AbstractObjectiveAnterior cervical discectomy and fusion (ACDF) surgery is a standard treatment for cervical spondylotic myelopathy or radiculopathy. Although the outcomes of ACDF are quite satisfactory, recurrent radiculopathy due to restenosis or adjacent degeneration cannot be completely avoided. We applied posterior endoscopic cervical foraminotomy (PECF) as salvage surgery after ACDF in 11 patients (16 levels).
MethodsWe performed PECF in 11 patients (16 levels) in the past 5 years for recurrent radiculopathy after ACDF. The time until the development of recurrent radiculopathy ranged from 8 months to 3 years. Before surgery, all patients were treated with adequate medication and rehabilitation. The radiological tools used for the evaluation included x-ray examinations (with anteroposterior, lateral, flexion, extension, and bilateral oblique views), computed tomography, and magnetic resonance imaging of the cervical spine.
ResultsOnly one of the 11 patients did not respond immediately; however, that patient showed gradual recovery after decompression surgery in the following 6 months. Another patient showed good sensory function recovery, but transient motor palsy for 2 weeks. Otherwise, all the other patients showed motor or sensory function recovery, without symptom deterioration. None of these patients presented instability or mechanical pain after surgery or required repeat anterior surgery during follow-up (8 to 20 months; mean, 12 months).
INTRODUCTIONAnterior cervical discectomy and fusion (ACDF) surgery has been the standard treatment option for cervical spondylotic myelopathy and radiculopathy since 1958 [1]. Although outcomes following ACDF are generally satisfactory, recurrent radiculopathy may occur due to factors such as pseudarthrosis, implant subsidence, hardware migration, or adjacent-segment disease [1,2]. Anterior revision surgery carries a high risk of complications. For patients with adjacent-segment disease, the anterior approach carries the risk of revision surgery and requires an extension of fusion levels [3]. Posterior endoscopic cervical foraminotomy (PECF) is an alternative strategy for cervical radiculopathy that was first used in 2000 [4,5]. PECF provides similar outcomes as ACDF. Furthermore, a posterior approach allows the surgeon to avoid scarring, tricky anatomical regions caused by prior surgeries, and the need to extend fusion levels for patients with adjacent-segment disease. In this clinical study, we applied PECF as salvage surgery for 11 patients with recurrent radiculopathy after ACDF (16 levels). This case series reviewed the efficacy and advantages of PECF as a treatment option for recurrent radiculopathy following ACDF.
MATERIALS AND METHODSThis is retrospective clinical study. Recurrent radiculopathy is defined as the alleviation of symptoms following the last ACDF procedure but with subsequent recurrence or new development of radiculopathy after a period of at least 6 months without symptoms. We included both recurring similar symptoms (i.e., same location and level) and newly developed distinct symptoms (i.e., different location and level). Over the past 5 years, we performed PECF on 11 patients (16 levels) for recurrent radiculopathy after anterior discectomy and fusion or disc replacement surgery. Anterior surgery was performed by different doctors but PECF was performed by the same doctor at a single hospital. Patient demographics are listed in Table 1. Most patients had unilateral radiculopathy of a single level.
1. Decision-Making ProcessFor patients who have been experiencing intolerable radiculopathy that has not responded to conservative treatments, such as medication and physical therapy for at least 3 months, we arranged imaging studies, including x-ray (with anteroposterior, lateral, flexion, extension, and bilateral oblique views), cervical spine computed tomography, and magnetic resonance imaging studies. Patients with a contributory lesion identified in their imaging were recommended to undergo decompression surgery. We offered both anterior fusion surgery and PECF for the selected patients. All patients chose PECF. We excluded patients who had radiological central stenosis or symptomatic myelopathy and those without contributory lesions identified in their imaging. The decision-making process is shown in Figure 1.
2. Operation Procedure—PECFPatients were placed in the prone position under general anesthesia. After disinfection and draping, the point of entry (ipsilateral to the operative target) was infiltrated with 2% lidocaine. A 1-cm incision was made after confirmation of the level by using C-arm fluorescence. A working cannula was introduced and reconfirmed by using fluoroscopy. After the working cannula was set in the desired position, we removed the remaining muscle and soft tissue for exposure of the medial part of the facet joint (V-point). An endoscopic 2-mm Kerrison punch and a high-speed diamond burr were used to perform partial laminectomy and facetectomy to decompress the responsible root. We defined adequate decompression as pedicle-to-pedicle decompression. The key concept of decompression is exposure of the shoulder and axilla aspect of the responsible root. We took great care to ensure that the facetectomy was performed on less than 50% of the facet joint width to preserve stability. We opted not to perform discectomy in all cases because the neuroforamen stenosis originated from the bony structure. Instead, we performed unroofing decompression surgery for all nerve roots.
RESULTSWe performed PECF on 11 patients (16 levels) between 2017 and August 2022 for recurrent radiculopathy after ACDF or total disc replacement (Table 1). The follow-up period ranged from 8 to 24 months. The time at which radiculopathy recurred ranged from 8 months to 3 years.
Same level restenosis was present in 7 patients, affecting 12 neuroforamens (2 cases involved bilateral recurrent 1-level radiculopathy). Adjacent level radiculopathy was present in 4 patients, affecting 4 neuroforamens.
The mean operation time was 123±35 minutes per site. The mean hospital stay was 3.1 days. All patients were given a soft neck collar to wear after the operation for a period of 1 month.
Among the 11 patients, there were two uneven clinical course. One patient did not respond immediately after PECF, but exhibited gradual and subtle recovery over the course of the following 6 months ( case 5, who had previously undergone anterior cervical corpectomy and fusion). Another patient showed good sensory function recovery but transient motor palsy for 2 weeks after PECF (case 10). All of the other patients exhibited varying degrees of recovery in their motor or sensory function with no signs of symptom deterioration. In terms of the modified MacNab criteria, the satisfactory rates were 72.7% (8 of 11 patients) immediately after PECF and 90.9% (10 of 11 patients) 1 month after PECF. None of the patients had instability or mechanical pain after PECF. None of the patients required further anterior revision surgery. Details on visual analogue score change and Neck Disability Index score are summarized in Table 2.
1. Case Presentation (Case 11)A 68-year-old man received ACDF surgery for C6–7 in 2020 and presented at our clinic with recurrent right interscapular region pain and progressive loss of dexterity in his right hand 9 months after ACDF. Imaging studies revealed C6–7 cage subsidence and narrowing on the right C6–7 and C7–T1 neuroforamen (Figure 2A-E). MRI also revealed right C8 nerve root compression. The patient’s symptoms did not respond well to conservative treatment; therefore, we performed right PECF at the C6–7 and C7–T1 levels to decompress the right C8 nerve root.
Due to cage subsidence, the disc space that usually locates at the axilla aspect of right C7 nerve root, was invisible. The right C7 root abutted the right C7 pedicle due to cage subsidence. To thoroughly decompress the nerve root, we performed both facetectomy and partial pediculectomy of C7 (Figure 3A-D). After the operation, the patient demonstrated improved fine motor skills in his right hand and reported relief from interscapular pain. A video of the procedure is available in the supplementary materials.
DISCUSSIONIn this observational study, we retrospectively collected data on individuals who initially recovered from anterior cervical surgery but later developed new radiculopathy. We performed uniportal PECF for the narrowed neuroforamens responsible for symptom.
Posterior cervical foraminotomy is an effective treatment for cervical radiculopathy [6]. Its efficacy is similar to that of ACDF and it avoids the complications of ACDF, which include postoperative dysphagia, pseudoarthrosis, loss of segmental motion, and adjacent-segment degeneration [7,8]. However, posterior cervical foraminotomy carries a risk of postoperative neck pain and muscle spasm due to the stripping and retracting of paraspinal muscles. PECF is an improvement on the conventional posterior cervical foraminotomy technique that has resulted in reduced muscle atrophy and a decreased incidence of postoperative neck pain and dysfunction [5,9]. Evidence supporting PECF as an alternative to ACDF in cervical radiculopathy is increasing [6]. PECF offers similar outcomes to ACDF in selected cases with fewer complications and shorter hospital stays [4,10]. The direct cost of PECF is 89% on average, less than that of ACDF [11]. In select situations, physicians should consider minimally invasive posterior cervical foraminotomy or PECF for cervical radiculopathy.
