Anterior Percutaneous Endoscopic Cervical Discectomy, a Stitchless and Bloodless Surgery: Clinical and Radiological Results
Article information
Abstract
Objective
Anterior cervical discectomy with fusion [ACDF] has been considered gold standard for cervical disc herniation over period of time. Anterior percutaneous endoscopic cervical discectomy [PECD] is minimally invasive technique without need for implant or bone graft in properly selected cases. In this study we present clinical and radiological results of anterior PECD.
Methods
We retrospectively studied 31 patients treated with anterior PECD in our institute from January 2014 to December 2016. Patients’ clinical data, visual analogue score [VAS], neck disability index [NDI] and radiographs were collected. Cervical lordosis angle, focal angle and disc height of involved segment were measured using Medsynapse software. Statistical analysis was performed using paired T test, chi square test.
Results
There were 18 males, 13 females in this study. Mean follow up period was 28.5 months. VAS for neck pain reduced from 6.2±0.72 to 1.67±0.59; VAS for arm pain reduced from 7.25±0.71 to 1.5±0.61 at final follow up. NDI reduced from 64.7±7.62 to 13.48±5.42 at final follow up. Mean disc height of involved segment was 6.15 mm pre-operatively which reduced to 5.24 mm at final follow up showing reduction of 0.91 mm. This reduction is disc space is not clinically significant as VAS and NDI show significant fall. Cervical lordosis was well maintained which changed from 13.93°±3.7° to 15.58°±6.66°; [p-value is 0.060]. Pre-operative focal cervical angle of involved segment was 0.86°±1.66° which increased to 1.7°±1.81° at final follow up [p-value 0.0067]. Twenty out of 31 patients resumed their previous employment within 2 weeks.
Conclusion
Anterior PECD is excellent minimally invasive technique for cervical disc herniation in properly selected cases. Patients have good functional and clinical recovery after this procedure.
INTRODUCTION
Anterior cervical discectomy with fusion [ACDF] using bone graft or a spacer has been considered gold standard treatment for cervical disc herniation over the period of time [1,2]. There has been fear that without reconstructing disc space, cervical spine will become kyphotic with distortion of alignment and neural foramen compromise, leading to axial neck pain and delayed radiculopathy. But enough evidence exists that in properly selected cases even without fusion, cervical kyphosis and delayed radiculopathy do not occur and very few cases require delayed fusion [3-5].
Anterior percutaneous endoscopic cervical discectomy [PECD] preserves majority of anterior and central disc, anterior longitudinal ligament, both endplates and facet joints with selective evacuation of offending fragment. This reduces damage to surrounding tissues, bones and ligaments. Thus prevents subsequent malalignment, instability and other approach related complications [6].
During this procedure there is minimal blood loss and less muscle trauma. It can be done under local anaesthesia. Hence, patient can be discharged on the next day of surgery reducing hospital stay. There is no need for expensive implants. These factors help in reducing cost of surgery.
Anterior PECD can be performed under local anaesthesia with sedation. Therefore, it can be performed for patients who are not fit for general anaesthesia due to medical reasons. Another benefit of having the patient awake is that the patient can give feedback during surgery which serves like live neuromonitoring.
Anterior PECD has evolved rapidly, but there are very few studies demonstrating its clinical and radiological effects. In this study, we present clinical and radiological outcome of patients treated with anterior PECD using working channel endoscopes and microforceps.
MATERIALS AND METHODS
1. Patients
We retrospectively studied all patients treated consecutively with anterior PECD from January 2014 to December 2016 in our institute. Thirty one patients were operated with anterior PECD during this period. Patients having neck pain and or cervical radiculopathy, soft disc herniation, corroboration of clinical and radiological picture as seen on MRI, failed conservative treatment at least for 6 weeks, disc height more than 4 mm, craniocaudal migration of disc less than half the distance of vertebral body and no previous history of neck surgery were included in this study. Patients having calcified sequestered disc, cervical myelopathy, segmental instability, bilateral symptoms, severe central canal stenosis, no clinic-radiological correlation and history of previous neck surgery were excluded.
Patients’ clinical data, pre-operative and post-operative visual analogue score [VAS], neck disability index [NDI] score were collected. Cervical spine AP, lateral, flexion and extension radiographs were obtained. Angle of cervical spine, focal angle and disc height of involved segment were measured using Medsynapse software [Medsynaptic Private Limited, Pune, India].
2. Statistical Analysis
Statistical analysis was done using paired T test, Chi square test.
Cervical angle was measured by angle between line drawn parallel to inferior end plate of C2 vertebra and another line drawn parallel to inferior end plate of C7 on lateral radiograph.
Focal angle of involved segment was measured by angle formed by lines drawn parallel to inferior end plate of cephalad and caudal vertebra. Lordotic angle was designated a positive value while kyphotic angle was designated a negative value.
3. Surgical Procedure
Patient was kept in supine position with head ring under head with neck in slight extension, shoulders pulled down, cervical block and sedation was given to minimise pain and anxiety. Approach on neck is taken from opposite side of upper limb having radicular pain. Local anaesthesia [5 mL 0.25% Bupivacaine + 5 mL 2% lignocaine] was given after marking level under image intensifier.
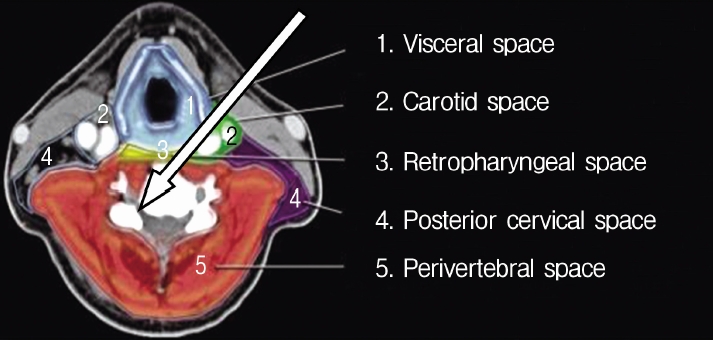
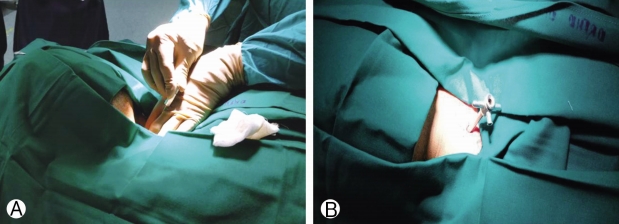
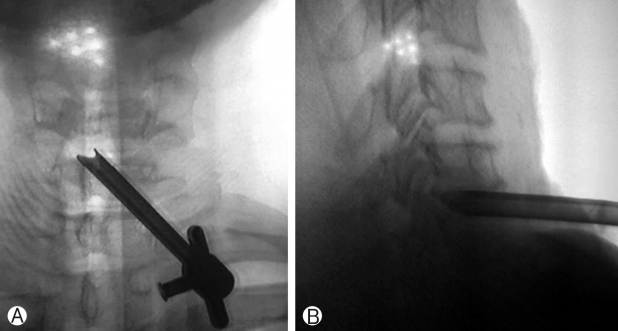
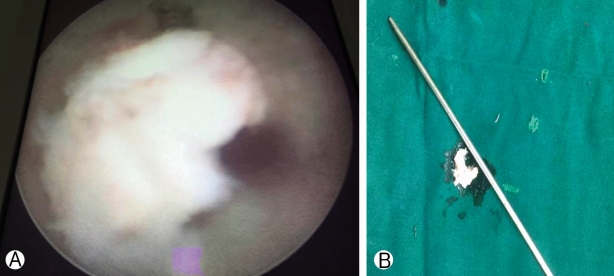
Compartmentalisation of anatomical structures in neck helps in the approach (Fig. 1). With left hand middle finger, the surgeon displaces trachea and oesophagus towards opposite side and palpates carotid pulse with index finger and displaces it laterally (Fig. 2). This way anterior aspect of vertebral body is reached. Needle with stellate is passed and disc is pierced in midline. This preserves central disc as the trajectory of the needle is oblique and angle depended on position of disc whether central, paracentral or foraminal. Once needle is in disc indigocarmine is injected. Needle is advanced till posterior aspect of vertebral body under image intensifier guidance. Stellate of needle is exchanged with guide wire, 3-5 mm transverse incision is taken, serial dilators are passed and finally camera sheath [cannula] is passed. Its position is confirmed under image intensifier in AP and lateral view (Fig. 3); endoscope [Karl Storz with 2.5 mm working channel] is inserted through sheath (Fig. 4). Operative space is continuously irrigated with sterile saline which is connected to endoscope.
Using endoscopic forceps and hooks offending fragment is freed and removed. Space for nerve root is restored. Platelet rich fibrin plug was inserted after completion of procedure as there is evidence that it alleviates pain and helps in annular healing [7-9]. After procedure sterile dressing is applied without stitch.
This procedure can be performed for C3-C4 to C6-C7 discs.
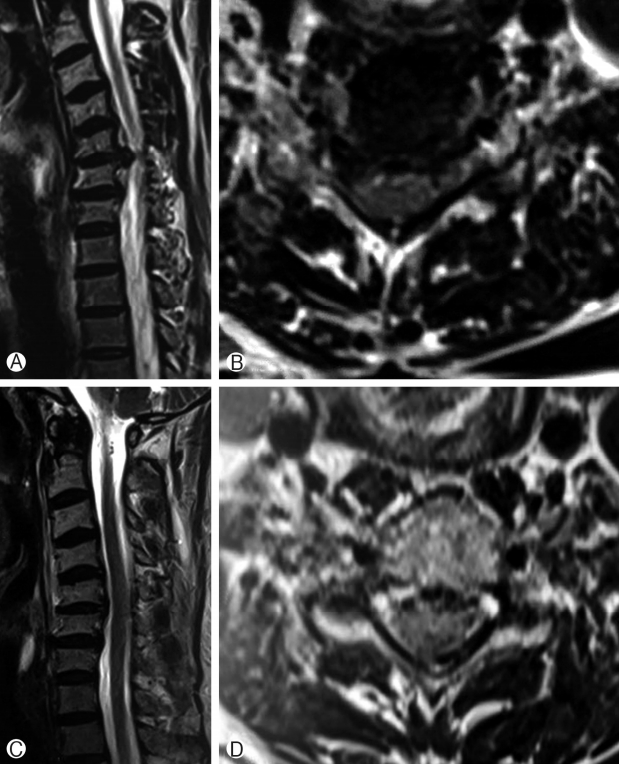
Post-operatively patients were given soft cervical collar and were discharged one day after surgery. Patients were followed up after 10 days, at 6 weeks and every 3 months thereafter. During each follow up, radiographs of cervical spine AP, Lateral, flexion and extension views were taken; VAS, NDI score were recorded. MRI was advised after 3 to 4 of surgery months after surgery (Fig. 5).
During post-operative and follow up period we were vigilant for complications like no or incomplete relief, neurological deterioration, radicular pain, CSF leak, infections, hematoma formation, dysphagia, delayed radiculopathy, spontaneous or delayed fusion and revision surgery.
This study was approved by our institutional review board.
RESULTS
During January 2014 to December 2016, a total of 31 patients were operated with anterior PECD. There were 18 males and 13 females. Average age of patients was 38 years, ranging from 25 to 61 years. Mean follow up period was 28.5±10.1 months. C3-4 level was operated in 3 cases, C4-5 in 6 cases, C5-6 in 14 cases and C6-7 in 8 cases. Central disc herniation was present in 4 patients 14 had paracentral disc herniation while 13 had foraminal disc herniation.
