AbstractObjectiveAwake spine surgery has improved patient outcomes in common orthopaedic procedures. Integrating it into spine surgery is of interest to surgeons since it may reduce the difficulties and complications associated with general anaesthesia. The demand for safe spine surgery is rising due to healthcare improvements and increasing ageing population. This study aimed to assess the safety and feasibility of spine surgery under spinal anesthesia for elderly patients aged 65 and older.
MethodsIn a retrospective review, 83 lower lumbar spine surgeries performed under spinal anesthesia by a single surgeon at a single hospital from 2015 to 2019 were examined. All procedure-related data was collected prospectively for analysis. This study explored demographic characteristics, surgical features, perioperative concerns, and anesthesia-related obstacles in spine surgery under spinal anaesthesia.
ResultsThis study included 83 patients aged 65 years and older. Following follow-up, visual analogue scale and Oswestry Disability Index scores considerably improved (p<0.05). Patients in the American Society of Anesthesiologists physical characteristics classification grade II had the highest count. The most common level was L4–5. About 7.2% of patients needed multiple spinal procedures. The average induction time was 20.2±9.6 minutes. The average intraoperative operation lasted 84.0±17.20 minutes. The shifting-out process took 7.95±2.10 minutes to start. The mean intraoperative arterial blood pressure was 70.7±10.8 mmHg, and the mean heart rate was 69.0±7.2 beats per minute. The average postoperative analgesia initiation time was 79.9±7.7 minutes. The average postoperative stay was 3.02±0.83 days. In 10.8% of individuals, cerebrospinal fluid was found. 1.2% of patients experienced postoperative hypotension, 12% experienced nausea and vomiting. Infection occurred in 2.4% of patients, and 14.5% experienced post-operative urinary retention.
INTRODUCTIONWith betterment in healthcare and increasing geriatric population in developing countries, the need and want to stay pain free has been increasing among this population group. The elderly demographic currently expresses a desire to lead a life free from pain, resulting in a rise in the frequency of lumbar spine decompression and fusion procedures [1]. The perceived risk associated with performing spine surgeries on the elderly population was mitigated in recent years due to advancements in anesthesia regimens. The efficacy of surgery in alleviating pain associated with spinal stenosis surpasses that of non-surgical therapy options [2,3]. Historically, awake surgery has been employed for craniotomies, although in recent years, there has been a growing prevalence of utilizing this technique for spine procedures as well [4].
A German surgeon named August bier used cocaine via lumbar puncture as the first person to ever give spinal anesthesia for spine surgery [5]. Even though there are cases of spinal anesthesia for spine surgery that date back to 1960s, eventually with the introduction of complex lumbar and long segment surgeries the complacency to general anesthesia started and eventually patients were not offered a choice of spinal anesthesia with general anesthesia becoming the standard. On the contrary to this, Lessing et al. [6] have described a 5-level lumbar fusion done under spinal anesthesia in a 72-year-old male successfully without any complications.
Many such studies in the recent past have been gaining much popularity as spine surgery is leaning towards minimally invasive techniques to decrease muscular stripping and provide patients with a much better outcome of which regional anesthesia has become a vital part.
General anesthesia is currently the standard followed in most centers for conducting spine surgery as literature gives us assurance of its safety. Spine surgery may require lengthy operative time due to unpredictability, and invasiveness of the procedure needing good airway control achieved only with general anesthesia. This is where minimally invasive surgery plays a huge role in changing the dynamics of how we perceive spine surgery from the surgeons and the anesthetist point of view. Many studies in the past have shown that the use of spinal anesthesia can reduce the use of vasopressors, need for transfusion, intraoperative hypotension and increase general hemodynamic stability in elderly patients with comorbidities, due to the lack of rostral spread of isobaric anesthetics to cardiac baroreceptors in spinal anesthesi [7,8]. Another aspect seen in the elderly population is the chances of postoperative delirium which are as high as 40% in general anesthesia, while it is hypothesized that spinal anesthesia decreases the chances of post operative delirium and dementia as it does not require deep sedative techniques [9].
Enhanced recovery after surgery (ERAS) is a novel concept that integrates perioperative and postoperative interventions aimed at facilitating expedited patient recovery and reducing the psychological and physiological burdens associated with surgical procedures, ultimately enhancing the overall patient experience. The ERAS protocol encompasses a range of multivariate procedures, such as preoperative education and counselling, preoperative optimization, smoking and alcohol cessation, pre-emptive analgesia, and various other aspects [10,11]. Another aspect of this protocol involves the utilization of regional or spinal anesthesia in spine surgeries.
Despite the advancements in ERAS protocols and the prevalent adoption of spinal anesthesia by orthopedic surgeons in lower limb and arthroplasty surgery, there persists a reluctance to employ these techniques in spine surgeries. The obstacles appear to be influenced more by the preferences of surgeons and the comfort levels of anesthetists, rather than being primarily rooted in scientific considerations. The lack of awareness and exposure to spinal anesthesia, in contemporary spine practice is evident due to the limited utilization of this method in spine surgeries and insufficient training among surgeon/anesthetist teams. Numerous prior research has demonstrated that spinal anesthesia yields superior outcomes compared to general anesthesia, as evidenced by diminished perioperative expenses, lower utilization of pain-related anesthesia, and decreased incidence of postoperative nausea and vomiting [7,12,13].
While numerous studies have been conducted on spinal anesthesia in the setting of the spine, there is a paucity of research specifically focused on geriatric population in this regard. This study presents an analysis of the experiences of 83 elderly patients who underwent lumbar spine procedures for degenerative spine pathologies causing compression as seen in lumbar canal stenosis or patients with disc pathologies, including both fusion and nonfusion procedures conducted under spinal anesthesia (given at 1 or 2 levels above the operative level). The study aims to investigate the potential advantages and risks associated with these surgeries by examining various perioperative and intraoperative outcomes.
MATERIALS AND METHODSAn analysis was conducted on a cohort of 85 patients who underwent lumbar spine surgery for degenerative spinal stenosis under spinal anesthesia at a single institute (Bombay Hospital and Medical Research Institute) by a single surgeon. The data used for this analysis consisted of longitudinal prospective follow-up data collected from the period of 2016 to 2020. The need for approval was waived off from the local ethics committee, specifically the Institutional Review Board. Informed consents were obtained from all patients for the procedures. Furthermore, the potential utilization of their data for subsequent research analysis was thoroughly elucidated to each individual. The treatment approach implemented in our study involved an initial phase of conservative therapy, which encompassed pain management strategies and the administration of epidural steroid injections, for a minimum duration of 6 months.
The study’s inclusion criteria had a case series of individuals aged 65 years and older who exhibited symptomatic lumbar pathology, specifically mechanical low back pain and radiculopathy, claudication with or without neuro-deficit, involving less than 3 levels at the L3–4/L4–5/L5–S1 levels. These symptoms were attributed to a range of aetiologies, including degenerative, dysplastic, and isthmic spondylolisthesis, degenerative lumbar canal stenosis with instability, and prolapsed intervertebral disc. Patients with minimum follow-up period of 2 years were included in the study.
The exclusion criteria for this study consisted of individuals who needed revision spine surgery, those with infections, tumours, Cauda equina syndrome, individuals with back pain or radiculopathy caused by factors outside of the spine, individuals who needed surgery at higher lumbar levels (specifically L1–2), and patients with low Ejection fraction under 55% and those with a short follow-up period. The administration of anesthesia for all surgical procedures was overseen by a sole anaesthesiologist, utilizing a consistent anesthetic approach. The demographic parameters of the patients, including age, sex, and American Society of Anaesthesiologists (ASA) physical status, were recorded. Based on the established criteria for inclusion and exclusion, individuals who had counselling for surgery were included in the study. In accordance with the established criteria for the study, spinal anesthesia was given to all included participants. The participants received comprehensive counselling and were provided with a detailed explanation of the advantages and disadvantages connected with this approach. A total of 85 patients voluntarily agreed to undergo spinal anesthesia and met the predetermined criteria for inclusion in the study.
1. Anesthesia TechniqueWe employ spinal anesthesia, utilizing the sitting position for optimal administration. The selected vertebral spaces for the procedure include L2–3, L3–4, and L4–5, with the level of spinal anesthesia set at T8. For extended surgical durations, we may adjust the level to T6. The spinal drugs employed for this technique include bupivacaine 0.5%, levobupivacaine 0.5%, and ropivacaine 0.75%. To enhance the efficacy of spinal anesthesia, we incorporate additives such as Fentanyl (10–20 μg), Buprenorphine (60–80 μg), and Clonidine (15 μg).
Following the spinal anesthesia, the patient undergoes proning after 15 minutes, contributing to the effectiveness of the procedure. During the prone position, sedation is administered, typically involving the use of midazolam and Nalbuphine (Fortwin). This comprehensive approach ensures the patient's comfort and the success of the spinal anesthesia in our spine surgery protocol.
2. Operative TechniqueThe patients who underwent decompression or fusion surgeries were approached using a 2.5-cm paramedic incision, positioned 3–5 cm away from the midline on the side that exhibited more severe symptoms. The procedure of tubular decompression was performed using 22-mm tubes from the METRx system, manufactured by Medtronic (Minneapolis, MN, USA). This was done in conjunction with a partial unilateral or bilateral laminotomy (over the top), foraminotomy and inferior partial facetectomy, all of which were guided by microscopic visualisation. In situations necessitating interbody fusion, the procedure involved further inferior facetectomy, discectomy, preparation of the end plate, and insertion of a cage along with the utilization of autograft taken from the local region. Cannulated pedicle screws were introduced subsequent to the introduction of a guidewire through Cook's needle, followed by sequential tapping using dilators and a tap, all under the guidance of fluoroscopy (Figure 1). Rod was introduced to a device via a distinct proximal stab incision. A comprehensive wash was carried out, followed by sequential layering for closure. Upon the conclusion of the procedure, the patient was afterwards transported to the postanaesthesia care for the purpose of recovery.
The perioperative parameters that were assessed in this study included the duration of surgery, blood loss during surgery, time from entering the operating theatre to incision, occurrence of cerebrospinal fluid (CSF) leak during surgery due to dural tear or dural needle prick, time from bandaging to exiting the operating theatre, need for postoperative analgesia, episodes of postoperative emesis, occurrence of urinary retention, postanaesthesia care unit (PACU) time, and duration of hospital stay. Postoperatively pain management was done using intravenous acetamiophen and tramadol for only first postoperatively and all patients were shifted to oral acetaminophen and tramadol if needed for a period of 5 days. These parameters were carefully documented, and the collected data was then extrapolated to evaluate the study's results. Postoperative complications were systematically recorded and categorised into general and neurological domains. General difficulties encompassed fever, wound infection, cardiac and pulmonary issues, as well as urinary tract infections. Neurological complications consisted of CSF leaks following surgery and the occurrence of neurological deficits.
RESULTSA total of 85 patients were included in the study but 2 patients were lost to follow-up. Forty-one males (49.4%), 42 females (50.6%) were included in study aged from 66 to 75 years (70.4±4.1 years). Their body mass index ranged from 28 to 38 kg/m2 (33.42±4.9 kg/m2). Patients consuming alcohol were 19 (22.9%) whereas those who were chronic smokers were 17 (20.5%). Hypertension was amongst 41 patients (49.4%) and 30 (36.1%) were diabetic. The level of fusion done ranged from 37 (44.6%) that had L3–4, 69 (83.1%) had L4–5 whereas L5–S1 was seen in 16 (19.3%). All participants included in the study were followed-up for an average period of 12.8±0.9 months. The number of surgeries where fusion was carried out was 33 (39.8%, Table 1).
The ASA physical status classification grade was II ranging up to III (2.3±0.6). The requirement for a repeat spinal was in 6 patients (7.2%). Also, the induction time ranged from 10 to 30 minutes (20.2±9.6 minutes). Whereas the total operative time was 68 to 100 minutes (84.0±17.2 minutes). Time taken to leave the operative room was about 6 to 10 minutes (7.95±2.10 minutes). The total blood loss calculated was about 104 to 140 mL (124.3±19.6 mL). Estimated intra operative mean arterial blood pressure (MABP) was 60 to 80 mmHg (70.71±10.8 mmHg). The intraoperative heart rate recorded was around 62 to 75 beats per minute (69.0±7.2 beats). Average number of days (Table 2) for the postoperative stay was 2 to 4 days (3.02±0.83 days).
Complications were limited and varied from postoperative urinary retention that occurred in about 12 patients (14.5%). Followed by nausea and vomiting prevalent in 10 patients (12%). CSF from needle puncture which was seen in 9 patients (10.8%) which were all managed without any active intervention with water tight closure. Infection was limited to 2 patients (2.4%), both of which were staphylococcus aureus infections treated with intravenous/oral antibiotics alone (Table 3). Lastly, postoperative hypotension was seen only in 1 (1.2%).
Preoperative visual analogue scale (VAS) score was average mean of 7.31±0.78 which significantly reduced to be an average score of 2.86±0.68 (Table 4). (p<0.05) Similarly the Oswestry Disability Index (ODI) scoring reduced significantly post operatively to 26.39±4.08 which was 71.02±5.51 preoperatively (p<0.05, Figure 2).
DISCUSSIONIn this study, we provide our findings of a cohort of 83 elderly individuals who underwent lumbar spine procedures, encompassing both fusion and nonfusion techniques. These interventions were performed using minimally invasive approaches under spinal anesthesia. Over a period of a decade performing lumbar spine surgeries in regional anesthesia our experience in the elderly population seems to be of utmost importance for literature. The study conducted exhibited an average operative time of 84.0±17.2 minutes. The existing literature requiring general anesthesia demonstrates consistent findings, with an average duration of approximately 100 minutes [14,15]. The VAS and ODI patterns at 6 months and 1year and final follow-up in our study significantly improved in comparison to preoperative values (p<0.05).
In contrast to the typical cohorts observed in previous studies, most of our patients exhibited ASA physical status classification grades II and III, indicating a higher level of risk. However, it is noteworthy that all the elderly patients underwent successful surgeries using spinal anesthesia. The average induction time for this procedure was a mere 20.2±9.6 minutes, and none of the patients necessitated a switch to general anesthesia. Another notable observation pertained to the duration of time required for all patients to be transferred from the observation area (PACU) following surgery. On average, this process took only 7.95±2.1 minutes. This expedited transfer can be attributed to the supplementary analgesic effects of spinal anesthesia during the postoperative phase, which ensured that all patients remained conscious, comfortable, and devoid of pain. A study conducted by Pierce et al. [16] similarly yields findings that are close to our own. Other studies which were done on younger population (<65 years), showed similar results with shorter hospital stay, well controlled pain and good patient satisfaction [17].
Regarding other perioperative complications, it was observed that 7.2% of cases required a repeat spinal procedure, while CSF puncture occurred was observed intraoperatively in 10.8% of instances. Notably, none of the patients exhibited symptomatic dural leak and all were managed conservatively with only water tight closure. During the postoperative phase, a mere 1.2% of patients exhibited symptoms of hypotension, while 6% of patients reported experiencing nausea and vomiting. A study done by McLain et al. [18] found a higher incidence of nausea and vomiting in patients who underwent procedure under general anesthesia in comparison to the regional anesthesia group. A comprehensive analysis conducted using a database approach investigated lumbar spine procedures, irrespective of the type of anesthesia employed, and revealed an aggregate incidence of adverse outcomes, including mortality at 16.34%, major complications at 3.23%, and mild complications at 14.57% [19]. According to review research conducted in 2008, it was found that the mortality rates among older individuals following spine procedures were around 10% [20]. Over the decade spine surgery has evolved into better and less invasive techniques to decrease mortality and in our cohort of study population we reported no major complications or mortality.
Regarding hemodynamic stability, the intraoperative MABP was consistently maintained at an average of 70.71±10.8 mmHg, with no observed significant fluctuations in any of the patients. The heart rate during the surgical procedure was also sustained at an average of 69.0±7.2 beats per minute. Prior research has also demonstrated that regional anesthesia exhibits significantly lower alterations in MABP and heart rate compared to general anesthesia [12,21]. In one observed case, the patient experienced bradycardia following prone positioning, which was attributed to the cranial spread of the administered drug. However, this adverse event can be mitigated by ensuring the adequacy of anesthesia level and employing appropriate head elevation techniques to minimize cranial spread. The average estimated blood loss was 124.3±19.6 mL. Additional research involving patients under the age of 65 and comparing general anesthesia with spinal anesthesia demonstrated comparable rates of complications in both groups, as well as minimal fluctuations in intraoperative MABP. However, patients who underwent spinal anesthesia experienced significantly fewer episodes of nausea [22]. According to existing literature, it has been suggested that spinal anesthesia patients experience a decrease in blood loss compared to patients under general anesthesia, primarily attributed to the reduced intrathoracic pressures resulting from spontaneous breathing.
Our study did show a considerably higher rate of post operative urinary retention in 12 patients (14.7%), out of which 4 patients required the use of bladder drainage using a K90 Catheter and the need for catheterization in 6 patients. These could also be attributed to the fact that in elderly population due to weakness in bladder mobility preoperatively due to lumbar spine compression or due to prostate hypertrophy seen in male patients. Studies comparing post operative urinary retention when compared in general and spinal anesthesia, there was a significantly more incidence in spinal anesthesia regarded due to the intrathecal spread in spinal anesthesia [23].
Another concern with regards to spinal anesthesia in our experience is the question whether spinal anesthesia is a viable option for procedures that may last up to 3 hours as the half-life of bupivacaine is 2.7 hours only. Such time related issues could be surgeon specific as different surgeons may require more time in some cases, but studies also report that anesthetic medications do exhibit pronounced and extended effects in geriatric population [20].
Another increasingly common strategy gaining attention is the utilization of epidural anesthesia for lumbar spine cases. This technique enhances the anesthesia effect by means of a catheter and can also be employed in the postoperative phase to effectively manage pain, thereby minimizing the requirement for narcotics. A study done on 111 patients who underwent lumbar spine procedures under epidural anesthesia with light sedation has been already shown to be a safe and feasible option of utilizing conscious sedation where patients can give live intraoperative feedback [24]. This study also shows that the use of epidural anesthesia with local anesthetics that have been diluted by half leads to effective pain relief while causing minimal impairment of motor function in the lower extremities. Conscious sedation is a surgical aid that resembles neuromonitoring. While neuromonitoring is not commonly employed in lumbar spine surgeries and the effects of spinal anesthesia on neuromonitoring are yet to be fully understood, previous studies have indicated that there is no notable disparity in neuromonitoring alterations when comparing patients who underwent surgery with balanced anesthesia versus total intravenous anesthesia [25].
In the context of performing spinal anesthesia for lumbar spine procedures, a crucial factor for ensuring patient safety is the presence of a proficient anesthesia team capable of promptly executing a supraglottic intubation procedure, as the potential for airway compromise is recognized when patients are positioned prone. Additional individuals at high risk include people who have severe cardiopulmonary dysfunction and those who suffer from obstructive sleep apnea. Numerous individuals experience discomfort when remaining awake and in a prone position throughout extended surgical procedures. Consequently, in such instances, the administration of mild sedation or, if desired by the patient, the implementation of general anesthesia, which is considered to be a safer alternative, may be warranted. In the context of younger patients, it is advisable to engage in a comprehensive discussion with the patient regarding the selection of anesthesia, by thoroughly considering the advantages and disadvantages, a collaborative decision can be reached, ultimately leading to potential benefits for the patient.
However, this study has several limitations. The present investigation comprised a limited group of patients who underwent a retrospective analysis. Hence, it is imperative to conduct a study including a larger cohort and employ a prospective analysis. In light of the encouraging findings and advantageous consequences demonstrated in our investigation pertaining to spinal anesthesia, it is crucial to undertake a comprehensive comparative analysis vis-à-vis general anesthesia in order to compare all perioperative variables and potential complications. Furthermore, this study did not investigate the efficacy of utilizing just epidural anesthesia for lumbar spine surgery. However, such an investigation is scheduled to be conducted in the future. Nevertheless, the importance of this research resides in its potential to enhance surgeon competency and promote the broad utilization of regional anesthesia for lumbar spine surgeries, therefore reducing the likelihood of complications. The objective of our study is to potentially enhance the feasibility of administering safe spinal anesthesia in the elderly population.
CONCLUSIONThe utilization of spinal anesthesia has become prevalent in the younger demographic for spine procedures, yielding positive outcomes. Our study highlights that employing spinal anesthesia in minimally invasive spine surgery allows the geriatric population to undergo lumbar spine surgeries safely, with minimal occurrence of significant complications. The study has successfully established the viability, safety, and effectiveness of conducting lumbar spine procedures utilizing spinal anesthesia. Nevertheless, the significance persists in the preoperative and perioperative optimization of patients using multimodal methods, aiming to facilitate early mobilization and reduce morbidity in elderly patients.
Figure 1.Case 1: a 68-year-old woman. (A) Preoperative sagittal section of magnetic resonance imaging. (B) Preoperative x-ray in lateral flexion and lateral extension. (C) Postoperative x-ray. 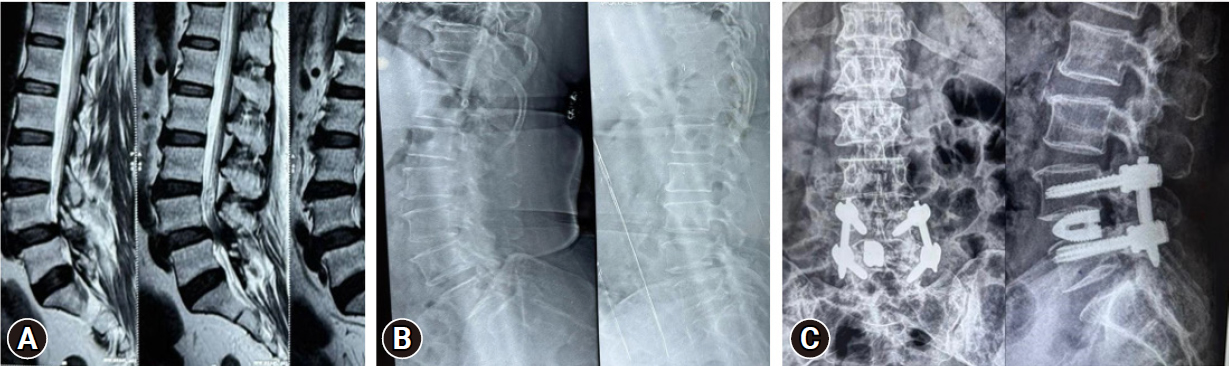
Figure 2.Case 2: a 74-year-old woman. (A) Preoperative x-ray in lateral flexion and lateral extension. (B) Preoperative axial section of magnetic resonance imaging. (C) Postoperative x-ray. 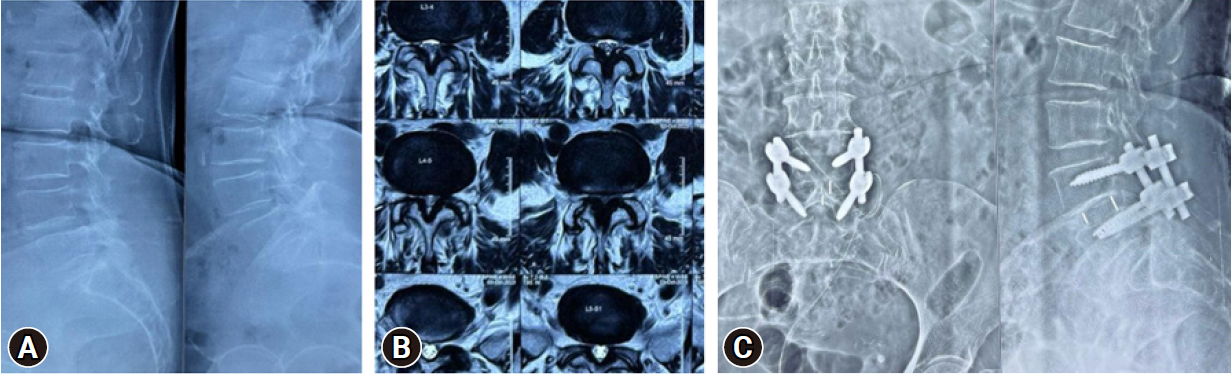
Table 1.Demographic characteristics of the included patients (n=83) Table 2.Perioperative parameters Table 3.Complications (n=83) REFERENCES1. Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259–65.
2. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008;358:794–810.
3. Rodrigues LCL, Natour J. Surgical treatment for lumbar spinal stenosis: a single-blinded randomized controlled trial. Adv Rheumatol 2021;61:25.
4. De Rojas JO, Syre P, Welch WC. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: a review of the modern literature. Clin Neurol Neurosurg 2014;119:39–43.
5. Tait FD, Caglieri G, Matas R, Jonnesco T. The history of anesthesiology. Spinal anesthesia [Internet]. Schaumburg (IL): Wood Library-Museum of Anesthesiology; 1973 [cited 2021 Aug 27]. Available from: https://www.woodlibrarymuseum.org/wp-content/uploads/e-books/wlmrep_3_03pdf.pdf.
6. Lessing NL, Edwards CC 2nd, Lin C, Brown CH 4th. Complex lumbar spine fusion for an elderly patient under spinal anesthesia. Orthopedics 2017;40:e915–7.
7. Deng H, Coumans JV, Anderson R, Houle TT, Peterfreund RA. Spinal anesthesia for lumbar spine surgery correlates with fewer total medications and less frequent use of vasoactive agents: a single center experience. PLoS One 2019;14:e0217939.
8. Finsterwald M, Muster M, Farshad M, Saporito A, Brada M, Aguirre JA. Spinal versus general anesthesia for lumbar spine surgery in high-risk patients: perioperative hemodynamic stability, complications and costs. J Clin Anesth 2018;46:3–7.
9. Brown CH IV, LaFlam A, Max L, Wyrobek J, Neufeld KJ, Kebaish KM, et al. Delirium after spine surgery in older adults: incidence, risk factors, and outcomes. J Am Geriatr Soc 2016;64:2101–8.
10. Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292e298.
11. Bansal T, Sharan AD, Garg B. Enhanced recovery after surgery (ERAS) protocol in spine surgery. J Clin Orthop Trauma 2022;31:101944.
12. Agarwal P, Pierce J, Welch WC. Cost analysis of spinal versus general anesthesia for lumbar diskectomy and laminectomy spine surgery. World Neurosurg 2016;89:266–71.
13. Lessing NL, Edwards CC II, Brown CH IV, Ledford EC, Dean CL, Lin C, et al. Spinal anesthesia in elderly patients undergoing lumbar spine surgery. Orthopedics 2017;40:e317–22.
14. Jhala A, Singh D, Mistry M. Minimally invasive transforaminal lumbar interbody fusion: results of 23 consecutive cases. Indian J Orthop 2014;48:562–7.
15. Patel J, Kundnani V, Raut S, Meena M, Ruparel S. Perioperative complications of minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): 10 years of experience with MI-TLIF. Global Spine J 2021;11:733–9.
16. Pierce JT, Kositratna G, Attiah MA, Kallan MJ, Koenigsberg R, Syre P, et al. Efficiency of spinal anesthesia versus general anesthesia for lumbar spinal surgery: a retrospective analysis of 544 patients. Local Reg Anesth 2017;10:91–8.
17. Khattab MFM, Sykes DAW, Abd-El-Barr MM, Waguia R, Montaser A, Ghamry SE, et al. Spine surgery under awake spinal anesthesia: an Egyptian experience during the COVID-19 pandemic. Neurosurg Focus 2021;51:E6.
18. McLain RF, Tetzlaff JE, Bell GR, Uwe-Lewandrowski K, Yoon HJ, Rana M. Microdiscectomy: spinal anesthesia offers optimal results in general patient population. J Surg Orthop Adv 2007;16:5–11.
19. Saleh A, Thirukumaran C, Mesfin A, Molinari RW. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J 2017;17:1106–12.
20. Cloyd JM, Acosta FL Jr, Ames CP. Complications and outcomes of lumbar spine surgery in elderly people: a review of the literature. J Am Geriatr Soc 2008;56:1318–27.
21. Davis FM, Laurenson VG, Lewis J, Wells JE, Gillespie WJ. Metabolic response to total hip arthroplasty under hypobaric subarachnoid or general anaesthesia. Br J Anaesth 1987;59:725–9.
22. Sarkar S, Banerji A, Chattopadhyaya A, Banerjee S. Lumbar spine instrumented fusion surgery under spinal anaesthesia versus general anaesthesia-A retrospective study of 239 cases. J Clin Orthop Trauma 2021;18:205–8.
23. Niazi AA, Taha MA. Postoperative urinary retention after general and spinal anesthesia in orthopedic surgical patients. Egypt J Anaesth 2015;31:65–9.
|
|
|||||||||||||||||||||||||||||||||||||||