Cardiac Perforation Caused by Cement Embolus after Cement-Augmented Pedicle Screw Instrumentation: A Case of Report
Article information
Abstract
Cement-augmented pedicle screw instrumentation (CAPSI) is a widely used surgical technique in posterior spondylodesis of osteoporotic patients. Complications related to cement leakage after CAPSI was rarely reported compare to that of vertebroplasty, kyphoplasty and most of them are asymptomatic. Herein the authors report the case of a 67-year-old female who experienced cardiac perforation by string shape cement embolus after CAPSI. She underwent the foreign body removal operation through the 5th intercostal thoracotomy and she was well recovered consequently. Surgeons should be aware of this complication entity when encounter postoperative chest pain to avoid fatal results. The authors also reviewed the case reports for cardiac perforation by cement embolus and preventive modalities for the cement leakage.
INTRODUCTION
As the proportion of elderly individuals in the population increases, the demand for surgical management for osteoporotic patients with poor bone quality has also increased. Pedicle screw insertion in osteoporotic vertebra has become a prevalent challenge. To overcome this issue, cement augmentation of pedicle screw insertion (CAPSI) has been proposed as a feasible surgical technique. Cement augmentation not only facilitates optimal fixation strength but also enhances the density of the instrumented vertebral body, thereby preventing further subsidence of the vertebral body and kyphotic deformity progression [9]. However, there are several complications related to cement insertion such as cement leakage through a nearby venous system. The incidence of pulmonary cement embolism following vertebroplasty or kyphoplasty was reported to be 3.5-23% and most cases are asymptomatic [17]. Unlike the complications from cement leakage into the basivertebral veins, leakage into segmental veins was reported to be related to more systemic and severe complications like cardiac perforation [31]. Herein, we report a rare case of cardiac perforation by a string shaped cement embolus after CAPSI.
CASE REPORT
1. History and Examination
A 67-year-old woman visited the outpatient clinic due to persistent severe back pain and left sciatica with a pain intensity of 8 on the visual analog scale (VAS) over a period of one year. She had a 30-minute walking limit due to neurogenic claudication. Suspecting spinal stenosis, we performed simple tomography (X-ray) on the lumbar region and there was an obvious grade one degenerative spondylolisthesis with dynamic instability on L4-5 (Fig. 1Ⓐ). Magnetic resonance imaging (MRI) and computed tomography (CT) were performed for further evaluation and showed spinal stenosis on L3-4-5 with left central intervertebral disc extrusion on L3-4 and vacuum discs on L3-4-5-S1 (Fig. 1Ⓑ, Ⓒ, Ⓓ). We decided to manage her conservatively initially and prescribed oral analgesics and physical therapies. She also underwent left L4-5 root blocks with epidural blocks twice. Her pain was relieved and she could walk for more than 2 hours. However, her pain relapsed after 7 months and persisted after additional epidural blocks. Therefore, we decided to perform unilateral laminectomy and bilateral decompression with discectomy on L3-4 and anterior lumbar interbody fusion on L4-5. On preoperative evaluation, osteoporosis was confirmed by a T-score of -2.5 on bone densitometry.
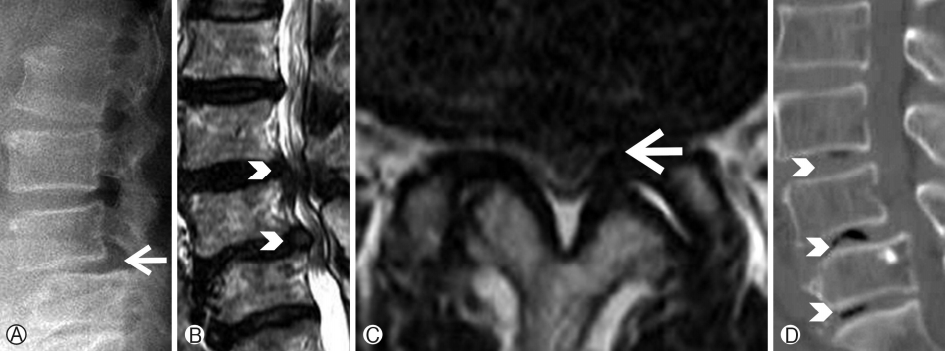
Ⓐ) flexion lumbar lateral simple tomograph shows grade I spondylolisthesis with dynamic instability on L4-5 (white arrow), Ⓑ T2 sequence sagittal magnetic resonance image (MRI) shows spinal stenosis on L3-4-5 (white arrowheads), Ⓒ T2 axial MRI shows concomitant left central disc extrusion with downward migration on L3-4 (white arrow), Ⓓ Sagittal computed tomography shows multiple vacuum intervertebral discs on L3-4-5-S1 (white arrowheads).