Posterior cervical foraminotomy is effective at decompressing the neuroforamen [10,12]. However, patients with ventral osteophyte and neuroforamen osseous stenosis have worse outcomes after PECF than after ACDF [13]. For lateral disc and foraminal stenosis, we believe that PECF provides more thorough and direct decompression compared with anterior decompression [14]. With regard to anatomy, during anterior decompression surgery at the C5–6 and C6–7 levels, which are the levels most commonly affected by cervical spondylosis, the disc and uncovertebral joint are located at the axilla region of the exiting nerve root. The root exits the cord cranially to the disc level. When we decompressed the root anteriorly via the disc space, decompressing the shoulder aspect of the nerve root was challenging. The sensory component of the nerve is located in the dorsal–cranial direction of the root. Achieving complete decompression in the lower cervical levels is challenging when discectomy via the anterior approach was used. With the advancement of endoscopic instruments and techniques, such as high-speed burrs and durable grasping forceps, access to ventral osteophytes of the neuroforamen can be achieved by partial pediculectomy and partial vertebrotomy. Despite being technically demanding, this procedure creates 180°–270° of decompression to the index root without affecting cervical stability [14,15].
In a retrospective clinical study that explored the efficacy of posterior decompression surgery in patients who had undergone prior anterior surgery, the author discovered that recurrent radiculopathy after prior cervical surgery usually occurred at the original level (65%) within 2 years (68%) [7,13]. The author also observed that patients with a history of anterior surgery had poorer clinical outcomes than those in a surgery-naive group (75% vs. 95.2%, respectively). The author attributed the observed outcome to a higher percentage of kyphotic change and osseous stenosis of the neuroforamen in the cases that had undergone surgery. In our series, each of the cases had osseous neuroforamen stenosis due to inadequate decompression, restenosis, or cage subsidence. In the present study, In the present study, we performed PECF from pedicle-to-pedicle decompression in every levels and added partial pediculectomy partial vertebrotomy (PPPV) for ventral osteophyte in only one case. All patients exhibited varying degrees of recovery in their sensory or motor function. Our results indicate that patients can benefit from PECF only.
In case 11, restenosis occurred due to cage subsidence; therefore, we performed laminotomy and facetectomy and partial pediculectomy of C7. The decreased disc height caused the C7 root to abut against the C7 pedicle. We used an endoscopic chisel and high-speed burr to complete the task without damaging the nerve root.
Another advantage of PECF as salvage surgery for ACDF is that it eliminates the need to address previous implants or extend fusion levels. For cases involving restenosis at the index level, attempting to remove implants can result in further damage to the endplate and vertebral body, making reimplantation and fusion more challenging. Alternatively, extending fusion to adjacent levels can limit neck mobility and increase costs.
ACDF is the preferred treatment for cervical spondylotic myelopathy and radiculopathy, despite some potential complications, such as implant-related events, approach-related complications, and adjacent-segment degeneration [7]. Cases where anterior revision is necessary have a high risk of adverse outcomes, including thromboembolic events, surgical site infections, repeat operation, blood transfusion, and readmission within 30 days [3]. These findings have important implications for patient counseling and risk assessment.
The present study has several limitations. First, the sample size is small and surgeries were performed by a single surgeon. This is a retrospective observational study, and the causes of recurrent spondylosis are diverse due to different habit and surgical technique of surgeons who had operated on the patient. All patients had experienced anterior cervical fusion surgery and subsequently chose the posterior approach. All patients agreed that the posterior approach is less burdensome than the anterior approach. We did not provide open posterior decompression and fixation as choice for the patients since we did not encounter obvious instability and wanted to provide minimal invasive method, in comparison with their previous surgery. We also found that the degree of neuroforamen stenosis did not always correspond with the severity of symptoms. Not all patients with neuroforamen stenosis and radiculopathy respond well to medication. We believe that subjective clinical improvement may be due to more than just mechanical decompression; it may also result from clearance of inflammatory material and adhesion bands. Further research is necessary to validate the correlation between neuroforamen size and clinical presentation.
