Tubular Micro-Discectomy Under Local Epidural Anaesthesia: A Technical Note
Article information
Abstract
Objective
Day-care surgery maximizes utilization of healthcare and aids in early return to work. Minimally invasive spine surgery (MISS) under local epidural anesthesia is a step in this direction. The combination of minimal surgical trauma and nominal sedation results in quick recovery and early discharge. To present our experience of performing lumbar tubular micro-discectomy under local epidural anaesthesia.
Methods
A case report of 10patients operated for lumbar herniated discs under local epidural anaesthesia. The patients had radicular pain since a few months with MRI evidence of herniated nucleus pulposus and failure of 6 weeks of conservative trial before surgery. The outcomes were assessed with ODI, VAS and Mac-Nab criteria. Premedication with Dexmedetomidine, local infiltration of lignocaine and bupivacaine with bolus dose of fentanyl during root manipulation facilitated the execution of the procedure.
Results
All patients obtained dramatic pain relief postoperatively. The procedure was well tolerated except for the slight discomfort during varying degrees of nerve-root retraction. Patients were made to walk and oral diet allowed after an hour and discharge was within 24 hours of the procedure. The VAS improved from 8.4 to 2.3 and ODI from 58.2 to 22.8. Follow-up was at 1, 6, 12 and 24 weeks. No complications such as dural tear, nerve root injury etc. were seen.
Conclusion
Microtubular discectomy under local epidural anaesthesia is a feasible option in experienced hands. Apart from reducing the effects of general anaesthesia, it reduces the hospital stay and cost. It is an evolution of microtubular discectomy towards day care surgery.
INTRODUCTION
Daycare surgery maximizes the utilization of healthcare and promotes early return to work [4,12,15]. Minimally invasive spine surgery (MISS) under local epidural anesthesia is a step in this direction. The combination of minimal surgical trauma and nominal sedation results in quick recovery and early discharge [1]. The authors present their experience of performing tubular lumbar micro-discectomy (MED) under local epidural anesthesia.
MATERIALS AND METHODS
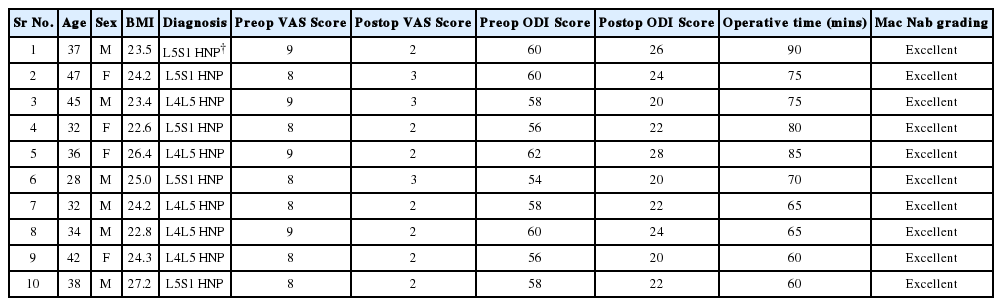
Ten patients underwent MED for lumbar disc herniation under local epidural anesthesia with mild sedation. The patients had radicular pain since a few months and were given at least 6 weeks of conservative trial before surgery. The demographic data of the patients in terms of age, sex, involved dermatome and BMI were recorded (Table 1). VAS and ODI were noted pre and post-operatively. The MRI films were reviewed to determine the level, side, size and location of the herniation. Postoperatively, all patients were mobilized the same day and discharged the following day. Mac-Nab criteria was utilized to assess the outcome.
