AbstractFully endoscopic lumbar surgery has emerged as an alternative technique to classic open microscopic laminectomy or discectomy. It is gaining popularity due to its advantages in terms of minimal invasiveness, while achieving equivalent clinical outcomes. Remarkable technical developments in surgical techniques and instruments have expanded the indications of this surgical method. However, as the utilization of endoscopic surgery increases, related complications inevitably arise and become major clinical issues. Frequent complications include failure to achieve adequate decompression, early recurrence, and the possibility of wrong-level surgery. Intraoperative and perioperative complications can include postoperative sensory changes related to neural injury, dural tears, hematoma, infection, and rarely, water pressure-related problems. This review article presents an overview of the possible intraoperative and perioperative complications associated with uniportal full-endoscopic surgery. We also discuss the pitfalls that can lead to unexpected devastating results. Additionally, we briefly review potential preventive efforts that can help reduce the risks. The objective of this presentation is to reinforce the basic principles and introduce key technical tips for full-endoscopic spine surgery, ultimately leading to clinical success and the prevention of complications.
INTRODUCTIONSpine surgery has experienced significant technological advances in recent decades, one of the most notable being the introduction of endoscopic techniques. Full-endoscopic lumbar spine surgery has demonstrated potential for better clinical outcomes, faster recovery, and less postoperative pain compared to traditional open surgery [1,2]. However, similar to other surgical procedures, it does not come without its complications [3,4].
Endoscopic lumbar spine surgery involves the use of an endoscope to perform surgery on the lumbar region of the spine, typically to relieve pressure on nerve roots or the spinal cord caused by herniated discs, bone spurs, or spinal stenosis [5]. Due to the minimally invasive nature of the procedure, it is often associated with less blood loss, shorter hospital stays, and reduced soft tissue trauma compared to open surgery. Nevertheless, understanding potential complications and their preventive strategies are crucial for enhancing patient safety and outcomes.
This paper seeks to provide an overview of potential complications associated with full-endoscopic lumbar spine surgery and highlight preventive measures that can be implemented to mitigate them. This knowledge is essential for surgical teams to anticipate, recognize, and manage complications should they occur. Through this paper, we aim to contribute to the ongoing dialogue and research surrounding full-endoscopic lumbar spine surgery, with a focus on enhancing the patient-centered care approach and promoting best surgical practices. The narrative review on the complications of endoscopic spine surgery was conducted using a comprehensive methodology to ensure a comprehensive analysis of the available literature. In addition to review of the existing literature, the authors’ experiences were added throughout the review, and these findings were synthesized and presented in a narrative format, providing a comprehensive overview of the various complications, their incidence rates, potential risk factors, and strategies for prevention and management. The methodology employed in this narrative review ensured a systematic approach to identify and synthesize the existing evidence on complications associated with endoscopic spine surgery, thereby contributing to a better understanding of this important aspect of the procedure.
INCOMPLETE SURGERY AND RECURRENCEIncomplete surgery can be defined as a possible complication that results in remnant spinal pathology related symptoms on the operated side, even after decompression of the spinal neural structures or removal of intervertebral disc materials (Figure 1). The time window defining incomplete surgery differs by each study, however generally incomplete surgery refers to remnant symptoms requiring additional treatment immediately after the surgery, while remote reappearance of symptoms within a certain period usually are categorized as recurrence. Recurrences usually have a transient period of resolution of the preoperative symptoms following a significant reappearance of the similar or sometimes even worse symptoms (Figure 2). Both incomplete surgery and recurrence after an endoscopic spine surgery are relatively common complications. Choi et al. [6] reported that incomplete surgery occurred in 2.8% of their 10,228 endoscopic discectomy cohorts at a single center. Although all incomplete surgeries or recurrences do not necessarily lead to reoperations, various studies have reported 2% to 15% rate of reoperations related to incomplete surgery or recurrence [7-9].