2. Operation
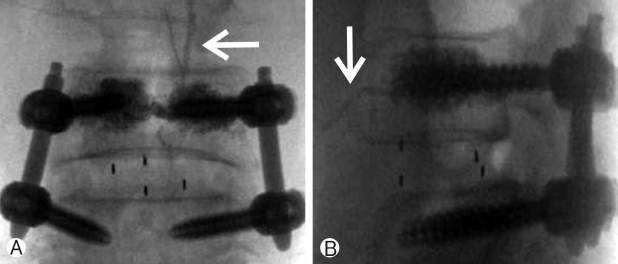
After inserting an interbody cage at L4-5 with an anterior approach, the patient was placed in the prone position for posterior decompression on L3-4 and percutaneous posterior fixation on L4-5. Approximately 6 mm of L4 vertebral body reduction was needed for an optimal lumbar lordosis and to decompress L4 exiting roots bilaterally. To overcome her weak bony structure due to osteoporosis and gain additional strength, bone cement augmentation was performed on each pedicle of the L4 vertebral body before the screw insertion. During the cement augmentation, cement leakage was visible through the right segmental vertebral vein and cement insertion was halted immediately (Fig. 2). Consequently 2 cc of cement augmentation was performed on the left side and 1.5 cc of cement augmentation was performed on the right side. There was no obvious unstable hemodynamic change during the entire operation.
3. Postoperative Course
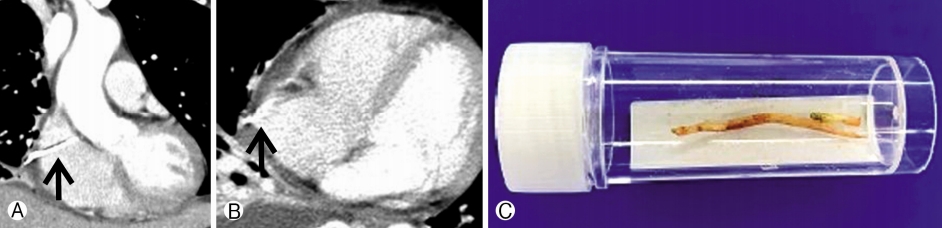
On postoperative day (POD) 1, her left sciatica improved to VAS 3 and she could walk without any assistance. On POD 2, she reported chest wall pain on the right side. A chest X-ray showed an asymmetric pleural effusion on the right lung field and a string shaped cement embolus was visible on the right cardiac silhouette (Fig. 3Ⓐ). Since her vital signs were stable, we presumed her chest pain originated from the pleural effusion due to fluid overloading and therefore treated her conservatively for 2 days with diuretics and oral analgesics. On POD 4, her symptoms and pleural effusion improved (Fig. 3Ⓑ). On POD 5, her right chest wall pain was aggravated and the pleural effusion had relapsed on the chest X-ray (Fig. 3Ⓒ). Although there was no hemodynamic instability, she was transferred to a tertiary hospital for further evaluation. At the emergency department, she underwent chest CT, which revealed perforation of the right atrium by a string shaped cement embolus (Fig. 4). She was transferred to the Department of Thoracic and Cardiovascular Surgery and underwent a foreign body removal operation through a 5th intercostal thoracotomy. Under the operation field, a string shaped cement embolus with a length of 4.5 cm was found to have perforated the pericardium and right atrium and was gently pulled out after placing purse string sutures around it (Fig. 4Ⓒ). Fortunately, there was no hemodynamic instability during and after the operation. She was discharged from the tertiary hospital after a week of postoperative care. Two months after the lumbar operation, her radiculopathy and back pain had improved and there was no more chest wall pain.
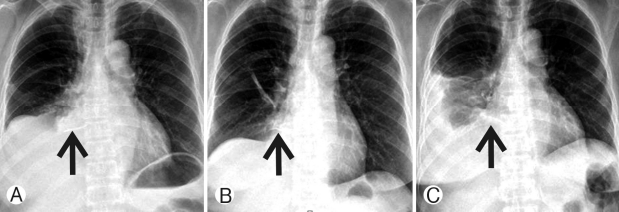
Ⓐ Posteroanterior chest X-ray on postoperative day (POD) 2 shows asymmetric pleural effusion on the right lung field and string shaped cement embolus on the right cardiac silhouette (Black arrow), Ⓑ After the conservative care pleural effusion subsided on POD4, the cement embolus became more vivid (black arrow), Ⓒ pleural effusion was aggravated again on POD5.
DISCUSSION
To study the incidence of cardiac perforation, we performed a PubMed search with the keywords “cement”, “cardiac perforation”, and “polymethylmethacrylate (PMMA)”. Twenty two case reports of cardiac perforation by a string shaped cement embolus were found and these are listed in Table 1 [1,4-7,10-12,15,16,18-27,29,30]. Fifteen (68.2%) of the reported patients underwent vertebroplasty and the rest underwent kyphoplasty (6, 27.3%). CAPSI was reported for only one patient (4.5%) by Andra et al. [1]. Therefore, this is the second report of cardiac perforation after CAPSI. The operated levels for the 22 patients reported in the literature varied from T8 to S1. Seven (31.8%) of the operations were at the thoracic level and the others (15, 68.2%) were limited to the lumbar levels. This shows that an embolus from the lumbar or sacral vertebral levels can also cause cardiac perforation. Most of the patients suffered from chest pain or dyspnea without hemodynamic instability (19, 86.4%). Interestingly only seven (31.8%) patients had these symptoms within a week. The others experienced an insidious onset with a wide range of symptom intervals from 10 days to five years. The insidious onset could be explained by the hypothesis that cement emboli can remained as intra-cardiac emboli until it penetrates or irritates the cardiac wall. Hatzantonis et al. reported a patient with left-sided chest pain, tachycardia and tachypnea 4 weeks after the vertebroplasty [12]. Echocardiogram revealed intra-cardiac cement emboli without perforation of the right ventricle wall, so they treated patient with enoxaparin at therapeutic dose of 1.5 mg/kg for 3 months with close follow up exams. They suggest that for patient with other treatable reasons for symptoms, without cardiopulmonary failure could be treated conservatively.
