Partial Vertebrectomy in Neglected Spondyloptosis at the T10–11 Level: A Case Report
Article information
Abstract
Our objective was to document the surgical results from a case and conduct a retrospective analysis of partial vertebrectomy in neglected spondyloptosis at the T10–11 level. Traumatic spondyloptosis is a severe and rare spinal cord injury. In spondyloptosis, there is a traumatic subluxation of adjacent vertebral bodies that exceeds the normal anatomical limits. The thoracic vertebrae possess a rigid skeleton, and the sternum also contributes to maintaining stability in the upper-middle chest area. Therefore, instances of spondyloptosis in the thoracic spine are exceedingly rare. Thoracic spondyloptosis typically results in neurological deficits. A 45-year-old man presented to the neurosurgery outpatient clinic complaining of weakness of lower extremities, back pain, headache, and vomiting. The patient was hospitalized for 7 days, and he was diagnosed with neglected spondyloptosis based on a computed tomography scan. The patient was treated using laminectomy decompression, bilateral facetectomy, partial vertebrectomy, and posterior stabilization. Management in cases of spondyloptosis has the aim of reduction, alignment, and stabilization. Early surgery with reduction and rigid stabilization is preferable to conservative treatment in most cases. The surgical approach can be anterior, posterior, or combined, without significant differences. Vertebrectomy is performed to remove part of the vertebral body to reduce spinal cord pressure. Thoracic spondyloptosis is a very rare but severe type of spinal cord injury. Neurological deficits are common in patients with this condition. Early management involving reduction and stabilization is generally recommended to obtain a better outcome.
INTRODUCTION
Spinal cord injury (SCI) is a neurological condition where there is damage to the spinal cord. The etiology can be divided into traumatic and nontraumatic etiologies. Data from the National Center for Spinal Injury Statistics state that there are approximately 12,500 new cases of SCI each year in North America, with traumatic etiologies accounting for more than 90% of cases [1]. The incidence of traumatic SCI was higher in men with a 2:1 ratio. The age distribution is bimodal, with the first peak involving young adults and the second peak involving >60 years of age. The reported incidence ranges from 12.1 to 57.8 cases per million population in high-income countries and 12.7 to 29.7 cases in low-income countries [2]. Primary damage from traumatic SCI will cause cellular damage and initiate a secondary injury cascade. Neuronal and glial cell death, ischemia, and inflammation occur due to injury. Changes in spinal cord architecture, such as the formation of glial scars and cystic cavities, will follow the injury cascade. The presence of poor intrinsic recovery potential can lead to neurologic deficits [3].
Traumatic spondyloptosis is a severe and rare form of SCI. In spondyloptosis, there is more than 100% traumatic subluxation of the adjacent vertebral bodies. High-energy trauma is required to produce a significant injury. Spondyloptosis is rare in the thoracic vertebrae [4]. The stabilizing effect of the associated coastal elements provides some stability and limits the dislocation spine. However, the thoracolumbar junction may be more vulnerable to dislocation because of the junction of the relatively fixed thoracic spinal segments with the mobile lumbar spine. Thoracic spondyloptosis generally causes neurologic deficits [5]. Posterior or anterior approaches or a combination of both can be used to correct traumatic spondyloptosis. However, correction of spondyloptosis via the anterior approach has several difficulties, such as failure to repair the dural tear and provide relief. This condition’s prognosis highly depends on the extent of the injury and the function maintained. Early management in the form of reduction and stabilization is generally recommended in cases to obtain a better outcome [6]. We report a rare case of American Spinal Cord Injury Association (ASIA) Impairment Scale (AIS) Grade A due to a rare case of thoracic spondyloptosis at level T10–11 with treatment in the form of laminectomy decompression, bilateral facetectomy, partial vertebrectomy, and posterior stabilization.
CASE REPORT
Before selecting individuals as the study subjects, researchers obtained consent from the patients who were used as subjects.