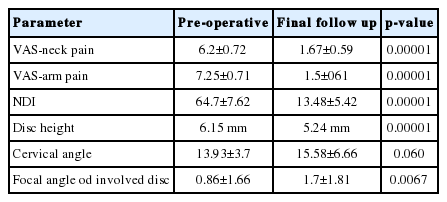
Pre-operative VAS for neck pain was 6.2±0.72 and at final follow up it was 1.67±0.59 [p-value=0.00001]. Pre-operative VAS for radicular upper limb pain was 7.25±0.71 and at final follow up was 1.5±0.61 [p-value=0.00001] (Table 1). NDI score preoperative was 64.7±7.62 and at final follow up was 13.48±5.42 [p-value=0.00001] (Table 1).
Mean disc height of involved segment was 6.15 mm pre-operatively which reduced to 5.24 mm at final follow up. There is mean reduction of 0.91 mm in disc height with p-value=0.00001. Though there is reduction in disc height, VAS and NDI also show significant fall which indicate that this reduction in disc height is not clinically significant.
Patients’ pre-operative cervical angle improved from 13.93°±3.7° to 15.58°±6.66° at final follow up [p-value is 0.060] and overall lordotic angle was well maintained.
Pre-operative focal cervical angle of involved segment was 0.86°±1.66° which increased to 1.7°±1.81° at final follow up which is statistically significant [p-value 0.0067]. There was no segmental instability noted on flexion extension radiograph. These results have been summarised in Table 1.
Twenty patients having desk jobs resumed their previous employment within 2 weeks, and remaining by 5 weeks.
Thirty patients were satisfied with the procedure. One patient was unsatisfied as he had persistent symptoms after surgery [Pre-operative VAS for arm pain and neck pain was 7 and 5, Post-operative it was 6 and 5] probably due to incomplete decompression. He was operated with ACDF two months after anterior PECD. No patient required delayed fusion procedure.
There were no complications like mortality, post-operative infection, neurological deterioration, hematoma formation, dysphagia, CSF leak, spontaneous fusion.
DISCUSSION
This study presents results of 31 patients treated with anterior PECD which shows fall of VAS and NDI after surgery. Cervical lordosis angle is well maintained with 0.91 mm fall in disc height of operated level post-surgery.
Surgeons strive to achieve better results day by day and try new techniques, which drives them to incorporate minimally invasive surgery [10]. Success of percutaneous endoscopic lumbar discectomy has encouraged surgeons to perform percutaneous endoscopic decompression for cervical disc herniations [11-13]. Minimally invasive cervical disc surgery has evolved from procedures like percutaneous fluoroscopy guided disc decompression, automated nucleotomy [14], percutaneous cervical disc decompression using chemonucleosis [15], percutaneous laser decompression [12,16]. But these were blind procedures without direct visualisation. In today’s era development of cervical endoscope has improved fineness of percutaneous cervical disc surgery due to direct visualisation.
When we go through literature we find that majority of improvement in cervical disc surgery resolves around development of newer implants to be inserted in empty disc space after discectomy. There is lack of clarity about sufficiency of anterior cervical decompression without fusion [ACD]. Whether fusion is really necessary to preserve disc space height and whether disc height maintenance is important for good clinical outcome is unclear [3-5,11,14].
Total volume of cervical disc is much less than that of lumbar disc. Cervical nerve root is confined to a smaller space than lumbar nerve root, therefore, a small volume reduction in cervical disc herniation produces a much greater effect [17].
Yong et al. [16] studied 36 patients treated with anterior percutaneous cervical discectomy. They found that mean disc height reduction after anterior PECD was 0.8 mm after 24 months follow up. In a study by Ruetten et al. [18] mean disc height reduction after anterior endoscopic cervical discectomy was 1.1 mm after 24 months follow up, while Yadav et al. [19] found that disc height reduction was 1.1 mm after anterior PECD. In our cases mean disc height reduction was 0.91 mm after 28.5 months of follow up period.