Figure 1.Decision-making process. s/p, status post; ACDF, anterior cervical discectomy and fusion; ADR, artificial disc replacement; ACCF, anterior cervical corpectomy and fusion; Tx, treatment; PT, physical therpay; NSAID, nonsteroid anti-inflammatory drug; CT, computed tomography; MRI, magnetic resonance
imaging; NCV, nerve conductive velocity; EMG, electromyeography; RASP, radiological adjacent segmental pathology; PECF, posterior endoscopic cervical foraminotomy. 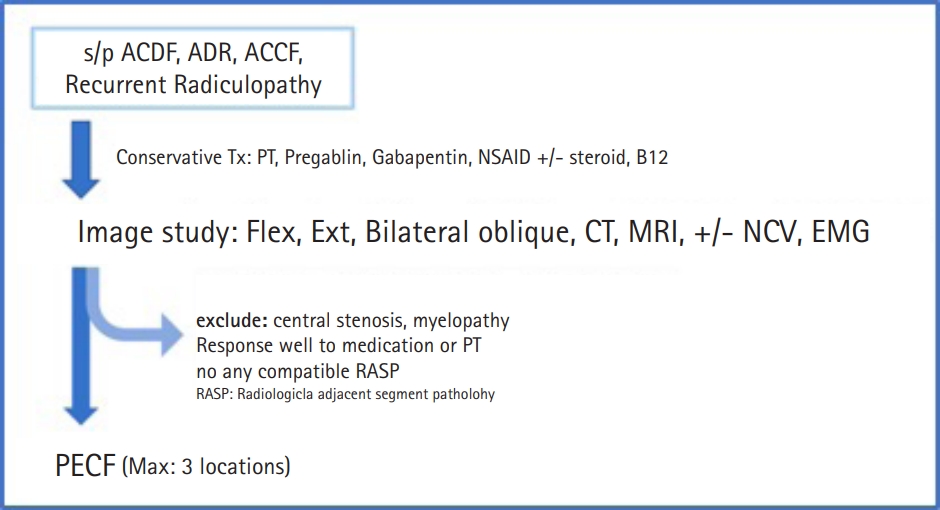
Figure 2.(A, B) Cervical spine x-ray after the first ACDF surgery at the C6–7 level. (C–E) Cervical spine x-ray 9 months after first surgery. Both anteroposterior and lateral views showed cage subsidence and subsequent neuroforamen narrowing. (E) Magnetic resonance imaging of the right-side C6–7 neuroforamen. The white arrow indicates abutment of the C7 root against the C7 pedicle. ACDF, anterior cervical discectomy and fusion. 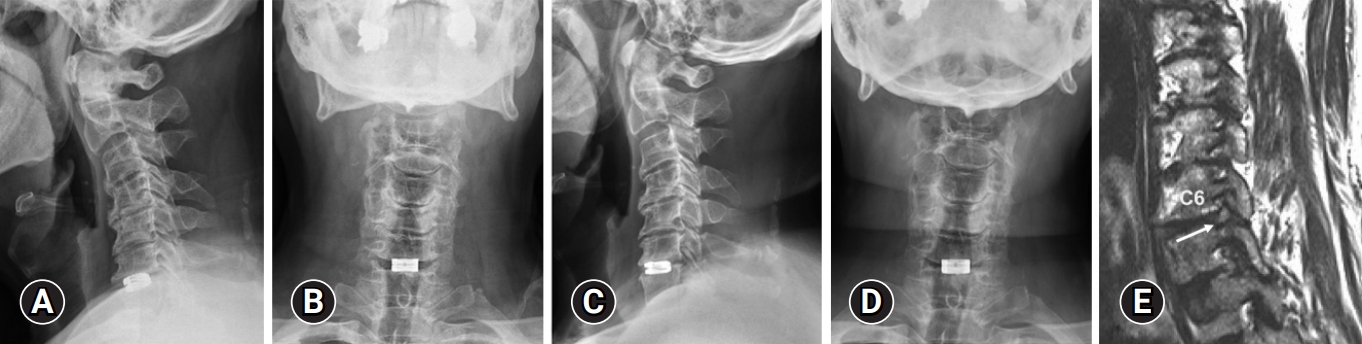
Figure 3.Sketches illustrate how cage subsidence leads to nerve abutment at the inferior pedicle (A: normal situation; B: cage subsidence). To decompress the nerve root, we performed not only partial facetectomy but also partial pediculectomy (gray area) to decompress C7 root. (C) Before partial pediculectomy. The asterisk (*) indicates the right C7 pedicle. (D) After partial pediculectomy. The dotted circle indicates the extent of the right C7 pediculectomy. 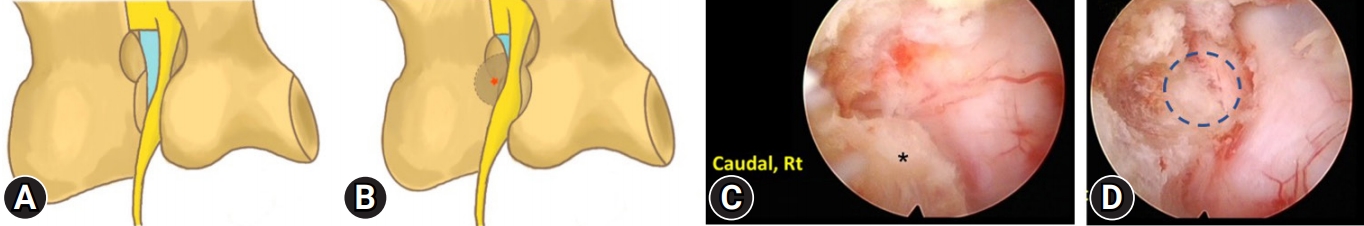
Table 1.Demographics of collected patients REFERENCES1. Yuen J, Whitfield P. Anterior cervical discectomy and fusion (ACDF) for degenerative cervical diseases - Six decades on. ACNR 2017;16. https://doi.org/10.47795/IWDK8512.
2. Cheung JP, Luk KD. Complications of anterior and posterior cervical spine surgery. Asian Spine J 2016;10:385–400.
3. Basques BA, Ondeck NT, Geiger EJ, Samuel AM, Lukasiewicz AM, Webb ML, et al. Differences in short-term outcomes between primary and revision anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2017;42:253–60.