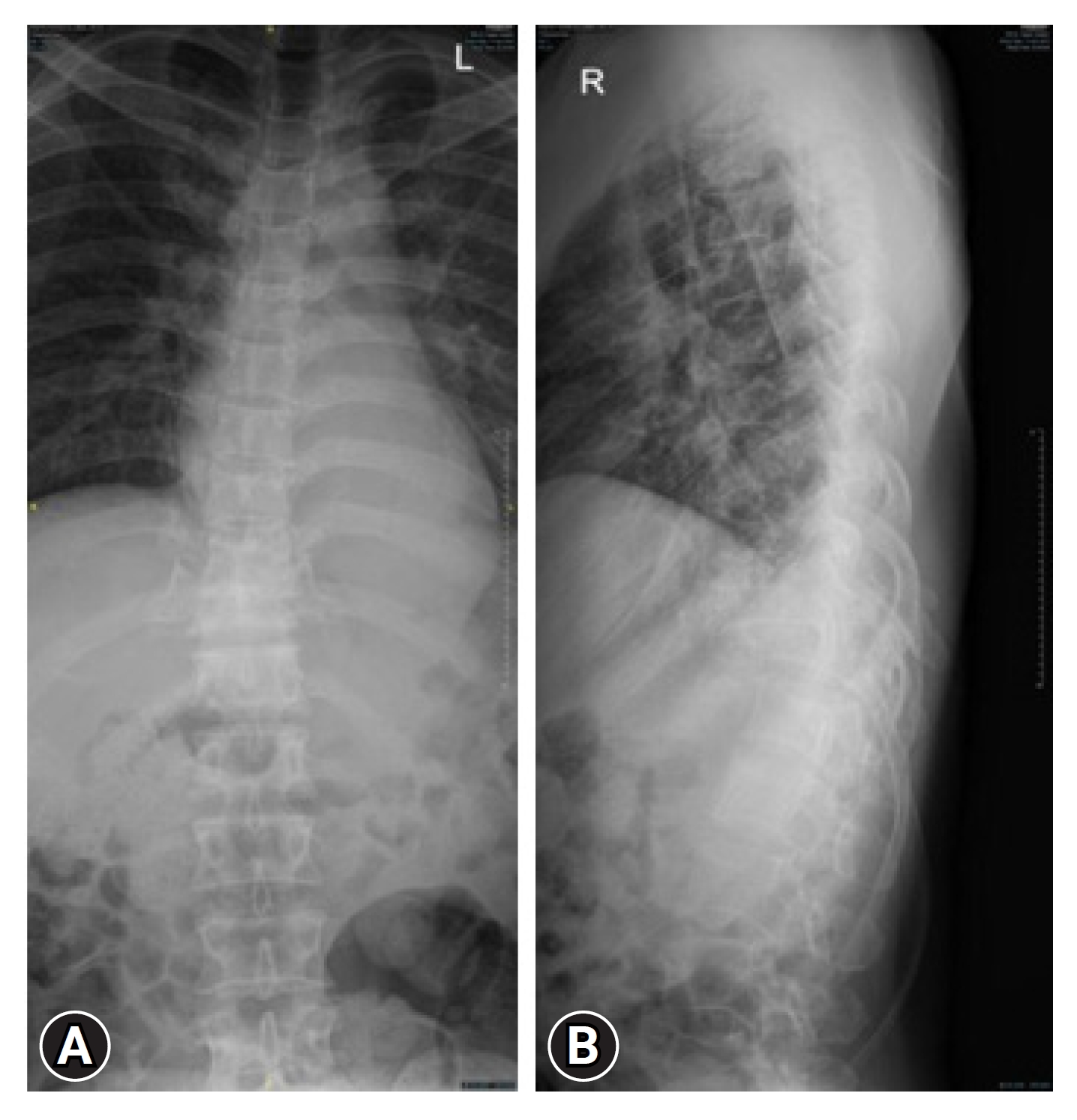
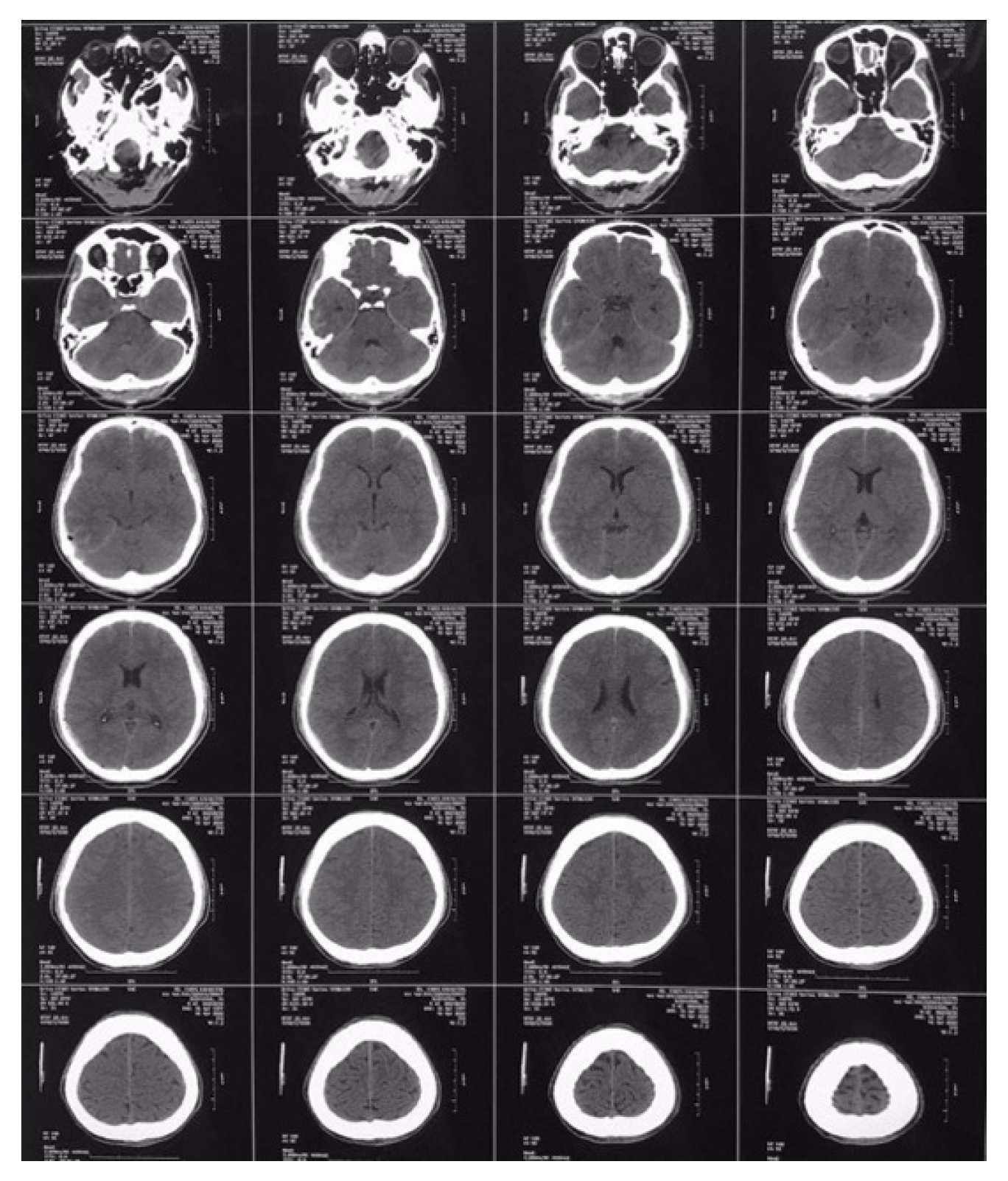
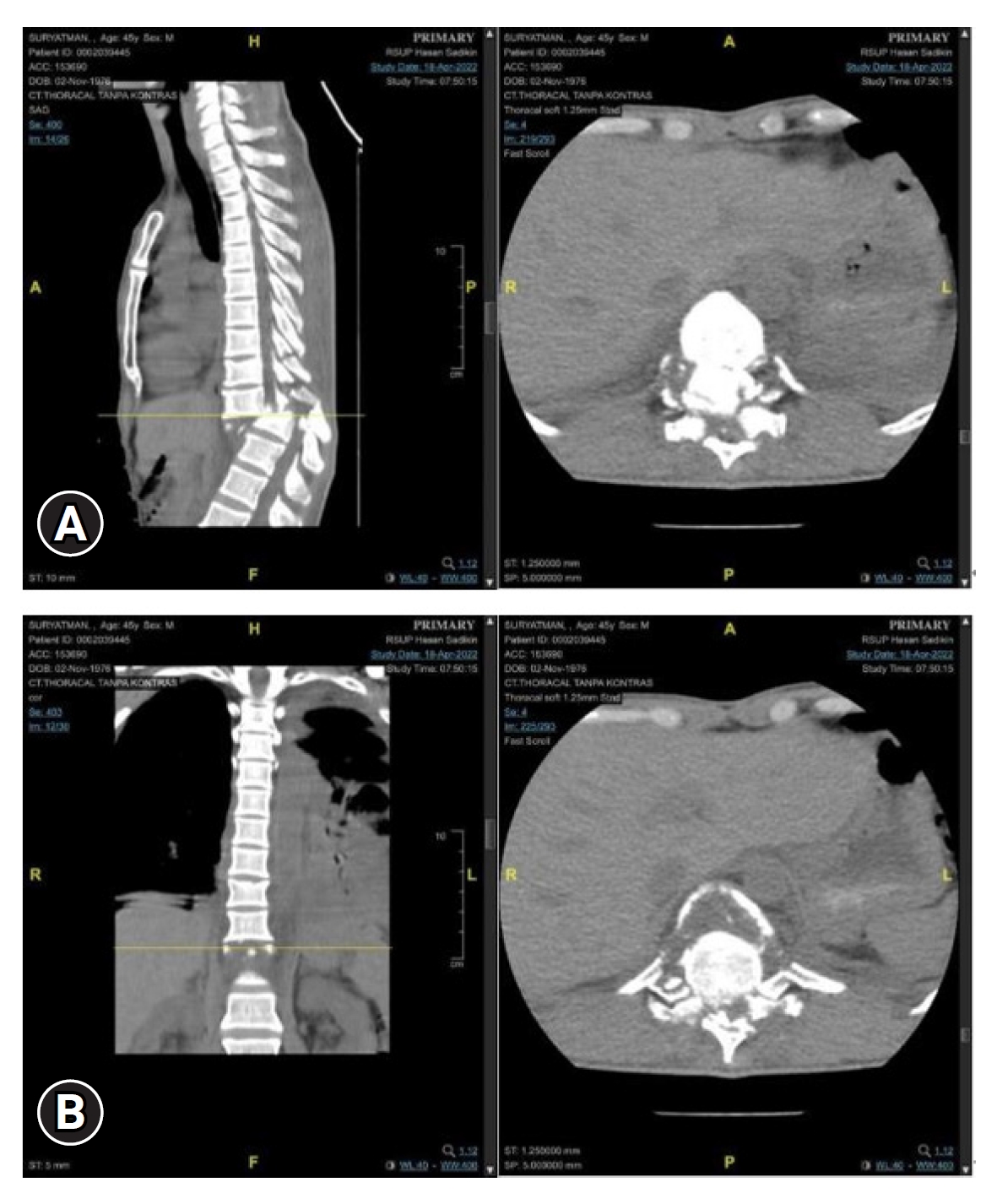
A 45-year-old male patient was brought to the Neurosurgery Emergency Department for laminectomy decompression and posterior stabilization (Figure 1). The patient previously complained of lower extremity weakness starting from the right leg. Complaints accompanied by back pain, headache, and vomiting. The patient was diagnosed with a mild head injury, which included a cerebral contusion in the frontal region along with an epidural hematoma in the right parietal area, as well as spondyloptosis at the T10–11 level (Figures 2, 3). The patient was hospitalized for 7 days, and a computed tomography (CT) scan showed neglected spondyloptosis. He was planned to undergo laminectomy decompression and posterior stabilization. At this point, due to the expiry of the patient's insurance, his family declined the recommended treatment, and as a result, he was discharged with persistent weakness in the lower extremities. In the meantime, his family sought alternative means to cure the disease while they also managed to reactivate his insurance package. Realizing that 2 months had passed without any improvement, the family then brought the patient back to the neurosurgery department.
On physical examination, the patient appeared compos mentis with mild pain. Vital signs within normal limits. On the thorax, found deformity, step-off, and tenderness. In the sacrum, found pressure sores and slough. Neurological examination showed the patient’s Glasgow Coma Scale (GCS) was 15. There was anesthesia at T10 and lower for sensory function. The catheter in this patient is attached. Physiological reflexes, pathological reflexes, and bulbocavernosus reflexes are absent.
