A Review of Fully Endoscopic Lumbar Interbody Fusion
Article information
Abstract
Over the past 10 years, fully endoscopic lumbar interbody fusion (FE-LIF) has been widely reported as a rational alternative to minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF), and several FE approaches for interbody fusion have been published. The short-term surgical outcomes of FE-LIF are reportedly superior to those of MIS-TLIF and conventional posterior LIF in terms of intraoperative blood loss and short-term back pain. However, the complication rate, medium-term clinical outcomes, and fusion rate have not been reported to be different in all uncontrolled studies. The challenges associated with FE-LIF include a longer operative time, which means a steep learning curve, and limited surgical indications, which leads to patient selection bias. FE-LIF is an excellent surgical option for treating degenerative disc disease, spinal instability, and spondylolisthesis. Although the amount of evidence is very small in existing studies and the long-term follow-up data are limited, this technique shows favorable clinical outcomes in selected patients.
INTRODUCTION
Various surgical procedures for lumbar interbody fusion (LIF) have been reported, including posterior LIF (PLIF), transforaminal LIF (TLIF), lateral LIF (LLIF), and anterior LIF (ALIF). LIF is indicated for various lumbar degenerative diseases, such as lumbar canal stenosis, spinal instability, spondylolisthesis, foraminal stenosis, disc herniation, and degenerative scoliosis [1]. Conventional open posterior fixation surgery is preferred as it has a shallow learning curve, offers sufficient decompression, and has wide indications and steady operative outcomes. However, due to the large incision and extensive paravertebral muscle dissection, the innervation and blood supply of the paravertebral muscles, such as multifidus and longissimus muscle, are considerably damaged during conventional posterior fixation surgeries. Many patients (~25%–35%) Intractable low back pain (LBP) after conventional PLIF and TLIF accounts for an increase in back pain visual analogue scale (VAS) scores from 3 to 5, which adversely affects patients’ quality of life [2]. Therefore, many spine surgeons have made significant efforts to reduce surgical complications such as soft tissue damage and LBP caused by conventional PLIF and TLIF, respectively. In 1988, Wiltse and Spencer [3] described a posterolateral approach through the space between the multifidus and the longissimus muscle to the foramina for the treatment of far-lateral disc herniation, spinal canal stenosis, and lumbar spondylolisthesis. Because the Wiltse approach significantly reduces paraspinal muscle damage and blood loss and makes direct exposure to the insertion point of the pedicle screw easier, it has been widely used for pedicle screw insertion. In 2002, Foley et al. [4] reported minimally invasive transforaminal fusion. Since its introduction, the MIS‐TLIF procedure has gained consensus among most spine surgeons. The terms Wiltse TLIF and MIS-TLIF are often used interchangeably these days. Wiltse TLIF and MIS‐TLIF are both minimally invasive surgical procedures with the advantages of less intraoperative bleeding, paravertebral muscle damage, shorter hospital stay, and significantly reduced long‐term complications such as those with intractable LBP [5-7]. Many studies have reported the clinical benefits of Wiltse TLIF and MIS-TLIF in the treatment of degenerative lumbar diseases, with less intraoperative blood loss (50–80 mL) and shorter hospital stays (2–5 days) [8,9]. Over the past few decades, the surgical technique has become more advanced and less invasive [10]. Spinal endoscopic technology and techniques have been continuously evolving since the early 2000s, with various innovations being introduced over the years [11-18]. The use of a uni-portal endoscopic system is becoming more popular for decompressing central canal and lateral recess stenosis [19-24]. Full-endoscopic LIF (FE-LIF) has been made possible through advancements in endoscopy technology, improved endoscopic instruments to facilitate soft and bony tissue removal, and improved surgical skills in endoscopic discectomy and neural decompression [25]. In full-endoscopic transforaminal lumbar discectomy, the target working zone is Kambin triangle. The area is also crucial for transforaminal fusion techniques, as it determines the entry point into the intervertebral disc. Disc height determines the cranial and caudal dimensions of the neuroforamen. The length of the pedicle, facet joint arthritis, and hypertrophic ligamentum flavum influence the size of Kambin triangle. Furthermore, pathological conditions such as lumbar disc herniation, degenerative spondylolisthesis, and foraminal stenosis can lead to changes in the position of the nerve roots. In the case of herniated discs, the exiting nerve root can deviate in any direction, depending on the location of protruding or extruding disc material. Kim et al. [25,26] reported the use of uniform portal facet-sacrificing post-erolateral TLIF (ETLIF). ETLIF was described as a means for performing interbody fusion using a large-channel endoscope with unilateral facet removal to create a working space for disc preparation and insertion of the interbody cage. Conversely, Morimoto and Ishiyama et al. [27,28] reported on the full-endoscopic trans-Kambin triangle LIF (FE-KLIF). They partially removed the superior articular process using a surgical drill until Kambin’s triangle was large enough to safely insert a box-type dilator in the next step.
Osteotomy aims to remove an adequate amount of bone required to expose 12 mm of the intervertebral disc surfaces. Kim et al. [34] reported that on radiological evaluation, both ETLIF and FE-KLIF showed promising results in terms of fusion rate and cage subsidence, comparable to those of other fusion methods. Exiting nerve root injury and subsidence are the most critical complications of FE-KLIF [29,30]. In contrast, incidental durotomy and traversing nerve root injury are possible complications related to ETLIF [31,32]. To prevent nerve root injury, Morgenstern et al. [33] suggested approaching Kambin triangle by performing foraminoplasty and disc preparation, followed by the insertion of the expandable cage and pedicle screws. Kim et al. [34] reported that the application of single-level ETLIF helped achieve better clinical outcomes and fusion rate with less subsidence than microscopic MIS-TLIF in midterm evaluation among patient cohorts. However, in some cases, other LIF procedures were preferable to ETLIF or FE-KLIF. First, the pelvis is often an obstacle for patients with degenerative spondylolisthesis at the L5/S1 level. Therefore, it may be difficult to insert the cage correctly. Second, in terms of operations, time, and corrective force, lateral LIF may be preferable to FE-KLIF for the correction of multilevel vertebral deformities is required. Finally, conventional PLIF or TLIF is preferable in cases requiring posterior decompression. Examples include cases with severe bony canal stenosis, ossification of ligamentum flavum and those with significant thickening of the ligamentum flavum, which makes it challenging to achieve symptomatic improvement with indirect decompression [27]. The full-endoscopic interlaminar approach, which is a well-known standard in full-endoscopic spine surgery, has rarely been applied to endoscopic lumbar fusion surgery. Full-endoscopic posterior lumbar interbody fusion (FE-PLIF) via an interlaminar approach can help achieve direct decompression of bony canal stenosis and safe interbody fusion.
To the best of our knowledge, only a few systematic reviews and meta-analyses have been conducted on FE-PLIF have been published. This review aims to clarify the distinction between FE-KLIF and FE-PLIF, and reports that FE-LIF is an extremely minimally invasive and safe surgical procedure for degenerative lumbar disease.
MATERIALS AND METHODS
Although this study was a narrative review, we also followed the Cochrane Handbook for Systematic Reviews of Interventions protocol. This study was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses as closely as possible [35,36].
1. Search Strategy
We searched Medline using PubMed, Embase, and the Cochrane Library databases on July 10, 2023, without restrictions on revision, publication type, or language. The following search terms were used : “(full endoscopic OR percutaneous endoscopic) AND (minimally invasive) AND (interbody fusion) AND (lumbar) AND (transforaminal) OR Kambin OR posterior )”.
2. Eligibility Criteria
In this study, only English-language articles were included. First, the remaining articles were assessed by title and abstract, and duplicate articles were erased. We excluded articles on air-based microendoscopic techniques using tubular retractor systems (MED system), laparoscopic ALIF, and endoscopy-assisted LLIF or oblique LIF. Systematic reviews, meta-analyses, cadaver studies, case reports, technical reviews, and reports that did not analyze the cases were excluded. After the screening, the full texts were reviewed and excluded if they fell under any of the following exclusion criteria: (1) the noncomparative study; (2) articles about standalone endoscopic fusion without transpedicle screw fixation; and (3) not related to clinical outcomes, including pain, complications, surgical time, blood loss, and fusion rate. The extracted details included first author, study design, year, and demographics information. It also covered the indication for surgery, surgical procedure (including anesthesia and intervertebral cage), operative time, blood loss, clinical scores (VAS for back and leg pain, and Oswestry Disability Index [ODI]), outcomes related to complications, and fusion rate.
RESULTS
1. Study Selection
The database search resulted in the identification of 115 studies. After screening the titles and abstracts according to the inclusion/exclusion criteria and removing the duplicates, 15 studies remained for full-text review. Finally, 15 articles were included in this study [37-49].
2. Characteristics of Eligible Studies
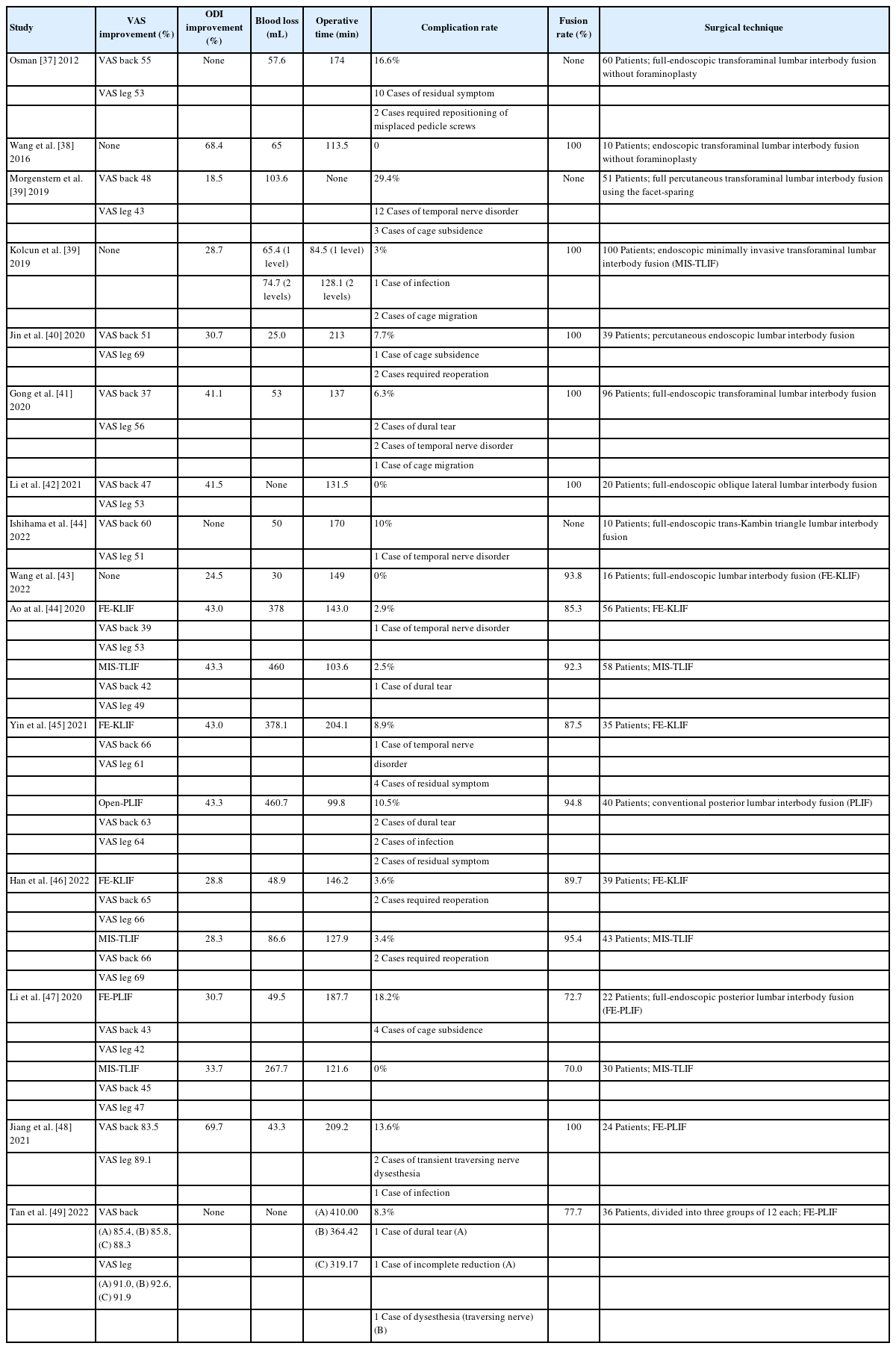
Among all studies, indications were identified as lumbar degenerative diseases such as disc herniation, canal stenosis, and spondylolisthesis. All studies reported clinical outcomes, including preoperative and postoperative VAS scores of the back/leg or ODI, surgical outcomes, including operation time, blood loss or incidence of complications, and fusion rates (Table 1).
3. Clinical Results of the Selected Studies
The clinical outcomes are summarized in Table 1, with surgical invasiveness assessed for blood loss and operative time. The VAS and ODI scores used to measure low back and leg pain were reported in 15 studies, all of which reported improved scores after surgery. There was no significant difference in the improvement rate of the VAS of the back/leg and ODI differences between FE-KLIF, FE-PLIF, MIS-TLIF, and conventional PLIF. Intraoperative blood loss was higher in MIS-TLIF and conventional PLIF than in FE-KLIF and FE-PLIF. The operative time was significantly longer in the FE-KLIF and FE-PLIF groups. The overall fusion rates at the final follow-up were not significantly different between FE-KLIF, FE-PLIF, MIS-TLIF, and conventional PLIF.
4. Complications
Complications are summarized in Table 1. Ishihama et al. [28] reported that one patient who underwent FE-KLIF complained of an existing nerve root injury that improved within 2 weeks after surgery. Postoperative dysesthesia was the most frequent complication and was primarily caused by exiting nerve root injury via the trans-Kambin triangle or the transforaminal approach. In this series, postoperative dysesthesia of the exiting nerve root was confirmed in 17 of the 532 FE-KLIF cases (3.2%). Unlike the trans-Kambin triangle or transforaminal approach, in the case of FE-PLIF, postoperative dysesthesia or motor weakness is mainly caused by traversing nerve root injury at the lateral recess. Morgenstern et al. [30] reported that 12 of their cases (23.5%) developed transitory 190 ipsilateral dysesthesia. In all 191 cases, dysesthesia resolved completely by an average of 7.2 weeks postoperatively after oral pregabalin treatment or selective nerve block. Transitory ipsilateral muscle weakness developed in 2 of the 12 patients, and resolved fully by an average of 8.2 weeks after surgery. In this series, postoperative dysesthesia of the traversing nerve root was confirmed in 3 of 82 (3.7%) FE-PLIF cases. Furthermore, 1 of the 131 MIS-TLIF and 40 conventional PLIF cases had postoperative dysesthesia. Ao et al. [44], who compared KLIF and MIS-TLIF, reported that one patient in the KLIF group showed a decrease in muscle strength to MMT 4/5 in the quadriceps femoris, which recovered by one month after surgery. A dural tear occurred in one patient in the MIS-TLIF group. Yin et al. [45] reported no significant difference in the complication rates between the FE-KLIF and conventional PLIF groups (p=0.67). Two patients who underwent conventional PLIF developed a surgical site infection, and 2 developed cerebrospinal fluid leakage. Conservative treatment was successful in all cases. Two patients complained of postoperative residual numbness, which resolved over time. In their series, there were no significant differences in the fusion rates between FE-KLIF, FE-PLIF, and MIS-TLIF.
DISCUSSION
The Endo-LIF procedure was first reported by Leu and Hauser [50] in 1996. Many studies have reported that FE-KLIF and other types of full-endoscopic lumbar decompression and interbody fusion lead to faster recovery and ambulation, along with less collateral tissue damage during microsurgery and tubular surgery, resulting in an early return to normal life for patients [18,37,38,44,51-53]. Few other study results were consistent with these reports, showing less blood loss, shorter hospitalization, and earlier LBP improvement in the FE-PLIF group [47-49]. There was no significant difference in clinical and radiologic outcomes at the final follow-up between FE-KLIF, FE-PLIF, and MIS-TLIF. Nevertheless, FE-PLIF requires more time for spinal decompression and endplate preparation than conventional fusion techniques such as MIS-TLIF.