4. Ahn Y, Keum HJ, Shin SH. Percutaneous endoscopic cervical discectomy versus anterior cervical discectomy and fusion: a comparative cohort study with a five-year follow-up. J Clin Med 2020;9:371.
5. Ji-Jun H, Hui-Hui S, Zeng-Wu S, Liang Z, Qing L, Heng-Zhu Z. Posterior full-endoscopic cervical discectomy in cervical radiculopathy: a prospective cohort study. Clin Neurol Neurosurg 2020;195:105948.
6. Sahai N, Changoor S, Dunn CJ, Sinha K, Hwang KS, Faloon M, et al. Minimally invasive posterior cervical foraminotomy as an alternative to anterior cervical discectomy and fusion for unilateral cervical radiculopathy: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2019;44:1731–9.
7. Yee TJ, Swong K, Park P. Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg 2020;6:302–22.
8. Kim SJ, Seo JS, Lee SH, Bae J. Comparison of anterior cervical foraminotomy and posterior cervical foraminotomy for treating single level unilateral cervical radiculopathy. Spine (Phila Pa 1976) 2019;44:1339–47.
9. Platt A, Gerard CS, O'Toole JE. Comparison of outcomes following minimally invasive and open posterior cervical foraminotomy: description of minimally invasive technique and review of literature. J Spine Surg 2020;6:243–51.
10. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:940–8.
11. Mansfield HE, Canar WJ, Gerard CS, O'Toole JE. Single-level anterior cervical discectomy and fusion versus minimally invasive posterior cervical foraminotomy for patients with cervical radiculopathy: a cost analysis. Neurosurg Focus 2014;37:E9.
12. Nguyen J, Chu B, Kuo CC, Leasure JM, Ames C, Kondrashov D. Changes in foraminal area with anterior decompression versus keyhole foraminotomy in the cervical spine: a biomechanical investigation. J Neurosurg Spine 2017;27:620–6.
13. Burkhardt BW, Müller S, Oertel JM. Influence of prior cervical surgery on surgical outcome of endoscopic posterior cervical foraminotomy for osseous foraminal stenosis. World Neurosurg 2016;95:14–21.
|
|
|||||||||||||||||||||||||||||||||||||||||