INTRODUCTION
Spondylolysis mainly affects children and young athletes. Because its symptoms can be challenging to treat, it can force these young individuals to refrain from practicing sports and, in many cases, to prematurely end their careers. This condition is caused by repetitive traumas in genetically susceptible patients, mainly young athletes [1]. The nonsurgical treatment applied to spondylolysis cases comprises using orthoses, restricting physical activities, as well as the implementation of a series of physical therapy sessions. These measures are known to relieve pain, in most patients. However, their effectiveness depends on injury’s response to treatment [2]. Surgical treatment is indicated when nonsurgical approach fails, after 6-month treatment [3]. The selected surgical approach (classically done through conventional surgery) can follow the conventional way or an endoscopic technique, mainly when there is no degeneration or severe disc instability in direct pars’ repair [4]. Endoscopic techniques are minimally invasive procedures leading to effective treatments. Because they require small incisions, they have several advantages, such as quick recovery, less pain, reduced risk of infections and nearly imperceptible scars; these factors turn them into a versatile and safe option in different medical specialties [5]. The aim of the current study is to describe both the use and the outcomes of a new alternative spondylolysis treatment based on percutaneous endoscopic approach.
CASE REPORT
A 33-year-old male individual, automotive mechanic, suffered from refractory low back pain (visual analogue scale [VAS] 8) for 7 years. He reported non-specific low-intensity irradiation to the right lower limb (VAS 2) and presented moderate (26%) Oswestry Disability Index (ODI). His pain worsened under prolonged orthostasis and when he lied down. He sought medical assistance due to sleep-quality loss, because he had been waking up every night in pain, for the past years.
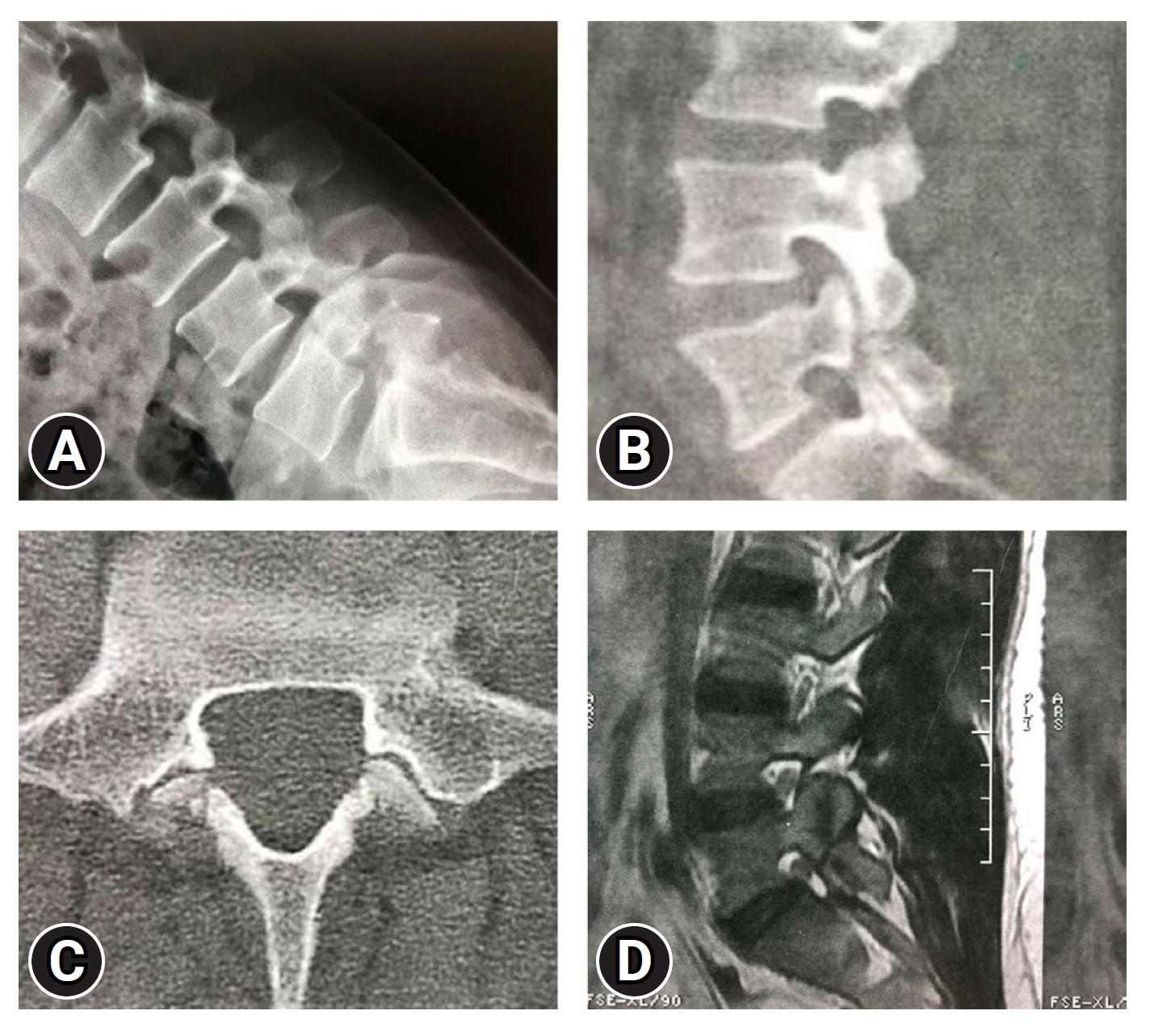
Dynamic radiography computed tomography (CT) scan and magnetic resonance imaging (MRI) of the lumbar spine have evidenced bilateral spondylolysis of the L5 pars interarticularis (Figure 1), without evidence of any other pathological abnormality capable of leading to similar clinical condition. There was no dynamic hypermobility or relevant degenerative alteration. The pars defect was clear; moreover; it presented sclerotic edges and no major reabsorption of the focus. These factors enabled inferring lesion chronicity, with small chances of consolidation, based on conservative measures, as well as indicated good prognosis for the lesion’s primary repair.
Nonetheless, conservative treatment measures were herein adopted to control pain, based on using medication and extensive physical therapy; however, the patient’s condition did not improve. Consequently, surgical treatment based on pars bilateral endoscopic fixation was performed.
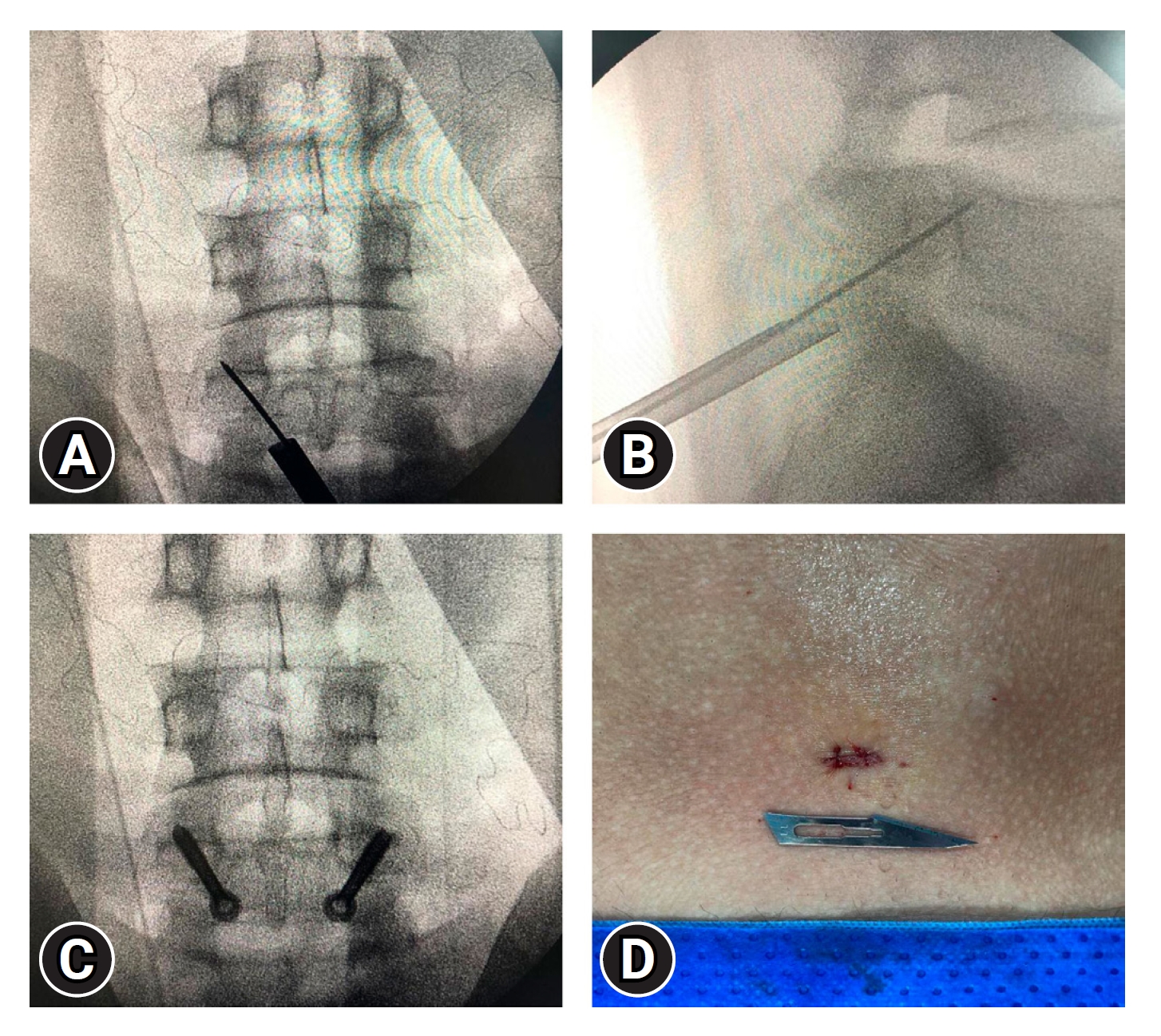
The patient was placed in ventral decubitus position, based on using 2 thoracic cushions (one of them, at iliac crests’ level), and his hip was kept in flexed position to avoid abdominal compression. Fluoroscopy imaging was used to define the entry point by following the lamina inclination. Subsequently, a single 6.0-mm transverse incision was made in the midline, at the height shown by the image at the point indicated at lateral view. It was done to enable good approximation of the posterior edge of the lamina, with sufficient angle to cross it and the pars defect, as well as to go on through the pedicle and to reach the posterosuperior edge of the vertebral body (Figure 2). The entire procedure was performed under general anesthesia and aseptic technique.
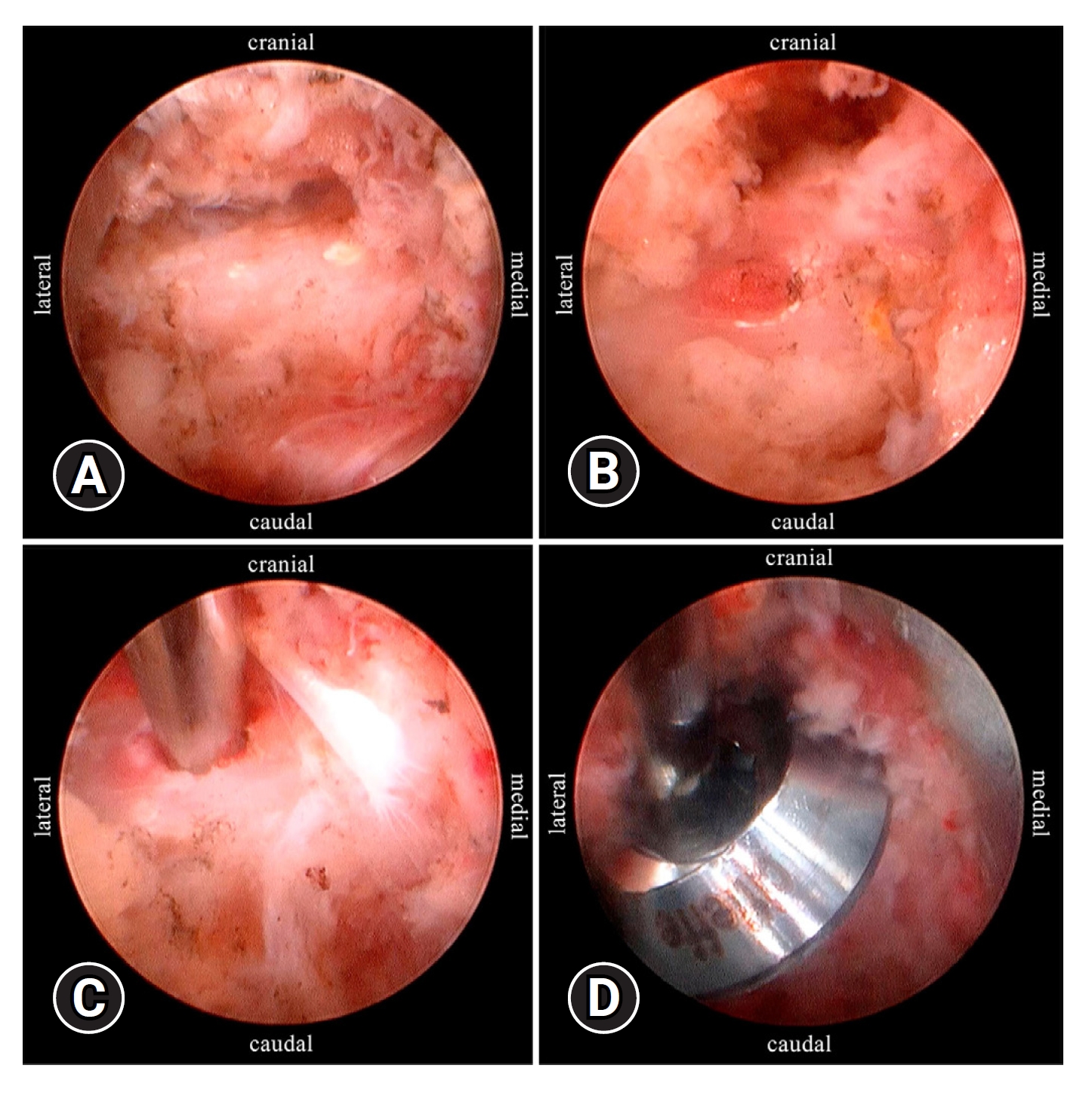
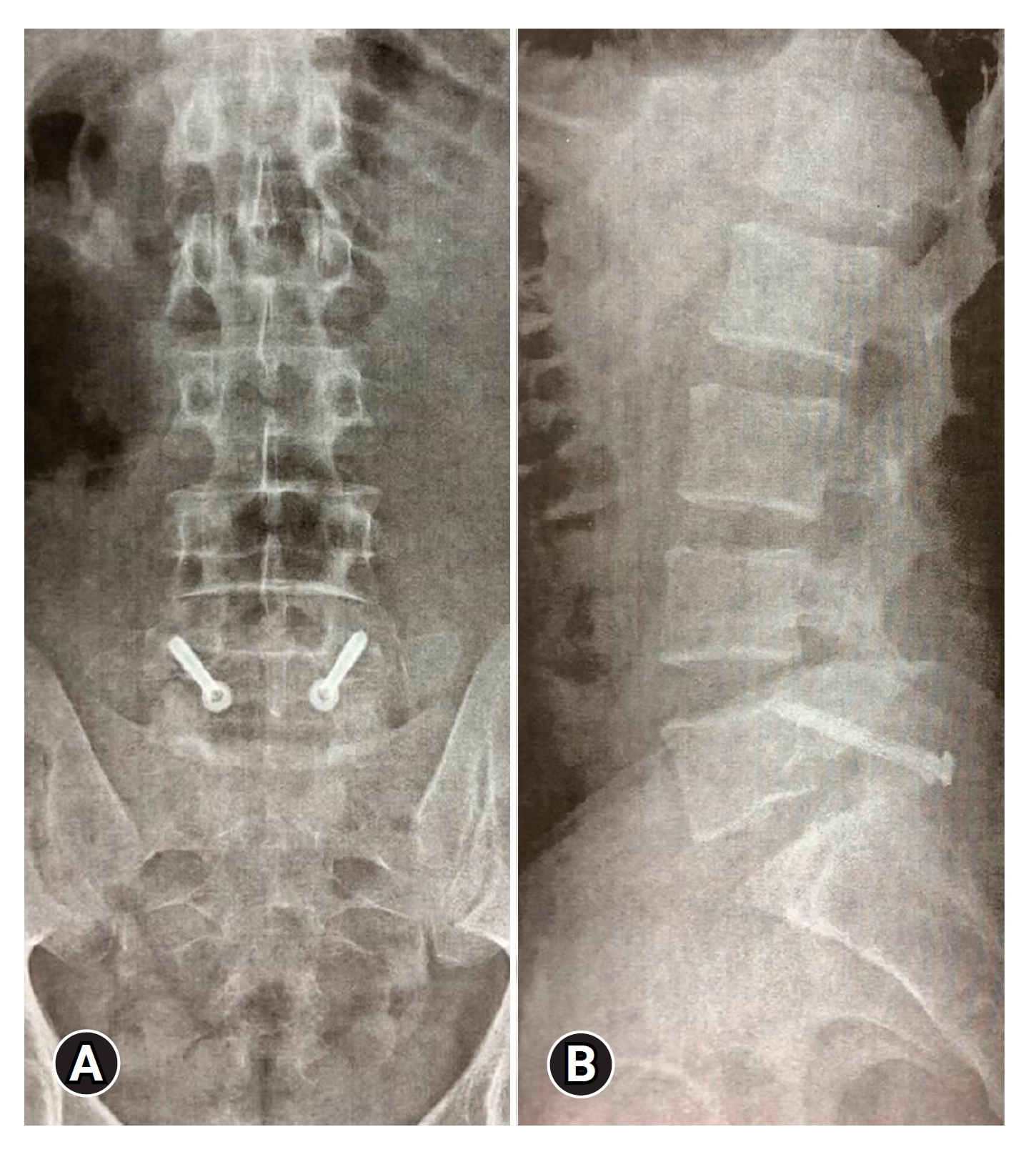
The patient’s skin was displaced through the incision, and the dilator was inserted to either the right or the left of the spinous process. As for the current case, the approach was firstly performed through the left side of the spinous process, by introducing a cannula over the dilator and, then, the scope (with a 3.7-mm working channel). Hemostasis was performed and initial debridement was done with the aid of a flexible bipolar electrode, which was oriented to the posterior edge of the left L5 lamina. A 3.5-mm burr was used to open the entry point, in the center of the posterior edge of this lamina (Figure 3), to enable seeing the cancellous bone and to provide a suitable surface to dock the guide wire. Then, the surgeon introduced a 1.5-mm guide wire through the planned position, also under endoscopic imaging conditions (Figures 2 and 3). Subsequently, cannulated drill guided by fluoroscopy imaging was used for perforation purposes and the implant’s length was measured. Then, a 5.0-mm self-tapping partial thread screw was introduced through the guide wire to provide excellent interfragmentary compression (Figure 4).
The same median incision was used to cross over the spinous process in order to repeat the entire procedure in the right side. The whole procedure required 45 minutes to be concluded, demanded small incision (Figure 2) and led to minimal blood loss.
The patient did not present relevant pain after the procedure and he was discharged after 24-hour antibiotic prophylaxis. He reported fully nocturnal pain improvement and uninterrupted sleep, at the first postoperative day. He started a 20-session protocol-based physical therapy at the third postoperative day and achieved excellent recovery. He was also advised by the medical staff to take time away from any physical work for the following 3 months. The patient remains mostly asymptomatic, so far, and he also maintains improved sleep quality. Moreover, he currently records ODI of 8%, lumbar VAS of 2, and lower limbs VAS of zero, on a daily basis, 3.5 years after surgery. Current postoperative imaging has shown spine stability (based on dynamic radiography), pars’ consolidation (based on CT scan) and no disc degeneration progression (based on MRI).
This study has been approved by the Institutional Review Board of Center of Biological and Health Sciences, State University of Pará (51883521.3.0000.5174). The authors obtained written informed consent from the patient.
DISCUSSION
Using this endoscopic technique enabled reaching both the precise entry point and the implant’s trajectory through the pars defect. It helped mitigating surgical risks and avoiding nerve injuries [5]. Furthermore, the smaller incision (6.0 mm) and the minimal tissue damage reduced blood loss during the herein performed surgery, in comparison to conventional techniques [6].
Firstly, the most common fixation-screw diameters would either be 3.5-mm or 4.5-mm, in thickness. In this case, the available screw was 5.0 mm thick, and it ensured remarkable compressive strength. A 3.5-mm screw would not be equally suitable to be used in young adults [4]. A 4.5- or 5.0-mm screw (in diameter) should be preferred instead. Using washers is optional, since they may increase interfragmentary compressive strength and prevent the screw head from sinking into the lamina’s edge. Guide wire thickness is also a crucial factor in this procedure. Guide wires thinner than 1.5 mm are harder to be controlled, and it can lead to their inadequate positioning, which, in its turn, can prolong surgical duration and make it harder to pass the wire through the pars defect focus. Thus, 1.5 mm, or thicker, guide wires are the ones recommended, in this particular frame.
Another important point to be discussed lies on the likelihood of making an additional incision to decorticate the defect and to use bone graft [6]. The wire insertion, drilling and screwing processes, themselves, promote a sort of decortication. Although external decortication and bone grafting play important role in improving consolidation, it is also recommended to start surgery by positioning the screws without tightening them, at first and, then, to move on to the external decortication and bone grafting processes, in order to finish the procedure by tightening the screw.
Surgery time (45 minutes) was shorter than the one reported in similar studies, regardless of whether they adopted the minimally invasive technique or conventional approaches. Widi et al. [7] reported mean duration of 65 minutes (range, 55–80 minutes) for surgery performed based on the percutaneous direct pars repair technique. Ghobrial et al. [8] reported mean duration of 189±29 minutes for the direct pars repair technique, based on minimally invasive approach, whereas Li et al. [9] described mean surgery time of 216.67±62.60 minutes for procedure based on the conventional Buck technique. Surgeon's experience with endoscopic procedures, and the fact that minimally invasive techniques require shorter surgical time, are some of the explanations for the herein addressed difference in surgical time.
Therefore, the main advantages of this technique over the traditional open repair of the pars defect possibly rely on reducing operative time, blood loss, hospital stay, postoperative pain, muscle damage and infection rate. Studies comparing the 2 techniques need to be conducted to validate these benefits.
Surgical outcomes remained satisfactory after 3-year-and-a-half follow-up, since the patient presented nocturnal pain improvement and good clinical evolution, which, in its turn, was evidenced by ODI of 8%, lumbar VAS of 2 and by no pain in the lower limbs. These findings are comparable to those observed in similar studies focused on investigating the effectiveness of pars interarticularis endoscopic fixation in increasing pain relief rate, in shortening hospital stay and in enabling faster patients’ recovery to perform daily activities by reducing muscle tissue damage during minimally invasive procedures [10,11]. However, Lau et al. [12] recorded higher complication rate in the first 10 surgical procedures performed during the process to learn how to use these correction techniques in patients with spondylolysis, spondylolisthesis and spondylosis. Therefore, surgeons' learning curve can significantly affect intervention outcomes.
CONCLUSION
The endoscopic pars fixation technique has the potential to be used for spondylolysis treatment purposes, since it enables pain relief and is mildly aggressive to muscle tissues, during surgery. Case series, clinical trials and comparative studies should be encouraged to confirm the safety and benefits of this technique.