OPERATIVE TECHNIQUE
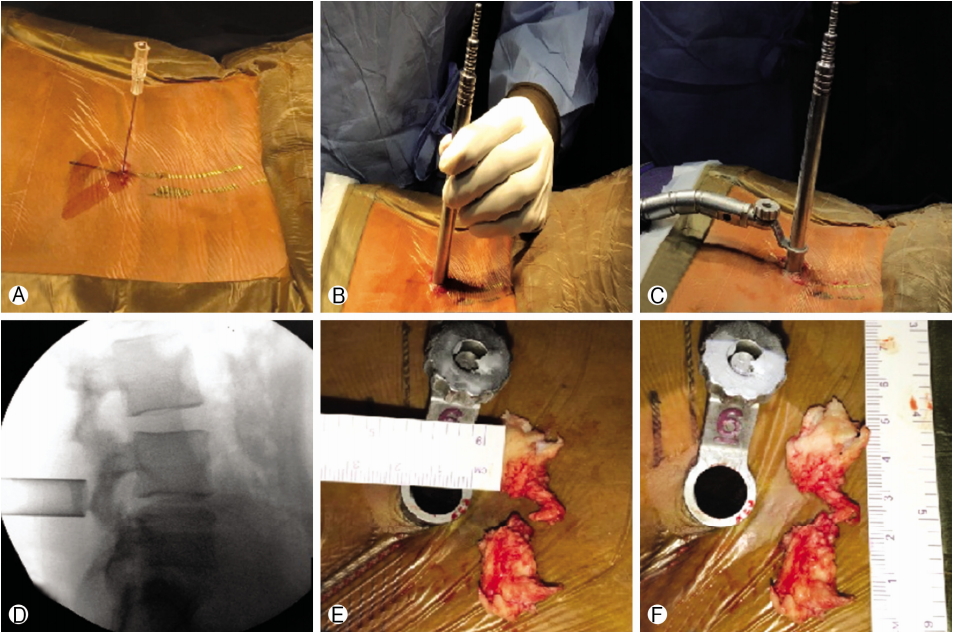
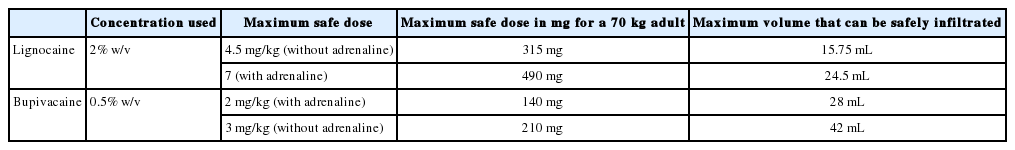
It is necessary to keep the patient nil by mouth for at least 4 hours before the procedure. In the preoperative room, the patient is pre-medicated with a Dexmedetomidine infusion 15-20 minutes before the procedure in a loading dose of 1 μg/kg. 15 minutes later the infusion is tapered to 0.2 μg/kg/hr and continued throughout the procedure [9]. It is necessary to monitor the pulse, heart rate, ECG and blood pressure. In the operation theatre, pillows are used instead of bolsters for cushioning. The patient is properly counseled regarding the procedure. The patient is made to lie prone on the operating table with head turned to one side for comfort. Music is played to relax the patient and dampen the noise of the operating room. The operative level is localized under C-Arm. A mixture of 10 cc of 2% lignocaine and 10 cc of 0.5% bupivacaine is used for local infiltration using a 23 G spinal needle, such that the trajectory of the needle bisects the intervertebral disc. Appropriate targeting of the laminotomy site during infiltration is imperative. The skin, soft tissue and periosteum is infiltrated with the mixture. After incising the skin with a 14-16 mm long incision at a site about 1 cm paramedian centered over the point of entry of the infiltration needle, serial dilators are inserted followed by docking of appropriately sized tubular retractor. The infiltration allows painless drilling of the lamina to create a bony window. The ligamentum flavum handling doesn’t cause discomfort to the patient. After the laminotomy, flavotomy is done and the dura with nerve root is exposed. At this stage, two crucial steps are application of a gelfoam soaked in 2% lignocaine over the nerve root and dura and Instant intravenous injection of Fentanyl 100 mcg. It is necessary to wait for a few minutes for the local anesthetic to act. Gentle manipulation of the nerve root is essential. Herniated fragment is then fished out using a nerve hook and pituitary forceps. The wound is then closed with absorbable sutures (Fig. 1).