The insidiouis onset nature of the chest pain could also be the reason why cardiac perforation by cement emboli is underestimated by spine surgeons. Patients are asymptomatic during the postoperative care period, which is usually one to three days. Only two cases (9%) were reported in a spine-related journal (Farahvar et al., and Tran et al.) [10,29]. The onset of the patient’s chest symptoms was one day after surgery in both reports. The other 20 reports (91%) were in cardiovascular, chest surgery, or radiology-related journals. Fortunately, two (9%) of the patients could be treated with minimally invasive endovascular retrieval; however, most patients were treated with open surgery (19, 86.4%). One patient could not receive any treatment due to sudden death and cardiac perforation by a cement embolus was found during an autopsy [6].
Cardiac perforation by a string shaped cement embolus occurred in all patients (22, 100%). Cement leakage can occur in several types of peri- or intra- vertebral body veins. These include the basivertebral, hemiazygos, azygos, and segmental veins [31]. The segmental veins are known to connect directly to major vessels like the azygos vein or inferior vena cava (IVC), which connect to the right heart and pulmonary artery [31]. Therefore, cement leakage to the peri-vertebral segmental veins should be considered the main route for intracardiac cement emboli. We believe the string shape likely forms in the perivertebral segmental veins, which generally have a linear shape. In addition, the right segmental veins are closer to the IVC and shorter than veins on the other side. In our case, there was a linear shaped leakage during the procedure through the L4 right segmental vein (Fig. 2). When leakage in this form is detected, immediate termination of the procedure is essential and thorough reading of the postoperative chest X-ray is required. Even when the leaked cement settles in the segmental vein, it can migrate later to the IVC, heart, or pulmonary artery. To prevent further migration, these fragments can be retrieved preemptively using endovascular snares [32]. A surgical approach should be considered when the cement pieces are too large to be extracted through the femoral catheter window.
There are several suggestions for the prevention of cement emboli. The first is to prevent leakage by thorough fluoroscopic inspection during the procedure. To do so, more vivid visualization of the cement leakage is required by increasing the proportion of barium in PMMA, which can help with early detection. Once cement extravasation to the segmental vein is detected, the procedure should be halted because the vein is directly connected to the azygos vein and IVC. Leakage through the segmental veins is detected in 14% of lateral radiographs and 52% of anterior-posterior (AP) views [31]. Since the lateral view is mainly utilized during CAPSI, frequent verification of leakage with the AP view is recommended. Concurrent venography can also be considered before cement injection for selective use embolization agents. However, the use of contrast media for venography may interfere with early detection of cement leakage, and is therefore controversial [12]. Viscosity is not a measurable value; therefore, despite the ambiguity, toothpaste-like viscosity is generally recommended. Low viscosity can cause early leakage before the hardening of the cement by polymerization of the PMMA.
Sophisticate control of the injection pressure is the key to fill the vertebra sufficiently and to minimize the risk of cement leakage. Broud et al. subdivide pressures should be considered for proper cement injection as follows: extra-vertebral pressure, trabecular cavity pressure, and vertebral cortex pressure [2]. Since interbody cage of anterior approaches is larger and it covers the wider surface of vertebral end-plate than that of posterior approaches, extra-vertebral pressure and vertebral cortex pressure can be assumed to be higher than that of posterior approaches. Therefore lessor injection pressure with careful inspection during the cement injection should be applied for those cases to minimize the risk of the venous leakage.
Cement leakage can also be prevented by using preventive material or controlling systemic pressure. Gelfoam preinjection embolization was reported to be an effective technique for preventing cement leakage [3]. Bhatia et al. performed gelfoam embolization prior to cement insertion routinely for osteoporotic patients, and reported a 2% epidural leakage rate [3]. Preoperative placement of an IVC filter could also be considered for severely osteoporotic patients as a preventive step [28]. El saman et al. insisted that a positive end expiratory pressure of 15 cmH2O could reduce local cement leakage [8]. The underlying mechanism is the temporary induction of high pressure in the IVC and segmental vein, which can suppress pressure in the tapped cavity before cement augmentation [8].
CONCLUSION
CAPSI is a generally safe and feasible procedure for osteoporotic patients. However, when a string shaped cement leakage is detected in the peri-vertebral segmental vein and postoperative chest pain develops, cardiac perforation should be considered as a possible cause for the symptom. Prompt evaluation, a high level of suspicion, and immediate surgical or procedural treatment are crucial to treat this disease entity and avoid fatal outcomes.