Incidence of spontaneous fusion in ACD is 4% to 74% [5,20-22]. Although there is reduction in disc height complete disc space collapse and fusion is not reported after anterior PECD [16].
In percutaneous cervical endoscopic discectomies done by Ahn Y et al. [16] VAS reduced from 8.78±1.6 pre-operative to 2.75±2.5 post-operatively. In a study by Parihar et al. [23] VAS for arm and neck pain improved from 6.7 and 3.2 to 1.7 and 1.1 respectively. In our study VAS for neck pain was 6.2±0.72 and at final follow up it was 1.67±0.59 and VAS for radicular upper limb pain was 7.25±0.71 and at final follow up was 1.5±0.61.
Even though there is disc height reduction, VAS and NDI show significant fall in our study which shows that there is no relationship between disc height reduction and clinical outcome, as shown by many other studies too [16,17,23].
It has been found that sizable numbers of patients develop cervical alignment disruption after open ACD. In a study by Laing et al. [24] postoperative loss of overall lordosis was found in 54.5% of patients and segmental kyphosis was seen in 32.7% of patients. There is evidence that immediate loss of lordosis after open ACD is corrected with time but still 10-20% patients remain kyphotic. In a study by Yong et al. [16] pre-operative overall cervical lordosis was 15.78°±8.01° which post-operatively became 16.00°±8.06°and focal lordotic angle of treated level preoperative was 0.36°±4.29° which improved to 2.33°±3.55°. Yadav et al. [19] found that mean pre-operative lordotic angle changed from 6.3° to 6.1° after surgery and mean focal angle of involved segment changed from 2.1° to 2.0°.
In our study this change of cervical angle was from 13.93°±3.73° pre operatively to 15.98°±6.66° post-operatively. Thus, overall cervical lordosis was well maintained. This change is not statistically significant [p-value 0.06]. Focal lordotic angle of treated level increased from 0.83°±1.66° to 1.7°±1.81° which is statistically significant with p-value 0.0067. The cause for maintenance of lordotic angle can be preservation of anterior structures like longus coli, anterior longitudinal ligament, and anterior annulus, most of the anterior and central disc and selective removal of herniated posterior disc. There is selective reduction posterior disc space, thus, maintaining lordosis24.
In study by Rueten et al. [18] revision rate was 7.4%, while in study by Parihar et al. [23] was 0.95%. In our study it was 3.2%. Stringent selection criteria and smaller sample size may be reasons for better results in our cases.
It has been reported that there is 3 times more risk of adjacent disc degeneration in incorrectly marked disc during ACDF [25]. This might be discouraging for endoscopic surgeons. But Hadley et al. [26] reported that in carefully selected patients only 1.5% patients need delayed fusion procedure. As stated by many studies, there is lack of correlation between disc height loss and symptoms. Thus inserting expensive implant or donor site morbidity due to bone grafting might be overdone for many cases.
Endoscopic cervical disc surgeries have longer learning curve and its application is limited to disc surgery for now. It is not recommended for advanced spondylosis with severe disc space narrowing. The success rate of anterior PECD is reported to be ranging from 51% to 94.5% [3,13,15,17].
Though PECD is rewarding, scientific evidence for this procedure is low; few randomised control trials [RCTs] are available evaluating its effectiveness.
Limitations of this study are no comparative group, fewer number of patients short period of follow up. More studies with higher number of patients with longer follow up and randomisation are needed to shed more light on effectiveness of anterior PECD.
CONCLUSION
Anterior PECD is safe and effective alternative to ACDF in properly selected cases. It has less approach related morbidity leading to lesser hospital stay and faster recovery. More studies with randomisation are needed to improve our knowledge about this procedure.
Notes
Authors declare that there is no conflict of interest.