Postoperative dysesthesia caused by nerve damage is a common complication of FE-KLIF. Ahn [18] reported that the working tube used in surgical procedures could potentially irritate the exiting nerve root, especially in cases with long surgery times. Conscious sedation and neuromonitoring may help reduce the incidence of intraoperative root injury. Preoperative magnetic resonance imaging is helpful in detecting anatomical anomalies such as conjoined nerve roots [54]. The surgeon’s knowledge of anatomical landmarks and precise C-arm fluoroscopic guidance may help prevent neurological injury.
Choi et al. [55] reported that the overall complication rate of FE-KLIF was 13.2% (range, 0%–38.6%). The most frequent complication observed was postoperative dysesthesia, which is primarily caused by exiting nerve root injury during the trans-Kambin triangle or transforaminal approach [56]. In patients with a narrow Kambin triangle, there is a risk of irritation to the exiting nerve root if the cannula is placed too close to the exiting nerve root. Unlike the trans-Kambin triangle or transforaminal approach, the FE-PLIF procedure uses an interlaminar space to reach the target pathological structure under a familiar surgical anatomy. In FE-PLIF, postoperative dysesthesia or motor weakness is mainly caused by traversing nerve root injury at the lateral recess. Compared with the advantages of other approaches, patients with severe bilateral and central bony canal stenoses may benefit more from this interlaminar approach, which enables better access to the contralateral side than the unilateral Kambin triangle.
Li et al. [47] reported that fusion rates with definite grades were not significantly different between the FE-PLIF and MIS-TLIF groups, reaching 73.3% in the FE-PLIF group, similar to those reported in previous studies [17,37,56,57]. Recent research has highlighted the suitability of expandable interbody fusion cage implants for full-endoscopic fusion [58]. These cages, requiring smaller cannulas, offer several advantages such as adjustable height and lordosis angle, facilitating controlled restoration of disc height and segmental lordosis. In addition, the expansion force of the cage may result in greater indirect decompression, thereby reducing the risk of cage migration.
Nonetheless, long-term follow-ups should be conducted to further evaluate the efficacy of interbody fusion and the adverse effects of cage subsidence in FE-KLIF and FE-PLIF procedures.
The indications of FE-KLIF and ETLIF are generally similar to those of conventional open PLIF or TLIF. In this review, FE-KLIF was performed for a wide range of diseases, including canal stenosis, degenerative spondylolisthesis, lumbar disc herniation, and lumbar degenerative disc disease. However, in some cases, other intervertebral fusion techniques are preferred over KLIF or ETLIF. First, in patients with degenerative spondylolisthesis at L5/S1, the pelvis is often an obstacle, and it may be difficult to insert the cage correctly. Second, given the operation time and corrective force required, lateral LIF may be preferable to FE-KLIF and ETLIF when multilevel vertebral deformities are corrected. Finally, conventional PLIF or TLIF is preferable in cases requiring posterior decompression. Examples include cases with ossification of the ligamentum flavum and those with significant thickening of the ligamentum flavum, which makes it challenging to achieve symptomatic improvement with indirect decompression [59]. The posterior interlaminar approach, a well-known standard in full-endoscopic spinal surgery, has rarely been used in endoscopic lumbar fusion surgery. FE-PLIF via an interlaminar approach can help achieve direct decompression of bony canal stenosis and safe interbody fusion.
CONCLUSION
According to this narrative review, the overall outcomes, including short-term outcomes, surgical complications, and fusion rates, were not significantly different among FE-KLIF, FE-PLIF, MIS-TLIF, and conventional PLIF. However, in terms of rapid recovery after surgery with less invasiveness, less bleeding, and diminished surgery-related back pain, FE-KLIF and FE-PLIF are more favorable than MIS-TLIF and conventional PLIF, despite the disadvantages of a steep learning curve and longer operation time.
Notes
Conflicts of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.