Occurrence of incomplete surgeries are usually related to inappropriate or suboptimal surgical approach of the endoscope, misunderstanding of the characteristics of the disc herniation or neural compression and sometime related to challenging cases [6,10,11]. Therefore, thorough preoperative optimization of the best surgical corridor and deep understanding of the individual characteristics of each spinal pathology can lead to lower risk of incomplete surgeries. Another possible preventive measure is utilization of modified techniques of endoscopic surgery. The wide acceptance of endoscopic spine surgery naturally leads to modifications in techniques that optimize procedures for each unique clinical situation, including modifications that offer advantages for lesser risk for incomplete surgeries [12]. There are several additional intraoperative measures that help surgeons determine whether adequate decompression has been achieved or not. Inspect the full free mobilization of the nerve root with careful examination on both the beginning and endpoint of neural structures, repeatedly open and close the water outflow to observe the spontaneous pulsation of the dura which indicates good decompression [13].
Although a widely agreed consensus on the specific time period to define recurrence after endoscopic spine surgery is lacking, it is well-established that the rate of recurrence following an initial procedure is estimated to be approximately 0.5% to 1.5% [6,14,15]. An interesting fact about recurrence after endoscopic spine surgery is that the overall recurrence rate is not that different from conventional microscopic discectomies, however they tend to recur more earlier [15]. Although we have not yet found an ideal solution for decreasing the risk of recurrence, optimized surgical strategies such as determining the appropriate amount of disc removal or performing radiofrequency ablation annuloplasty after removal may provide assistance. Absolutely, considering the natural course of degeneration of the intervertebral disc after an endoscopic surgery is also important when planning any intervention or treatment. The postoperative change of the intervertebral disc is inevitable and can have a significant impact on the clinical outcome and long-term consequences of any intervention [16].
POSTOPERATIVE HEMATOMASJust like any other spinal surgical procedures, unexpected bleeding and resultant hematomas can occur after endoscopic spine surgeries. The majority maybe subclinical, asymptomatic that they can be even unnoticed, but in rare incidences they result in devastating clinical conditions such as neurologic deterioration. Hematomas can occur both at the epidural space or the retroperitoneal space depending on the surgical approach or detailed surgical procedures [17]. Postoperative epidural hematomas that requires surgical evacuation after an endoscopic surgery is reported to be 0.1% to 1% [18-20]. Most of these uncontrolled clinically significant hematomas are due to unexpected injures to lumbar radicular arteries of any of its’ distal branches [17]. Trying to stay posterior to the posterior vertebral body line helps to avoid intervening with major vascular structures and exercising extra caution during the surgery to prevent injury to vessels, especially in the foraminal area, can help reduce the risk of bleeding.
Fortunately, thanks to the nature of full-endoscopic surgeries, which require minimal or no working space during the procedure, there is limited room for bleeding or hematoma formation. As a result, most hematomas that do occur are subclinical or self-limiting in nature for most cases. Nonetheless, we still need to do maximum effort to reduce the risk of any possible hematomas, epidural or retroperitoneal. Applying modified techniques, such as transsuperior articular process approaches for transforaminal surgeries, can be beneficial. This approach involves landing in an anatomical area that has minimal arterial distal branches, specifically the ventral part of the superior articular process. By using this technique, the risk of encountering arterial bleeding can be further reduced.
Regardless of the endoscopic approach – transforaminal or interlaminar, meticulous hemostasis using various measures including radiofrequency ablation, mixture of epinephrine to the irrigation saline, use of hydrostatic pressure for bleeding control and utilization of various commercialized hemostatic agents can also help reducing the risk of bleeding. Thermal nerve injury caused by radiofrequency is another potential secondary injury that can occur after using it for hemostasis during bleeding control. While radiofrequency is an effective measure for preventing bleeding complications, it can also lead to iatrogenic thermal nerve injury if not used with caution. Therefore, maintaining high vigilance during surgery and exercising careful application of radiofrequency at all times are essential to prevent any potential injuries [21].
NEURAL INJURIES AND IATROGENIC DUROTOMIESAs the primary objective of most endoscopic surgeries is to decompress the neural elements within the spinal canal, unexpected neural injuries can occur during the manipulation or decompression of neural structures during surgery, and in many cases, they can happen even unnoticed. Although nerve root injuries are rare for experienced endoscopic spine surgeons, they can occur during the early stages of the learning curve for inexperienced surgeons. The most frequent neural injury during transforaminal endoscopic spine surgeries is the irritation of the exiting nerve root, dorsal root ganglia, or possibly the furcal nerve in the foraminal area and the reported rates are ranging from 0.1% to 4% [22]. While iatrogenic neural injuries are uncommon when there is full visualization during surgery, the majority of exiting nerve injuries are known to be related to the transforaminal surgical approach in most cases [13,23,24]. Although even rarer than exiting root injuries during transforaminal approaches, excessive nerve root retraction during interlaminar surgeries can also result in catastrophic traversing root injuries.
Indeed, careful preoperative planning plays a vital role in minimizing the risk of complications and optimizing surgical outcomes. Thoroughly analyzing the imaging studies, such as magnetic resonance imaging or computed tomography scans, allows surgeons to gain valuable insights into the specific anatomical characteristics of the exiting root in individual cases (Figure 3). The utilization of modified techniques in endoscopic surgery can be a potential preventive measure to reduce the occurrence of exiting root injuries in transforaminal approaches. The transsuperior articular process approach, which focuses on targeting the point farthest from the exiting root within Kambin triangle, can be beneficial in reducing the risk of potential exiting root injuries [25]. This technique aims to minimize the chance of inadvertently damaging the exiting nerve root during endoscopic procedures by precisely navigating and accessing the desired area. By carefully selecting the entry point and trajectory, surgeons can decrease the risk of injury to the exiting root and enhance the safety of the procedure. Unfortunately, there is still no foolproof or perfect way to prevent certain events. In various situations, despite our best efforts, certain injuries may still occur. While we strive to minimize risks and take preventive measures, it is important to acknowledge that we cannot completely eliminate all potential issues or guarantee absolute prevention. Instead, the focus is on implementing best practices, protocols, and guidelines to reduce the likelihood of such events and to manage them effectively when they do occur.
Iatrogenic dural injury is one of a common complication during endoscopic spine surgery procedures (Figure 4). Although it is not frequently seen, if a dural tear does occur, it can lead to cerebrospinal fluid leak leakage, which in turn can cause orthostatic headaches, and in more severe cases, it can result in the formation of pseudomeningoceles that may require additional surgical repairs [26-28]. It inevitably leads to prolonged hospital stay, poor immediate postoperative outcomes and poor patient satisfaction once occurred. While the reported incidence of iatrogenic durotomy during conventional open spinal surgeries varies between studies, ranging from 3.1% to 14% [26-28], there is little reported regarding the rate of durotomy during endoscopic spine surgeries. Although the number of reports on this topic is limited, the currently available evidence suggests that the durotomy rate during endoscopic surgery falls within the range of 0.5% to 7.5% [29-32]. These findings indicate that endoscopic surgery itself does not pose a higher risk for dural injuries compared to open surgery. In fact, the reported rates of durotomy during endoscopic surgery are even lower than those reported for open surgery. Absolutely, despite the lower reported rates of durotomy during endoscopic procedures compared to open surgery, it is crucial to exercise great caution during any endoscopic procedure to avoid injuring the dura. To minimize the risk of dural injury, surgeons performing endoscopic procedures should employ meticulous techniques and adhere to proper surgical principles. Diligent attention and care such as keeping the ligamentum flavum as a dura protector [11], should be taken throughout the procedure to ensure the integrity of the dura is maintained.
Due to the limited access and visualization provided by endoscopic procedures, direct repair of a durotomy can be challenging. In such cases, the conversion to an open surgery may be necessary as it provides better exposure and facilitates easier repair of the durotomy. However, it's important to note that this conversion comes at the expense of losing the benefits offered by an endoscopic procedure. Therefore, several full-endoscopic dural repair techniques have been introduced including direct repair of it [33,34], using muscle patches or applying commercially available collagen patches (Figure 5) [31,35]. In most cases durotomies are well managed by these intraoperative endoscopic repairs or sealing techniques without any significant additional complications, with no worsened clinical outcomes. However, in cases where unrepairable and clinically significant injuries are identified, it is important not to hesitate in converting to open surgery to address and repair them. The priority should be the proper management of the injury, even if it means transitioning from the initial endoscopic approach to an open surgical procedure.
MISCELLANEOUS AND OTHER COMPLICATIONSSurgical site infection after a spinal surgery is a common complication that occurs in 0.7% to 10% of open surgical cases which is directly linked to surgery related outcome and quality of life [36,37]. It is a great socioeconomic burden at the same time. Thanks to the nature of this specific technique that does the entire procedure withing continuous aseptic saline irrigation, the reported post operative infection rate is extremely low [6,38]. However, when the cylindrical structure of the endoscope channels is not adequately cleaned and sterilized, there is a risk of unexpected infections occurring at any time. Therefore, it is crucial to exercise caution and ensure proper cleaning and sterilization procedures are followed.
Water pressure-related complications are additional unique problems that should be taken into consideration. During full-endoscopic procedures, there is continuous infusion and irrigation of saline over the epidural space throughout the surgery. This can be a point of concern as it has the potential to increase epidural pressure at any given time, and in rare cases they can lead to increased intracranial pressure [39]. Although the reported incidence of problems related to increased intracranial pressure is less than 0.1% [6,39], it can occur due to negligence or carelessness in managing the dynamics of saline irrigation. Therefore, it is crucial for endoscopic spine surgeons to ensure proper regulation of infusion using pump irrigation systems or natural drain systems to mitigate the risk.
DISCUSSIONFull-endoscopic lumbar spine surgery, emerging as a significant milestone in the realm of spinal surgical practice, has been rapidly garnering attention and recognition due to its minimally invasive nature. A paradigm shift from traditional open surgery, this novel approach is underpinned by the core principles of minimally invasive surgery, aiming to achieve the same or better surgical outcomes while causing the least possible disruption to the patient's body. The operational benefits offered by this technique are vast and multifold, ranging from decreased operative trauma to reduced recovery times, and improved patient comfort [2,5,23]. Firstly, the minimally invasive characteristic of this procedure results in reduced tissue injury, lessening surgical trauma. By preserving the integrity of surrounding tissues, full-endoscopic lumbar spine surgery decreases postoperative inflammation and pain, facilitating a faster recovery process for patients. This is a crucial advantage over traditional open surgeries, which typically involve more extensive tissue damage and consequently, longer recuperation periods [40]. Additionally, this method also promises reduced recovery times, enhancing the overall patient experience. Faster postoperative recovery translates into shorter hospital stays, prompt return to daily activities, and reduced healthcare costs—a significant improvement not only in the quality of life for patients but also in terms of broader healthcare economics [2,41]. Enhanced patient comfort is another compelling advantage of this technique. The reduced trauma, faster recovery, and minimal scarring associated with this procedure collectively contribute to an improved patient experience, and higher satisfaction rates [2].
However, while this technique is revolutionizing the field of spine surgery with its impressive advantages, it is important to acknowledge that it is not devoid of potential complications. Just like any other surgical procedure, full-endoscopic lumbar spine surgery carries certain inherent risks and complications. From potential nerve injuries to the risk of disc herniation recurrence, these complications can have significant implications for patient outcomes [1,42]. Therefore, a comprehensive understanding of these potential complications, along with the development and application of strategic preventative approaches, is absolutely crucial in order to ensure optimal patient outcomes and fully realize the transformative potential of full-endoscopic lumbar spine surgery.
One of the potential complications associated with the transforaminal approach is the exiting nerve root injury. Key prevention strategies lie in the accurate assessment of the surgical approach and the precise docking. Safe docking can significantly minimize the risk of nerve root injury [40]. Patients with a narrow foramen present an additional challenge. Such situations may necessitate a foraminoplasty to widen the foramen, using tools like a reamer or drill [43]. Furthermore, it is of paramount importance to prevent the endoscope from exerting pressure on the exiting root by ensuring a proper endoscope trajectory during the surgery.
Durotomy, another frequently encountered intraoperative complication, often necessitates immediate recognition and prompt management to prevent adverse consequences. Preventive measures such as adopting meticulous surgical techniques and fostering enhanced knowledge of the local anatomy can be particularly beneficial [31].
Thermal nerve injury due to radiofrequency is a significant concern that requires attention. This calls for diligent operative techniques, especially when using heat-generating instruments. High vigilance during surgery and careful application of radiofrequency can potentially mitigate such injuries [21]. It is crucial to highlight that safety during endoscopic spine surgery is not solely determined by the intensity of radiofrequency power used but also by the duration of its application. While the intensity of radiofrequency power plays a significant role in achieving efficient tissue ablation and coagulation, the duration of its use must be carefully considered to prevent potential complications. Prolonged exposure to radiofrequency energy can lead to excessive tissue heating and thermal damage, which may result in adverse effects on surrounding structures and tissues. Therefore, surgeons must exercise caution and adhere to established guidelines regarding the appropriate duration of radiofrequency power application during endoscopic spine surgery. This balanced approach, considering both power intensity and time duration, is essential to ensure patient safety and optimize surgical outcomes in the context of endoscopic spine procedures [21].
Dealing with more rare but highly impactful complications, such as massive or remote epidural/subdural hematoma due to hydrostatic pressure, warrants cautious and controlled use of irrigation during surgery, as well as attentive postoperative monitoring [29,44-46]. This further accentuates the critical role of comprehensive postoperative care.
The risk of disc herniation recurrence represents a significant concern following full-endoscopic lumbar spine surgery. The implications of recurrence can range from prolonged recovery times to the requirement of additional surgical interventions, significantly affecting the quality of life and satisfaction in patients. Certain risk factors have been identified that may increase the likelihood of disc herniation recurrence, including younger age, greater disc height, and advanced stages of disc degeneration. In order to mitigate this risk, a precise surgical technique is critical. The goal should be to achieve an optimal balance during discectomy—enough disc material needs to be removed to alleviate symptoms and avoid immediate postoperative reherniation, but overzealous removal can compromise the structural integrity of the disc and potentially lead to further issues, including recurrence [42]. Moreover, the use of predictive scoring systems as part of preoperative evaluation and patient consultation can further assist in minimizing recurrence risks. Such an approach enables surgeons to better anticipate potential challenges and tailor surgical strategies accordingly, thereby enhancing overall patient outcomes following full-endoscopic lumbar spine surgery.
Moving forward, we need to recognize that the landscape of endoscopic spine surgery is continuously evolving. New technological innovations, surgical techniques, and advancements in our understanding of spinal pathology are likely to introduce new challenges and complications. Hence, commitment to ongoing research, surgical training, and collaboration among the surgical community is essential to continually improve outcomes in endoscopic lumbar spine surgery.
In conclusion, while full-endoscopic lumbar spine surgery provides significant benefits to patients, potential complications need careful attention. Through strategic preoperative planning, meticulous operative technique, and vigilant postoperative care, we can minimize the incidence and impact of these complications and realize the full potential of this transformative technique.
NOTESConflicts of Interest JWH, a member of the Editorial Board of Journal of Minimally Invasive Spine Surgery & Technique, is the corresponding author of this article. However, he played no role whatsoever in the editorial evaluation of this article or the decision to publish it. Authors have no conflict of interest to declare. Funding/Support This study was in part supported by grants from the Korea Medical Device Development Fund, Republic of Korea (KMDF_PR_20210526_0003) and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HR22C1302) to JWH. It was also supported in part by Korea University research grants (K2313771, K2311211 and K2225601) to WKK. Figure 1.(A) Representative preoperative and postoperative magnetic resonance imaging (MRI) of remnant L3/4 down-migrating disc material indicating incomplete surgery. (B) Another representative MRI presenting incomplete removal of up-migrated disc material at the L3/4 level. A1 and B1, preoperative; A2 and B2, postoperative. 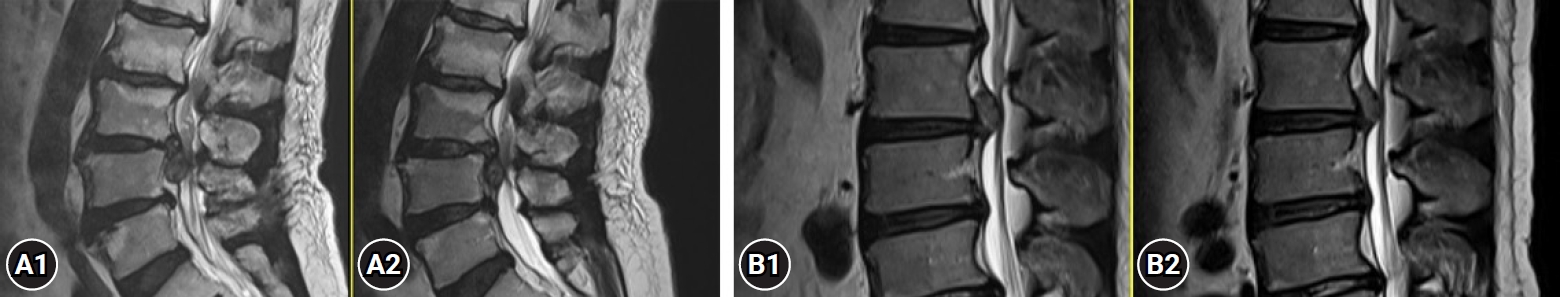
Figure 2.Representative magnetic resonance images present a recurrent disc rupture after a successful removal of disc materials. Depict the preoperative image (A), immediate postoperative image (B), and final follow-up image (C), respectively. Arrows indicate disc materials. 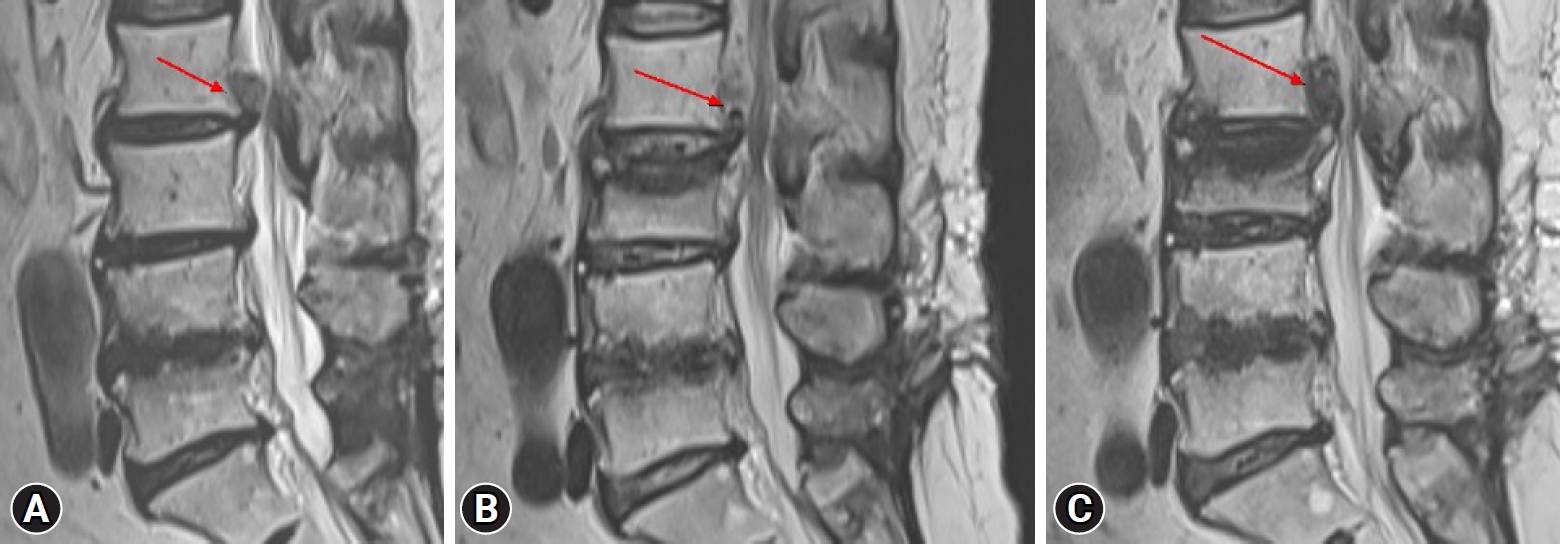
Figure 3.(A1 and A2) Representative sagittal T2-weighted images demonstrate exiting roots located adjacent to the intervertebral disc (arrow), just ventral to the superior articular process. In such cases, it is crucial to exercise extra caution to prevent any injury to the exiting root. (B) The exiting root is observed to run more cranially to the endoscope landing area in this image, indicating a relatively lower risk of injury. 
REFERENCES1. Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:E326–32.
2. Hur JW, Lee S, Kim BJ, Kim SH. The growing popularity of MISS: a focus on endoscopic surgery for the cervical and thoracic spine. J Minim Invasive Spine Surg Tech 2023;8:5–8.
3. Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine (Phila Pa 1976) 2007;32:1735–47.
4. Wu PH, Kim HS, Choi DJ, Gamaliel YHT. Overview of tips in overcoming learning curve in uniportal and biportal endoscopic spine surgery. J Minim Invasive Spine Surg Tech 2021;6(Suppl 1):S84–96.
5. Wu PH, Kim HS, Jang IT. A narrative review of development of full-endoscopic lumbar spine surgery. Neurospine 2020;17(Suppl 1):S20–33.
6. Choi KC, Lee JH, Kim JS, Sabal LA, Lee S, Kim H, et al. Unsuccessful percutaneous endoscopic lumbar discectomy: a single-center experience of 10,228 cases. Neurosurgery 2015;76:372–80; discussion 380-1; quiz 381.
7. Kim HS, Wu PH, Jie Chin BZ, Jang IT. Systematic review of current literature on clinical outcomes of uniportal interlaminar contralateral endoscopic lumbar foraminotomy for foraminal stenosis. World Neurosurg 2022;168:392–7.
8. Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976) 2008;33:973–8.
9. Park CH, Park ES, Lee SH, Lee KK, Kwon YK, Kang MS, et al. Risk factors for early recurrence after transforaminal endoscopic lumbar disc decompression. Pain Physician 2019;22:E133–8.
10. Choi SJ, Ham CH, Moon HJ, Kim JH, Park YK, Kwon WK. Full endoscopic decompression for a misdiagnosed far-out syndrome (L5/S1 extraforaminal stenosis) in an elderly patient with L5 radiculopathy: case report. Asian J Pain 2022;8:1.
11. Kwon WK, Kelly KA, McAvoy M, Sivakanthan S, Ogunlade J, Yap NKY, et al. Full endoscopic ligamentum flavum sparing unilateral laminotomy for bilateral recess decompression: surgical technique and clinical results. Neurospine 2022;19:1028–38.
13. Ahn Y. Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices 2012;9:361–6.
14. Lewandrowski KU. Incidence, management, and cost of complications after transforaminal endoscopic decompression surgery for lumbar foraminal and lateral recess stenosis: a value proposition for outpatient ambulatory surgery. Int J Spine Surg 2019;13:53–67.
15. Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, et al. Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 2013;37:1511–7.
16. Kim JH, Ham CH, Kwon WK. Current knowledge and future therapeutic prospects in symptomatic intervertebral disc degeneration. Yonsei Med J 2022;63:199–210.
17. Ahn Y, Kim JU, Lee BH, Lee SH, Park JD, Hong DH, et al. Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine 2009;10:595–602.
18. Sairyo K, Matsuura T, Higashino K, Sakai T, Takata Y, Goda Y, et al. Surgery related complications in percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest 2014;61:264–9.
19. Ahn Y, Keum HJ, Lee SG, Lee SW. Transforaminal endoscopic decompression for lumbar lateral recess stenosis: an advanced surgical technique and clinical outcomes. World Neurosurg 2019;125:e916–24.
20. Zhou C, Zhang G, Panchal RR, Ren X, Xiang H, Xuexiao M, et al. Unique complications of percutaneous endoscopic lumbar discectomy and percutaneous endoscopic interlaminar discectomy. Pain Physician 2018;21:E105–12.
21. Ahn Y, Lee U. Use of lasers in minimally invasive spine surgery. Expert Rev Med Devices 2018;15:423–33.
22. Fan N, Yuan S, Du P, Wu Q, Wang T, Wang A, et al. Complications and risk factors of percutaneous endoscopic transforaminal discectomy in the treatment of lumbar spinal stenosis. BMC Musculoskelet Disord 2021;22:1041.
23. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–9.
24. Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 2007;6:521–30.
25. Hasan S, White-Dzuro B, Barber JK, Wagner R, Hofstetter CP. The endoscopic trans-superior articular process approach: a novel minimally invasive surgical corridor to the lateral recess. Oper Neurosurg (Hagerstown) 2020;19:E1–10.
26. Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am 1998;80:1728–32.
