoperative Anteropulsion of an Interbody Fusion Cage During Minimally Invasive Transforaminal Lumbar Interbody Fusion: A Case Report
Article information
Abstract
Expandable cages are very commonly used during minimally invasive lumbar interbody fusion surgery for better restoration of sagittal alignment. We present a rare event of intraoperative expandable cage anteropulsion into the retroperitoneal space. To date, several cases of cage migration have been reported. However, ours is the first case of intraoperative anterior cage migration during minimally invasive lumbar fusion. Herein, we present a case of 70-year-old female planned for minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) for grade II L5–S1 lytic spondylolisthesis. There was an unnoticed anterior longitudinal ligament rupture during the cage expansion manoeuvre. Cage dislodgment was noticed intraoperatively. This was managed by compression of the interbody site posteriorly and insertion of another snugly fitting bullet cage, followed by anterior retroperitoneal exploration in the same setting to retrieve the migrated cage. The patient’s postoperative course was satisfactory. At a 1-year follow-up, patient was ambulatory and asymptomatic. Follow-up imaging showed bony fusion and no signs of implant failure. Expandable TLIF cages can cause iatrogenic release of the anterior longitudinal ligament during expansion. Surgeons must be aware of this rare complication, which can result in anterior cage migration.
INTRODUCTION
Transforaminal lumbar interbody fusion (TLIF), a posterolateral approach to lumbar fusion, was initially described in 1982 by Harms and Rollinger. It gained popularity in 1992 after work by Harms and Jeszenszky [1,2]. Open TLIF procedure carries the disadvantage of iatrogenic soft tissue injury. A novel surgical technique of minimal invasive TLIF (MIS TLIF) by use of serial tubular dilators and muscle retracting approach was introduced by Foley et al. [3] in early 2005 which has now become increasingly popular. Although rare, anterior cage migration during TLIF can be catastrophic and life threatening with possibility of vascular and bowel injuries [4-6]. We present a case report of intraoperative anteropulsion of a cage into the retroperitoneum during MIS TLIF. To date, several cases of cage migration have been reported. However, this is the first case that reports intraoperative anterior cage migration during MIS TLIF.
CASE REPORT
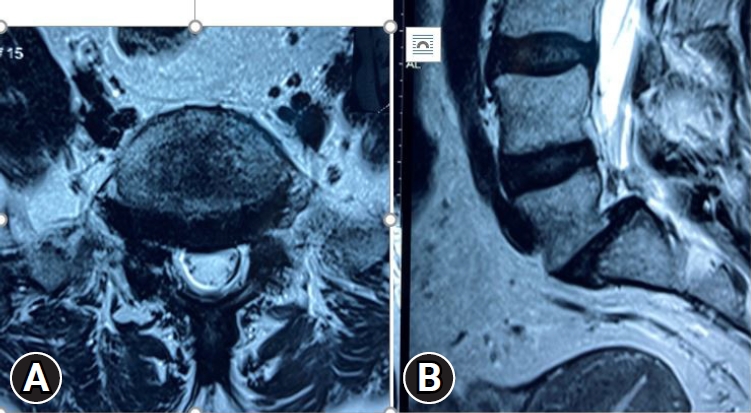
A 70-year-old female with body mass index of 40 was seen at the spine clinic, with history of low back pain over one year with aggravation of symptoms, bilateral lower limb radiculopathy and neurogenic claudication for around 6 weeks. The onset of symptoms was insidious without any prior traumatic event. On examination, walking distance was less than 500 m with no neurological deficit. Reflexes and other general spine examination was found to be normal. She was advised magnetic resonance imaging (MRI) of the lumbosacral spine and dynamic lumbosacral x-rays which were suggestive of grade 2 mobile L5–S1 lytic spondylolisthesis (Figure 1). Patient had no other comorbidities except her obesity. Patient underwent MRI scans depicting findings as shown in Figure 2. Given the radiographic findings, surgical plan was MIS TLIF with expandable cage.