The patient then underwent a series of examinations. Chest x-ray examination showed results within normal limits. The results of the thoracolumbar x-tray examination showed malalignment with spondyloptosis grade IV T10–11 (Figures 3, 4). The patient’s Thoracolumbar Injury Classification and Severity Scale (TLICS) score was 7. The assessment of the TLICS score for this case involved a systematic evaluation of several key parameters to determine the severity of the thoracolumbar injury. The TLICS scoring system considers 3 primary components: injury morphology, integrity of the posterior ligamentous complex (PLC), and the patient's neurological status. In this particular case, the injury morphology, as revealed by thoracolumbar x-ray and CT scans, indicated a significant dislocation and subluxation of vertebral segments at level T10–11, contributing significantly to the score. Additionally, the assessment of PLC integrity, based on imaging findings, revealed compromised posterior ligamentous structures, further increasing the score. Lastly, the patient's neurological status, carefully evaluated through clinical examination, highlighted sensory deficits at T10 and below, aligning with the neurological component of the TLICS scoring system. The collective assessment of these parameters resulted in a TLICS score of 7, indicating a severe thoracolumbar injury that warranted thorough surgical intervention and stabilization to mitigate associated risks and achieve optimal clinical outcomes. The patient also underwent a noncontrast head CT scan with the results of soft tissue swelling in the right parietal, linear bone discontinuities in the right temporoparietal, uncompressed sulcus and gyrus, uncompressed sylvian fissure, uncompressed ventricles and cisterns, lesions Bicovex hyperdense in the right parietal with a volume of about 5 mL with bilateral frontal salt and pepper features, and no midline shift. The patient was treated using laminectomy decompression, bilateral facetectomy, partial vertebrectomy, and posterior stabilization procedure.
(A) Noncontrast computed tomography of cervical spine showing lytic lesion involving body, pedicle, lamina, and spinous process of C5, 6, 7. (B) Sclerotic margin around margin of lesion is clearly seen.
To achieve the successful reduction of traumatic spondyloptosis at level T11 and restore proper vertebral alignment, a series of meticulous reduction maneuvers were skillfully employed during the surgical procedure (Figures 5, 6). These reduction maneuvers played a pivotal role in addressing the displacement and spinal cord compression associated with spondyloptosis. The reduction process involved the strategic placement of a 6-level pedicle screw and reduction screw assembly within the T8–L2 region, providing essential anchor points and controlled force for realignment. Subsequently, a bilateral laminectomy was performed to access the site of spondyloptosis, followed by a facetectomy to enhance visibility and create space for the critical reduction maneuvers. The cornerstone of the reduction process was the partial vertebrectomy at T11, meticulously executed to alleviate spinal cord compression and restore proper vertebral alignment. With the vertebral bodies realigned, rigid rods were carefully positioned to maintain alignment, and an essential crosslink was securely installed to enhance stability. These reduction maneuvers, conducted with a high degree of surgical expertise, were instrumental in achieving successful intraoperative realignment, mitigating spinal cord compression, and ultimately optimizing the patient's chances of a favorable clinical outcome.