RESULTS
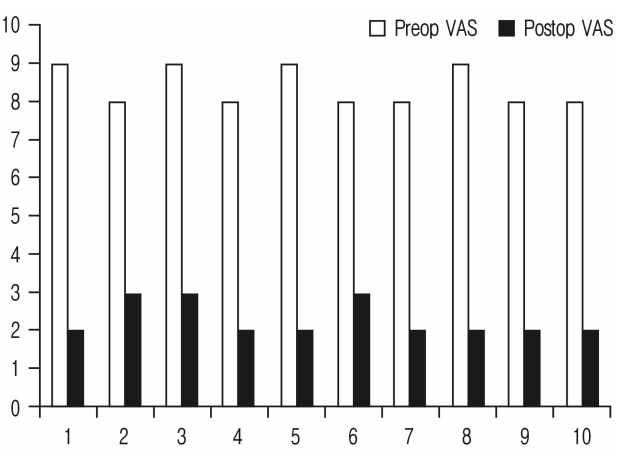
All patients experienced dramatic pain relief post-operatively. The procedure was well tolerated except for the slight discomfort felt during varying degrees of nerve-root retraction. The mean VAS improved from 8.4 to 2.3. ODI improved from a mean of 58.2 to 22.8 (Fig. 2)(Table 1). No complications such as dural tear, nerve root injury, wound infection etc. were seen. All patients were made to walk and have oral nutrition within an hour post-surgery. Mild analgesics were required to counteract the post-operative pain. The patients were discharged within 24 hrs of the procedure. The benefit was sustained in the post-operative period at 1, 6, 12 and 24 weeks.
DISCUSSION
Use of local anaesthesia in spine surgeries dates back to 1926, Towne reported 4 laminectomies for tumour removal under local anaesthesia [16]. Most articles mention the use of local anaesthesia for spine surgeries in high risk subjects (ASA class iii and iv) [10]. In the modern era, local anaesthesia in spine surgeries is generally used for Trans-foraminal endoscopic discectomies [5,11,14]. According to our knowledge, there are only few reports of the use of local epidural anaesthesia in MED. Pharmacological innovations and MISS have made the idea of day care spine surgery conceivable. The patient is pre-medicated with Dexmedetomidine. It is a selective α2-adrenoreceptor agonist [8]. It has sedative and analgesic properties with short duration of action. Unlike opioids and other sedatives like propofol, it achieves its effect without causing respiratory depression. Dexmedetomidine induces sedation by decreasing activity of noradrenergic neurons in the locus ceruleus in the brain stem, thereby increasing the activity of inhibitory gamma-aminobutyric acid (GABA) neurons in the ventrolateral preoptic nucleus. In contrast, other sedatives like propofol and benzodiazepines directly increase activity of GABA neurons. Sedation by Dexmedetomidine emulates natural sleep. Dexmedetomidine has less amnesia compared to benzodiazepines and also has analgesic effects at the spinal cord level and other supraspinal sites. The recommended dose of the same is 1 μg/kg stat over 15-20 mins followed by 0.2 μg/kg/hr [2]. Dexmedetomidine is known for its arousable sedation without respiratory depression. It also does not alter the cardiovascular system and maintains hemodynamic stability [2]. Overdose may cause bradycardia and hypotension [7]. It is important to know the maximum permissible dose of lignocaine and bupivacaine for local infiltration (Table 2) [13]. Overdose of lignocaine can cause seizures, respiratory depression and ventricular rhythm abnormalities and that of bupivacaine can cause cardio toxicity [3,6]. It is important to counsel the patient before starting the procedure. This is particularly important in MED as the tubular retractor is fixed to the operating table. Sudden unanticipated movements of the patient after tube docking can alter the position of the tube and, in unfortunate cases, may run the risk of damaging the neural structures. Hence it is necessary that the patient is compliant and remains still during the procedure. It is important for the surgeon to execute the procedure swiftly, since prone position is uncomfortable for prolonged periods. The familiarity with the use of tubes, microscope and the art of meticulous hemostasis cannot be underestimated. Diligent and tactful use of burr to create laminotomy adjacent to the site of herniation is crucial since time is valuable in such cases. Inappropriate delays in sorting instruments and solving technical hitches only increases patient discomfort. It is important that the scrub nurse and the surgical assistant are scrubbed in before the patient is positioned. It is imperative that all the necessary instruments are ready over the trolleys, the C-Arm and the microscope are draped and the necessary drugs and disposables required for infiltration are ready before the patient is positioned. It is necessary to continuously interact with the patient during the procedure and caution him/her whenever a painful stimulus is anticipated. It is also necessary to use heating devices to maintain a comfortable environment for the patient. Execution of MED under local epidural anaesthesia works similar to a wakeup test as the movements can be easily assessed. This prevents the surgeon from excessively manipulating and/or damaging the root, thus providing real time monitoring of the same.
CONCLUSION
MED in local epidural anaesthesia is a feasible option in experienced hands. A team effort is imperative to streamline the course of action and increase the operational efficiency. It helps in reduction of adverse effects of general anaesthesia, hospital stay and cost. Our technique can be considered as evolution of MED towards day care surgery.
Notes
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper