Minimally Invasive Irrigation for Lumbar Spinal Epidural Abscess using a Trans-Sacral Epiduroscopic Laser Decompression Catheter
Article information
Abstract
We describe a case of a spinal epidural abscess that was successfully treated with minimally invasive irrigation using trans-sacral epiduroscopic laser decompression (SELD) catheter. A 66-year-old man experienced aggravating right leg pain and lower back pain for 1 month despite receiving several pain blocks at a local hospital. Magnetic resonance imaging scans showed annular fissure and bulging disc at the L4/5 level. Therefore, we decided to treat the L4/5 lesion using SELD. Laboratory studies demonstrated leukocytosis and elevated C-reactive protein level. However, we did not pay attention to the abnormal laboratory values before SELD. During SELD, we found a yellowish epidural abscess and pus drainage. Therefore, we irrigated the epidural abscess using an SELD catheter. His low back pain was relieved dramatically immediately after the procedure. The spinal epidural abscess completely resolved after 20 days of antibiotic treatment. Minimally invasive irrigation and drainage using a SELD catheter and intravenous antibiotic therapy are helpful for the treatment of spinal epidural abscess.
INTRODUCTION
The trans-sacral epiduroscopic laser decompression (SELD) technique has been widely used as an out-patient department-based procedure that can relieve symptoms without using general anesthesia in patients experiencing lumbar herniated nucleus pulposus (HNP) [6,9,11]. Endoscopy is performed through the sacral hiatus into the epidural space, and the disc can be decompressed by cauterizing the disc using laser, while directly exploring the disc at the affected area pressing the sac [10]. It is intuitive and effective for relieving pain because it allows the patient to be alert during the procedure and confirm the pain and gross findings in real time [2,4]. It is also useful in patients with multiple levels of diseases because they allow an easy access to multiple spinal levels [2]. We incidentally found a pus discharge during elective SELD in a patient who had not improved for more than 1 month despite several block procedures. Herein, we report a case of an infection managed with irrigation and drainage (I & D) using an SELD device for infectious spondylodiscitis and psoas abscess, in which the clinical symptoms rapidly improved.
CASE REPORT
A 66-year-old man presenting with lower back pain (LBP) and right knee pain lasting for more than 1 month visited a local clinic. L-spine magnetic resonance imaging (MRI) showed an L4-5-level HNP; thereafter, he underwent nerve block for several times and conservative treatment for 1 month (Fig. 1). However, the range of pain extended to the right inguinal area and shin; thereafter, he visited our outpatient clinic. The patient complained of pain at the back and radiating to right leg VAS score of 8 points. He had no axial pain during weight bearing or psoas muscle symptoms. The neurologic examination showed an alert mental status and no motor weakness. He was diagnosed with diabetes mellitus, hypertension, and cerebrovascular accident in 2009 and underwent PCI in 1997 and CABG in 1998 due to angina. We planned to perform SELD, and the patient was hospitalized on the next day after the baseline examination.
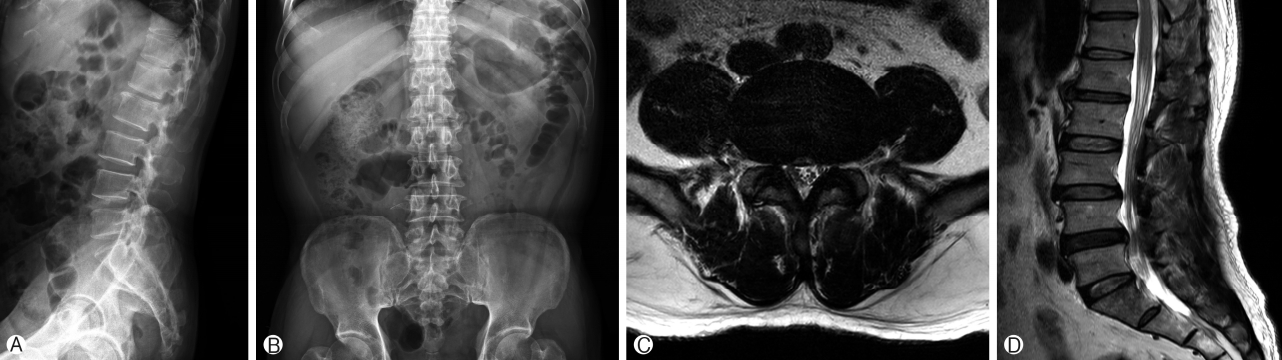
Preoperative imaging. Preoperative L-spine anteroposterior Ⓐ and lateral Ⓑ views showing posterior wedging. Preoperative L-spine magnetic resonance imaging sagittal (Ⓓ & Ⓔ) and axial Ⓒ views showing an L4-5 herniated disc protrusion inferiorly.
The patient was placed in the prone position, and the sacral hiatus was confirmed using the C-arm machine (Fig. 2A). The guide catheter was inserted, and the ruptured disc was found; laser ablation was then performed (Fig. 2B and C). During exploration of the disc, we eventually found a pus like discharge (Fig. 2D). Using the SELD device, a pus culture sample was obtained, and I & D using 1 L of saline was performed (Fig. 2D). A culture sample from the irrigated fluid was obtained, and SELD was then completed [1]. Surgical Techniques
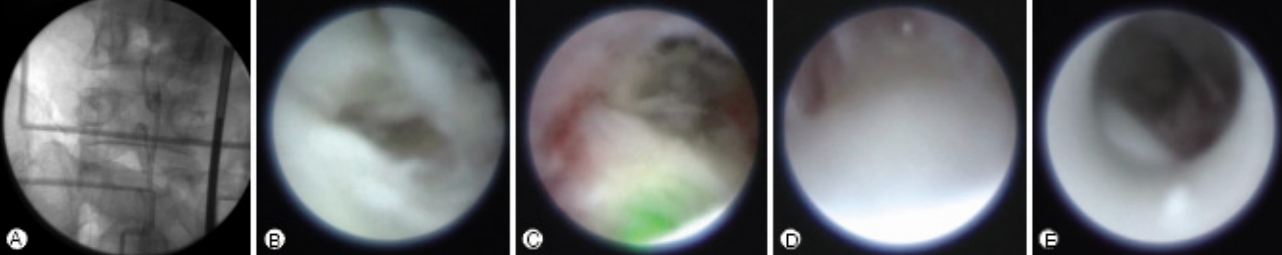
Intraoperative epiduroscopic imaging. Using a C-arm X-ray machine, we explored multiple levels of the sacrolumbar epidural space and approached the target lesion Ⓐ. Laser (Ⓑ, green light) ablation of the protruded disc. When we advanced the upper lumbar level epidural space to explore other lesions Ⓒ, the field became suddenly blurred owing to the presence of a turbid fluid Ⓓ. Thus, we drained the turbid fluid and irrigated almost 1 L of saline using the trans-sacral epiduroscopic laser decompression device Ⓔ.
Postoperative L-spine MRI scan showed infectious spondylodiscitis and psoas muscle abscess; this finding was not shown on initial MRI 1month ago. Fever at a temperature of 39.2℃ was noted. Cefazolin and vancomycin were administered as empirical antibiotics (Fig. 3A and B). At 5 days postoperatively, methicillin-sensitive staphylococcus aureus (MSSA) was identified in the pus culture sample and treated with nafcillin 2 g every 4 hours for 6 days and cefazolin 2 g every 8 hours for 8 days. His pain was relieved further, with a VAS score of 2 points. Percutaneous abscess drainage was performed at 7 days postoperatively (Fig. 3C). The preoperative examination findings were as follows: WBC, 16,000 1,000/mm3; C-reactive protein (CRP), 5.91 mg/dL; and erythrocyte sedimentation rate (ESR), 106 mm/h; at 6 days postoperatively, the follow-up test findings rapidly decreased as follows: WBC, 6,800 1,000/mm3; ESR, 59 mm/h; and CRP, 2.45 mg/dL (Fig. 4).
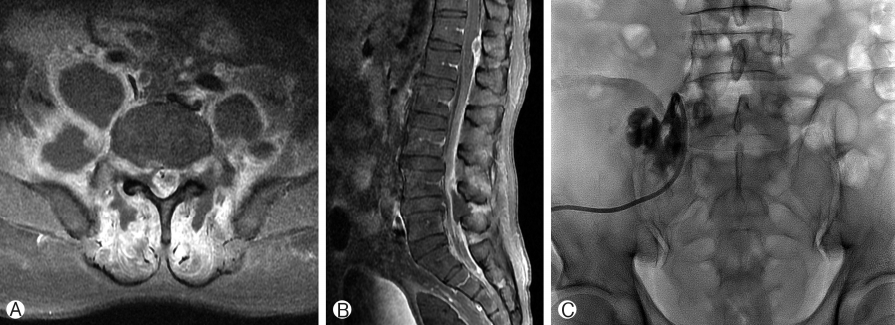
Postoperative imaging. L-spine magnetic resonance imaging scan (Ⓐ & Ⓑ) showing epidural and psoas muscle abscesses with multiple fluid-containing pockets surrounding the contrast-enhanced wall. Radiologic C-arm X-ray-guided percutaneous psoas muscle abscess drainage Ⓒ.