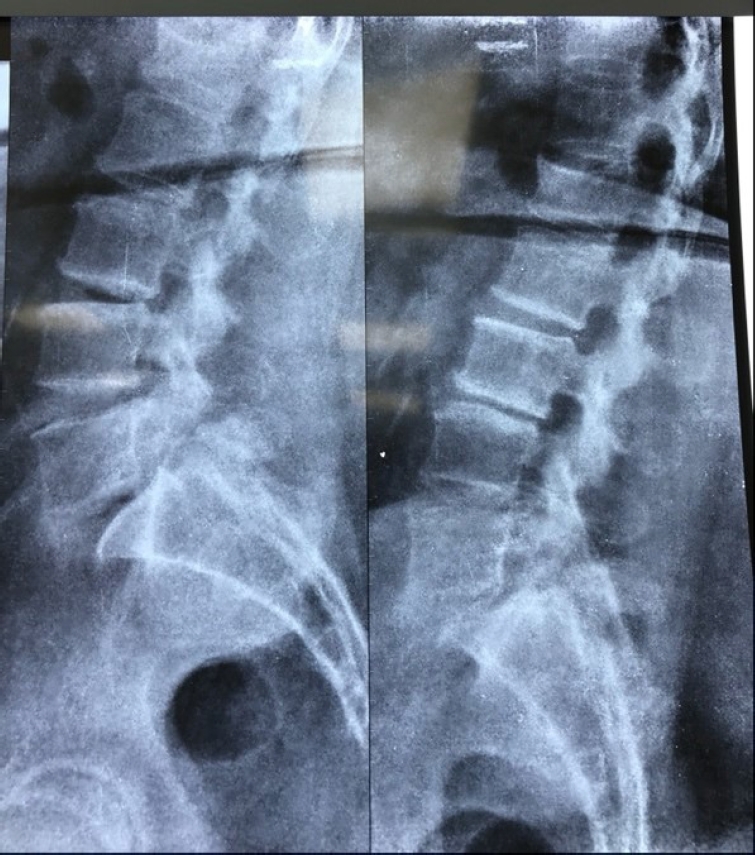
Dynamic x-ray film of lumbosacral (LS spine) suggestive of mobile grade II lytic spondylolisthesis at L5–S1. Extension view (A) and flexion view (B).
1. Surgery and Intraoperative Complication
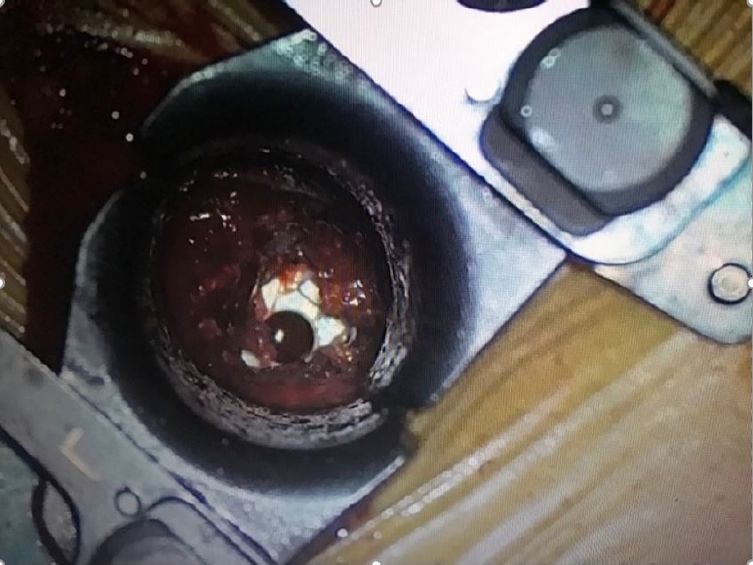
Decompression and interbody fusion were performed with expandable Medtronics tube system. Unilateral facetectomy and discectomy was done after direct visualization and protection of traversing and exiting nerve roots. Shavers of progressively increasing size were used for interbody site preparation and residual disc material was removed. Endplate preparation was done with help of straight and 30 degree bend curette as provided in the implant set. Intraoperatively, after end plate preparation, trial cage was inserted and checked on C arm. After appropriate selection of trial cage which was snuggly fitting on both endplates, Wave-D expandable cage (Medtronics, Minneapolis, MN, USA) of 12 mm was inserted and further expanded to 14 mm after placement between L5–S1 vertebral bodies. Position of the cage after expansion was found to be appropriate. After removal of holder, bone graft was inserted into the expandable cage. The cage slipped from its position after graft insertion and this was noticed through the microscope. Intraoperatively, total slippage of the cage through the anterior margins of both L5–S1 vertebral bodies breaching the anterior longitudinal ligament (ALL) was identified, potentially risking major vessel and bowel. No attempts were made to remove the cage posteriorly considering potential devastating complications which may arise and it was left in situ (Figure 3).
2. Surgical Management
After notifying anaesthesia team, vitals were noted stable, and an on call vascular access surgeon was informed. Pedicular screws of size 6.5 mm×40 mm were inserted at L5–S1 level and fixed with rods. Meanwhile decision was taken to insert another nonexpandable bullet cage measuring 12 mm packed with bone graft. The interbody site was compressed first to reduce the anterior defect and then a bullet cage of size 12 mm was inserted. It was positioned off centre and fitted snuggly to prevent slippage through an apparent central defect in ALL (Figure 4). Wound was closed in layers and intraoperative consent was taken from relatives after explaining the complication. The patient was positioned supine and the migrated expandable cage was approached through anterior retroperitoneal approach which was found below bifurcation of abdominal aorta. On direct visualization, there was no visceral injury. The dislodged cage was then removed and wound was closed in layers (Figure 5). Postoperatively, patient was haemodynamically stable. At 1 year of follow-up, patient was ambulatory and asymptomatic. Follow-up imaging showed bony fusion and no signs of implant failure.
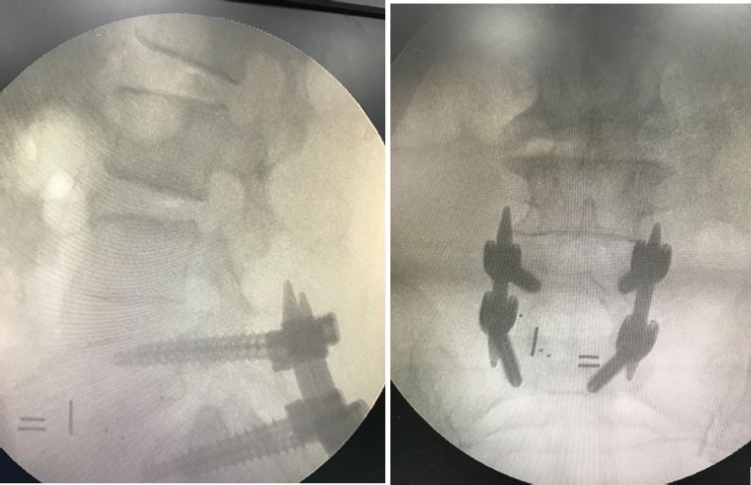
Fluoroscopy lumbosacral spine lateral view (A) and anteroposterior view (B) showing posterior fixation with bullet cage while leaving anteropulsed cage in situ.
3. Ethics Statement
A valid informed consent of patient was taken for publication of case report.
DISCUSSION
With changing demographics, prevalence of diseases related to aging has increased. TLIF offers circumferential arthrodesis of spine via single stage posterior approach. The advent of microscopic surgeries has allowed TLIF procedure to become minimally invasive i.e., MIS TLIF; which offers added advantages of lesser tissue trauma, less blood loss, reduced infection rates and early mobilization. Drift towards minimally invasive techniques of interbody fusion has increased challenges dealing with complications. Besides neural injury, infection, dural injury and screw malposition, TLIF carries risk of cage migration. Cage migration can be classified as anterior, posterior or sagittal, depending upon the direction [7]. Anterior cage migration has catastrophic complications due to visceral injury [5,6,8,9].
There are no fixed guidelines for retrieval of anteriorly migrated cages due to paucity of literature. L4–5 [8] and L5–S1 [10] are the most common sites of anterior TLIF cage migration. In our case, L5–S1 was the site of cage migration. Retroperitoneal migration of cage usually occurs due to over preparation of disc space, uncontrolled hammering of cage during insertion without fluoroscopy, inappropriate position of cage, osteoporosis and ALL rupture [4,8]. Severe obesity or decreased load bearing capacity has been documented to increased risk of cage migration [11].
Wong et al. [12] found a 0.97% of cage migration in their MIS TLIF series of 512 patients. In selected cases where cage had migrated anteriorly and vitals remained stable, the surgery was completed leaving the cage/graft in place [4]. Although in other cases immediate removal of cage/graft was done to prevent impending complication due to major vessel compression [13]. Iatrogenic perforation of ALL during discectomy has been reported in the literature with collateral damage to bowel and left common iliac artery and vein [14,15].
In our case, we used wave-D expandable cage to attain additional lordosis which also has the provision of inserting bone graft after cage expansion to accommodate a large graft size. While inserting bone graft inside the expanded space using a funnel, dislodgment and anterior migration of the cage was noticed. Intraoperatively a central breach in the ALL was documented which is thought to be happened during cage expansion manoeuvre. Our case has come to show that while improving lordosis through an expandable cage from a posterior approach, iatrogenic ALL breach can be an impending complication especially in old fragile patient and with aggressive surgical manoeuvres. Care should be taken that bigger size shavers and overzealous use of curettes to remove the endplate might damage the subchondral bone. This damage to bone may cause complications of implant subsidence. Although in our case, some manoeuvres performed during endplate preparation might be contributing factors of ALL damage, it was only during cage expansion that the ALL gave away and cage slipped anteriorly.
Unlike previously reported cases of anterior cage migration, we inserted snuggly fitting nonexpandable bullet cage of 12-mm size pre-packed with bone graft. This was done only after compressing pedicle screw over rods so as to minimise the anterior ALL opening. Most commonly, anterior transperitoneal or lateral retroperitoneal approaches are recommended for cage extraction [16]. We took retroperitoneal approach with the help of vascular access surgeon and retrieved the migrated cage. The rationale behind inserting another cage was to obtain stable construct with anterior column support.
CONCLUSION
In summary, surgeons must be aware of intraoperative anterior cage migration due to iatrogenic rupture of ALL while using expandable interbody cages. The exact incidence of such events is rare and due to scarcity of literature, comprehensive management guidelines are lacking.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.