27. Ghobrial GM, Theofanis T, Darden BV, Arnold P, Fehlings MG, Harrop JS. Unintended durotomy in lumbar degenerative spinal surgery: a 10-year systematic review of the literature. Neurosurg Focus 2015;39:E8.
28. Cammisa FP Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663–7.
29. Sen RD, White-Dzuro G, Ruzevick J, Kim CW, Witt JP, Telfeian AE, et al. Intra- and perioperative complications associated with endoscopic spine surgery: a multi-institutional study. World Neurosurg 2018;120:e1054–60.
30. Telfeian AE, Shen J, Ali R, Oyelese A, Fridley J, Gokaslan ZL. Incidence and implications of incidental durotomy in transforaminal endoscopic spine surgery: case series. World Neurosurg 2020;134:e951–5.
31. Kim HS, Raorane HD, Wu PH, Heo DH, Sharma SB, Jang IT. Incidental durotomy during endoscopic stenosis lumbar decompression: incidence, classification, and proposed management strategies. World Neurosurg 2020;139:e13–22.
32. Matsumoto M, Hasegawa T, Ito M, Aizawa T, Konno S, Yamagata M, et al. Incidence of complications associated with spinal endoscopic surgery: nationwide survey in 2007 by the Committee on Spinal Endoscopic Surgical Skill Qualification of Japanese Orthopaedic Association. J Orthop Sci 2010;15:92–6.
33. Shin JK, Youn MS, Seong YJ, Goh TS, Lee JS. Iatrogenic dural tear in endoscopic lumbar spinal surgery: full endoscopic dural suture repair (Youn's technique). Eur Spine J 2018;27(Suppl 3):544–8.
34. Soma K, Kato S, Oka H, Matsudaira K, Fukushima M, Oshina M, et al. Influence of incidental dural tears and their primary microendoscopic repairs on surgical outcomes in patients undergoing microendoscopic lumbar surgery. Spine J 2019;19:1559–65.
35. Oertel JM, Burkhardt BW. Full endoscopic treatment of dural tears in lumbar spine surgery. Eur Spine J 2017;26:2496–503.
36. Ham CH, Kwon WK, Moon HJ, Kim JH, Park YK, Hofstetter CP. Use of prophylactic perioperative antibiotics for lumbar spinal fusions: A nationwide population-based cohort study. J Infect Public Health 2023;16:354–60.
37. Shaffer WO, Baisden JL, Fernand R, Matz PG; North American Spine Society. An evidence-based clinical guideline for antibiotic prophylaxis in spine surgery. Spine J 2013;13:1387–92.
38. Mahan MA, Prasse T, Kim RB, Sivakanthan S, Kelly KA, Kashlan ON, et al. Full-endoscopic spine surgery diminishes surgical site infections - a propensity score-matched analysis. Spine J 2023;23:695–702.
39. Choi G, Kang HY, Modi HN, Prada N, Nicolau RJ, Joh JY, et al. Risk of developing seizure after percutaneous endoscopic lumbar discectomy. J Spinal Disord Tech 2011;24:83–92.
40. Ahn Y, Jang IT, Kim WK. Transforaminal percutaneous endoscopic lumbar discectomy for very high-grade migrated disc herniation. Clin Neurol Neurosurg 2016;147:11–7.
41. Choi KC, Shim HK, Kim JS, Cha KH, Lee DC, Kim ER, et al. Cost-effectiveness of microdiscectomy versus endoscopic discectomy for lumbar disc herniation. Spine J 2019;19:1162–9.
42. Kim HS, You JD, Ju CI. Predictive scoring and risk factors of early recurrence after percutaneous endoscopic lumbar discectomy. Biomed Res Int 2019;2019:6492675.
43. Lin YP, Wang SL, Hu WX, Chen BL, Du YX, Zhao S, et al. Percutaneous full-endoscopic lumbar foraminoplasty and decompression by using a visualization reamer for lumbar lateral recess and foraminal stenosis in elderly patients. World Neurosurg 2020;136:e83–9.
44. Hahn BS, Jang JW, Lee DG, Park CK. Current status of biportal endoscopic decompression for lumbar central stenosis. J Minim Invasive Spine Surg Tech 2021;6(Suppl 1):S164–70.
|
|
||||||||||||||||||||||||||||||||||||||||||||