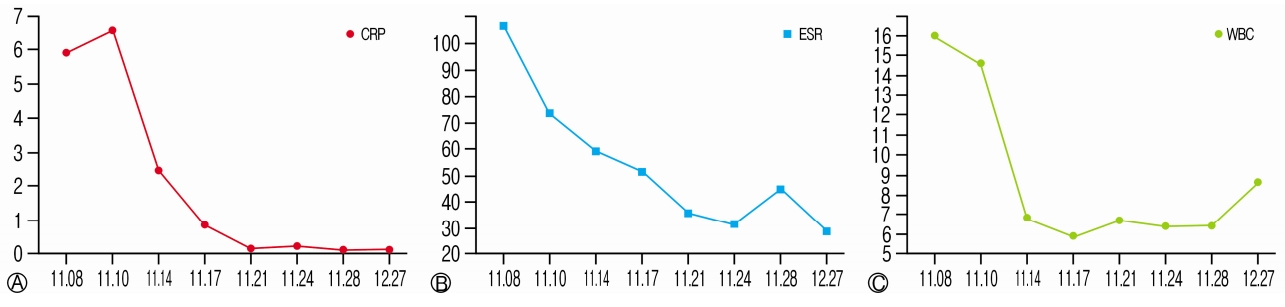
Follow-up infection marker. After operation, the marker levels declined rapidly. C-reactive protein (CRP), mg/dL Ⓐ; Erythrocyte sedimentation rate (ESR), mm/h Ⓑ; and WBC, 1,000/mm3 Ⓒ.
The patient was maintained on intravenous antibiotics and was discharged at 19 days postoperatively. The out-patient clinic follow-up laboratory findings were normal, and his pain gradually resolved.
DISCUSSION
In this case, SELD was planned as an elective procedure for the LBP of the patient, which did not respond to long-term conservative therapy. There were no significant physical or neurological findings of spondylodiscitis such as axial pain during weight bearing or psoas muscle symptom and SELD operation was underwent for L 4-5 level HNP shown initial L-spine MRI. We didn’t consider for infection initially and epidural abscess was incidentally detected during procedure. Despite the increase in the infection marker levels preoperatively, we performed SELD, and an intraoperative extrathecal pus discharge was found. After infusing a large amount of saline during I & D using the SELD device, spondylodiscitis and epidural and psoas abscesses were confirmed on L-spine MRI follow-up; antibiotics were then combined to manage the infection.
Surgical drainage together with systemic antibiotics for spondylodiscitis is the treatment of choice [8]. Conventional open I & D has been commonly used for epidural abscess; conversely, endoscopic I & D has been reported as a minimally invasive procedure [5,12]. Ito et al. reported that debridement with 2 L of saline on posterolateral endoscopy showed a CRP and VAS score improvement 1 week after surgery [5]. Yang et al. reported improvements in pain with antibiotics and performed percutaneous endoscopic debridement with 10 L of 0.35% dilute betadine solution in 32 patients with spinal infection; their patients recovered without complications [2]. Mathews et al. inserted a catheter through the sacral hiatus and obtained an epidural abscess drain and culture sample under fluoroscopic guidance [7]. In our case, I & D was performed through SELD; consequently, the patient showed a rapid recovery and continued for pain relief. Subsequent effects of the antibiotic therapy also show the effectiveness of SELD on spondylodiscitis. The addition of psoas abscess drainage after the initial treatment also shortened the disease course. Considering the abovementioned cases and our case, microbial lavage through I & D may be an important factor in the treatment of epidural abscess.
In addition, compared with percutaneous epidural neuroplasty, SELD was able to visualize the epidural space using epiduroscopy and find the epidural abscess [2]. The fact that the identified bacteria were MSSA also seemed to have led to a good prognosis [3]. For patients with a history of vulnerability to infection, such as old age, diabetes mellitus, immune-compromised host, intravenous drug use, alcoholism, liver cirrhosis, and renal failure, an attitude to identify an infection marker is required during preoperative laboratory evaluation [1].
CONCLUSION
Using a SELD catheter, minimally invasive I & D of epidural abscesses may help treat spinal infections.