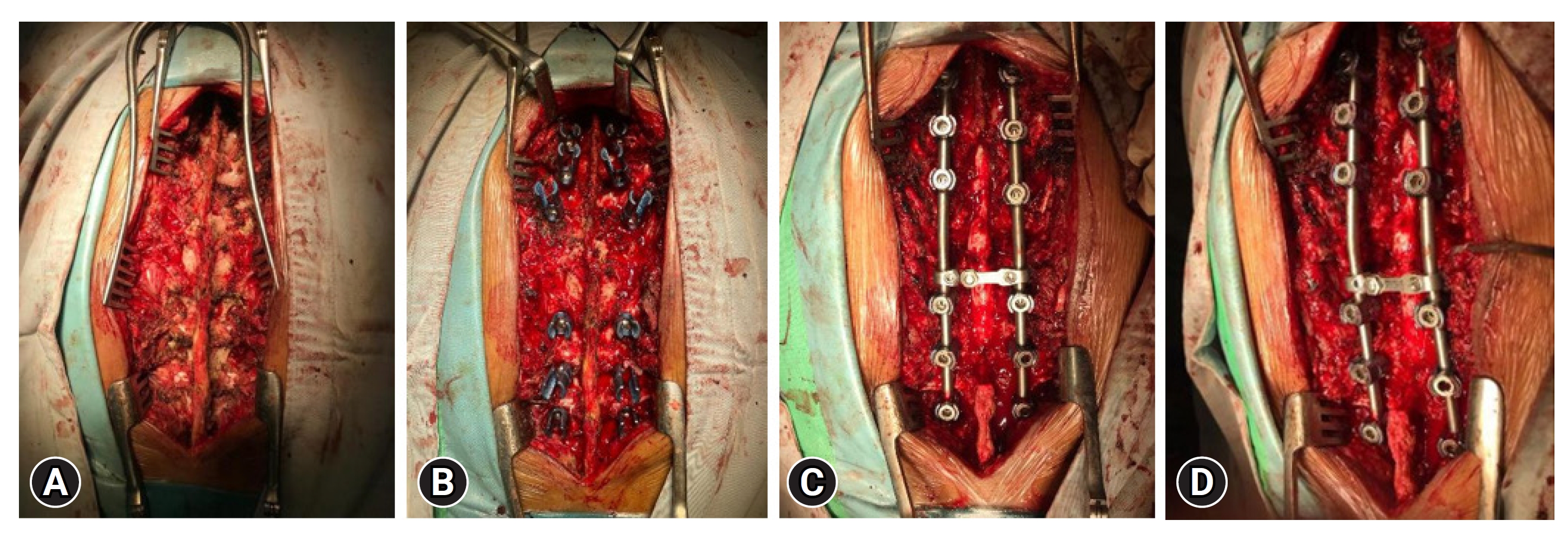
Intraoperative findings, showing the laminectomy (A), the placement of screws (B), the rod stabilisation (C), and rod bent (D) to match appropriate angulation.
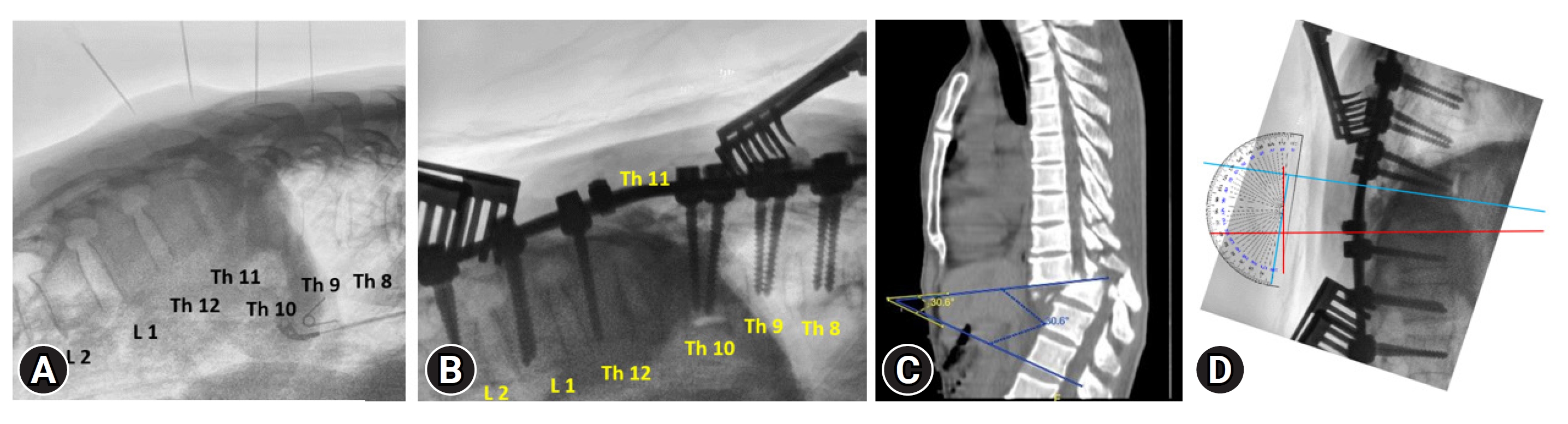
Intraoperative findings on C-arm, showing the spondyloptosis prior to correction (A), screws being placed (B), spondyloptosis before correction (C), and angle of correction after rod was bent (D).
In the case of our American Spinal Injury Association Impairment Scale (AIS) grade A patient with traumatic spondyloptosis, the decision to fuse 7 vertebral levels during surgery was driven by several crucial considerations, supported by existing literature. First and foremost, the severity of the SCI, denoted as AIS grade A, indicated a complete loss of motor and sensory function below the level of injury. In such severe cases, the primary objective during surgical intervention is to restore spinal stability and prevent further damage. Traumatic spondyloptosis often leads to significant vertebral instability and dislocation, necessitating a comprehensive fusion construct to ensure the secure realignment of the affected segment. This longer fusion construct, spanning 7 vertebral levels, not only enhances immediate spinal stability but also reduces the risk of potential complications, such as adjacent segment disease, which can arise when there is increased stress on adjacent vertebrae in shorter fusion constructs. While the preservation of thoracic spine rotations is undeniably important for rehabilitation and activities of daily living, the primary focus in AIS-A cases is often on establishing a stable environment to prevent further neurological damage. Therefore, in our patient's case, the decision to perform a 7-level fusion was based on a careful assessment of the severity of the injury, the need for spinal stability, and the aim to minimize the risk of complications while providing a foundation for potential future rehabilitation efforts. This choice aligns with the individualized approach to patient care and reflects the balance between spinal stability and functional preservation in such challenging clinical scenarios.
Following the surgical intervention for neglected spondyloptosis at levels T10–11, the patient's postoperative journey was closely observed, encompassing their immediate recovery, subsequent clinical follow-up, and symptom improvement. The patient was vigilantly monitored in the intensive care unit for a duration of 2 days immediately after the surgery. This critical phase allowed for continuous assessment of vital signs, neurological status, and wound healing, ensuring the patient's stability and well-being in the early postoperative hours. Subsequently, the patient was transferred to the general ward, where they underwent a 5-day recovery period under ongoing medical supervision. During this period, pain management, rehabilitation, and patient education were prioritized to facilitate the initial stages of recovery. One week after discharge from the hospital, the patient returned to the clinic for a scheduled follow-up appointment. This appointment played a pivotal role in assessing the patient's progress and response to the surgical intervention.
DISCUSSION
SCI is a neurological condition in which the spinal cord is damaged. The annual incidence of SCI reaches 15–40 cases per million people worldwide. Etiology can be divided into traumatic and nontraumatic etiologies [7,8]. Trauma is responsible for >90% of SCI incidences. The incidence of traumatic SCI was higher in males by a 2:1 ratio. The age distribution is bimodal, with the first peak affecting young adults (around 30 years old) and the second peak above 60 years of age. In the thoracic spine, the stabilizing effect of the associated rib members provides some stability and limits the degree of dislocation more commonly seen in the relatively mobile cervical spine. However, the thoracolumbar junction may be more prone to dislocation because the relatively fixed thoracic segment is connected to the mobile lumbar spine [2,9].
Traumatic spondyloptosis is a rare medical condition defined as subluxation of ≥100% of a vertebral unit beyond the lower unit in the sagittal or coronal plane following high-energy trauma such as a traffic accident or fall from height. This medical condition is classified as a highly unstable injury. Most commonly, thoracic spondyloptosis occurs in the sagittal plane, with the upper vertebral bodies usually seen in front of the lower vertebral bodies. Posterior and lateral spondylolisthesis are rarely described in the literature [10-12]. The etiology of this ailment exhibits a spectrum of contributing factors, including perinatal trauma, congenital malformations, calcified defects in the pars interarticularis, neoplastic pathologies like neurofibromatosis or aneurysmal bone cyst, as well as traumatic incidents such as vehicular collisions or diving-related trauma. Frequently, spinal cord compromise arises from the malpositioning of adjacent vertebral bodies [13].
A study by Mishra et al. [13] is the largest case series in the literature, including his 8 cases (50% sagittal, 50% coronal) of traumatic thoracic spondyloptosis. All cases were AIS grade A on admission and were treated with pedicle screws. The second largest case series included his 3 patients with thoracic spondyloptosis. Chandrashekhara et al. [14] treated an AIS grade A patient with a T11–12 fracture dislocation with pedicle screws and rod fixation, but no neurological improvement was reported. Sekhon et al. [6] reported a case of traumatic thoracic spondyloptosis with complete SCI that underwent vertebral reduction and posterior stabilization. In 4 case reports, a patient with AIS grade A did not show neurological improvement after surgical treatment. Study by Gitelman et al. [15] presented the case of a neurologically intact young man involved in a motor vehicle accident with T6–7 spondyloptosis. He was treated on his 3-month bed rest, after which a delayed in situ fusion was performed while preserving his neurological function.
Management of spondyloptosis has the goals of reduction, adjustment, and stabilization. Early surgery with reduction and stabilization is preferable to conservative treatment. The surgical approach can be done anteriorly, posteriorly, or in combination with no significant difference. For paraplegic patients, the goal of surgery is early mobilization and rehabilitation [15,16]. Surgical management of reducible spondyloptosis typically includes an open posterior approach and distraction between segmental pedicle screws in the sagittal plane to create sufficient reduction force to restore alignment. A vertebral resection (vertebrectomy) removes a body part of the spine to relieve pressure on the spinal cord. A recent study by Lee et al. [4] reported the case of a 37-year-old man with a T3–4 posterior dislocation resulting in complete paraplegia. Patients were treated with controlled sequential sagittal distraction and unlocking anteroposterior shear reversal, and open reduction using horizontally aligned temporary rods to facilitate alignment restoration [17].
In this case, the surgical approach used is the posterior approach. A study showed there is no significant difference between the anterior approach, the posterior approach, and both approaches. However, another recent study found that patients undergoing an anterior approach were at increased risk of hospitalization costs, length of stay, and postoperative complications such as mortality, wound dehiscence, hematoma/seroma, and adhesion failure [16]. The posterior approach is also used more frequently in surgical procedures. In addition, comorbidities play an important role in the successful fusion outcome and have different implications depending on the surgical approach. Increased due diligence in patient selection should be considered when choosing an approach in preoperative planning [18,19].
The findings from this case contribute significantly to the existing body of literature in several ways. Firstly, it addresses a rare and challenging clinical scenario: traumatic spondyloptosis at the thoracic level, which is a severe form of SCI associated with a high degree of vertebral instability. While there are case reports and small case series documenting spondyloptosis in various contexts, our manuscript provides a comprehensive analysis of a neglected spondyloptosis case at levels T10–11. Neglected cases of spondyloptosis are particularly rare and present unique clinical challenges, making our case an important addition to the literature.
This case highlights the critical role of surgical intervention in managing traumatic spondyloptosis, emphasizing the need for early reduction, realignment, and stabilization. This aligns with recent trends in SCI management, where early surgical intervention has shown promise in improving clinical outcomes. We discuss the various surgical approaches and techniques employed, including laminectomy decompression, bilateral facetectomy, and partial vertebrectomy, shedding light on the intricacies of the surgical process in such complex cases. Furthermore, it underscores the decision-making process regarding the extent of fusion in an AIS grade A patient with traumatic spondyloptosis. We provide a detailed rationale for the fusion of 7 vertebral levels, considering factors such as spinal stability, complications, and the potential for future rehabilitation. This decision-making aspect is often underrepresented in the literature but is of great significance in guiding clinical practice.
We also offer insights into the evolving landscape of SCI management, incorporating recent findings and recommendations. By combining a detailed case report with a thorough analysis of surgical techniques and decision-making, our manuscript serves as a valuable resource for clinicians, neurosurgeons, and researchers specializing in spinal cord injuries. It not only enriches the existing literature on spondyloptosis but also provides a reference point for the multidisciplinary management of severe spinal cord injuries.
CONCLUSION
Thoracic spondyloptosis is a very rare but severe case of SCI. Neurological deficit is common in this case. Early management in reduction and stabilization is generally recommended in cases to obtain a better outcome. Although previous studies mentioned no significant difference from the surgical approach, recent studies showed that patients undergoing an anterior approach were at increased risk of hospitalization costs, length of stay, and postoperative complications such as mortality, wound dehiscence, hematoma/seroma, and adhesion failure.
This manuscript contributes significantly to the literature by presenting a rare case, elucidating surgical intricacies, addressing decision-making in complex scenarios, and aligning with contemporary approaches to SCI management. It serves as a comprehensive reference for both clinicians and researchers, advancing our understanding of and approach to traumatic spondyloptosis.
Notes
Conflicts of interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.