INTRODUCTION
Failed back surgery syndrome (FBSS) is characterized by persistent or recurrent back pain and nerve root pain symptoms after one or more spine surgeries [1]. According to some reports, the incidence of FBSS ranges from 10% to 40% after decompressive laminectomy with or without lumbar spinal fusion [1,2]. The cause of FBSS originates from one or more factors: before, during, and after surgery [2]. This undetected compression from foraminal or lateral recess stenosis and fibrous tissue forming after surgery causes more pain to the patient. If it does not respond to medical treatment, surgery is required to release the compressed nerve structure. However, operation on a patient with previous surgery carries many potential risks, such as dural tears, nerve damage, infection, and other serious events [3]. Most FBSS patients are old with many underlying diseases, so resurgery has a high risk of complications. In such a situation, there is a requirement for minimally invasive intervention; full-endoscopic spine surgery (FESS) can meet this requirement, and there are cases where it can be performed under local anesthesia [4]. Also, compared to open surgery, FESS allows precise access to the location of the nerve structure that needs to be released while being able to pass through adherent fibrous tissue easily [5,6]. For these reasons, reoperation in patients with FBSS is more feasible and less risky. The report aims to describe the treatment results of patients with FBSS at Saint Paul General Hospital.
MATERIALS AND METHODS
We retrospectively reviewed 24 patients with FBSS treated with full-endoscopic surgery at Saint Paul General Hospital from January 2020 to June 2023. Our local institutional review board approved this study. The selection criteria include: (1) Previous lumbar spine surgery; (2) Nerve root pain that may be accompanied by low back pain; (3) Treating doctors recorded signs of compression on computed tomography (CT) and magnetic resonance imaging in the area immediately above or below the intervention site; (4) Surgeon determined the pain generator by selective nerve root block injection; (5) Medical treatment fails. In addition, cases with cauda equina syndrome, unstable spondylolisthesis, infection, tumor, or systemic neurological disease should be excluded. Surgical results are monitored and interviewed according to the visual analog scale (VAS), Oswestry Disability Index (ODI), and MacNab criterion (excellent – no pain, no functional limitation; good – occasional back or leg pain, mild functional limitation; moderate – improvement in general function, but requires changes in work and daily life activities; poor – no improvement in function and pain) at six weeks, six months, one year, and two years after surgery. All patients signed an informed consent form before surgery and before being included in this study. Statistical data were processed using IBM SPSS Statistics ver. 20 (IBM Co., Armonk, NY, USA), comparing ODI and VAS scores simultaneously with the T-test (p<0,05).
RESULTS
1. Patient Population
According to the data we obtained (Table 1), among 24 patients with FBSS, 50% were male, with an average age of 61±15 years. Of these, 50% were patients who had previous bone fusion surgery, 16.7% had previous cement injections, and the remaining had endoscopic surgery, microsurgery, or simple open decompression surgery without fusion. All of these cases were reoperated using uniportal endoscopy at the neurosurgery department, Saint Paul General Hospital, and there were no cases of complications during or after surgery. After the follow-up period, one complication occurred due to nonunion fixation after the removal of the interbody cage and endoscopic fusion. Open surgery was performed for revision. The average surgery time is 94 minutes, with a small amount of blood loss during surgery—impossible to quantify; 58.3% of cases are operated on at the old surgical site—and the rest are operated on at the adjacent location above and below the old surgical area. The new surgical location is in the L34–L51 area, accounting for more than 70%, mainly using interlaminal approach, as the damage is located primarily in the lateral recess or the center of the spinal canal. Regarding the nature of the new pain generators, 83.3% were disc herniations or compression lesions that were not sufficiently decompressed. Notably, 16.7% of cases were compression due to surgical materials (disc graft, cement fragment in the spinal canal).
2. Foraminal Decompression
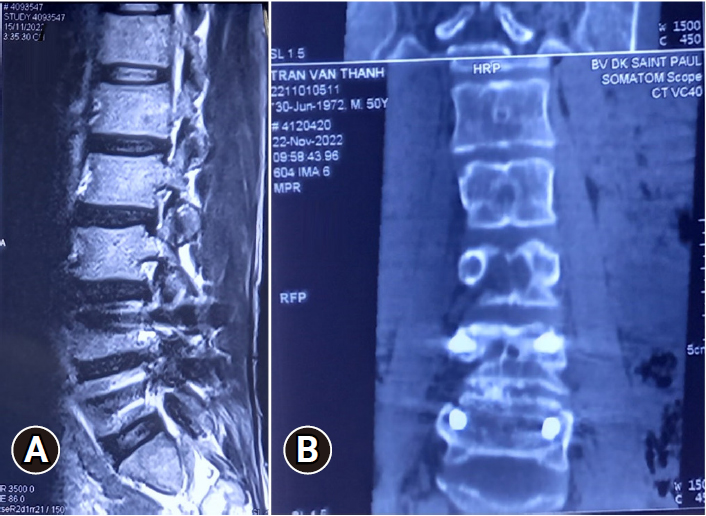
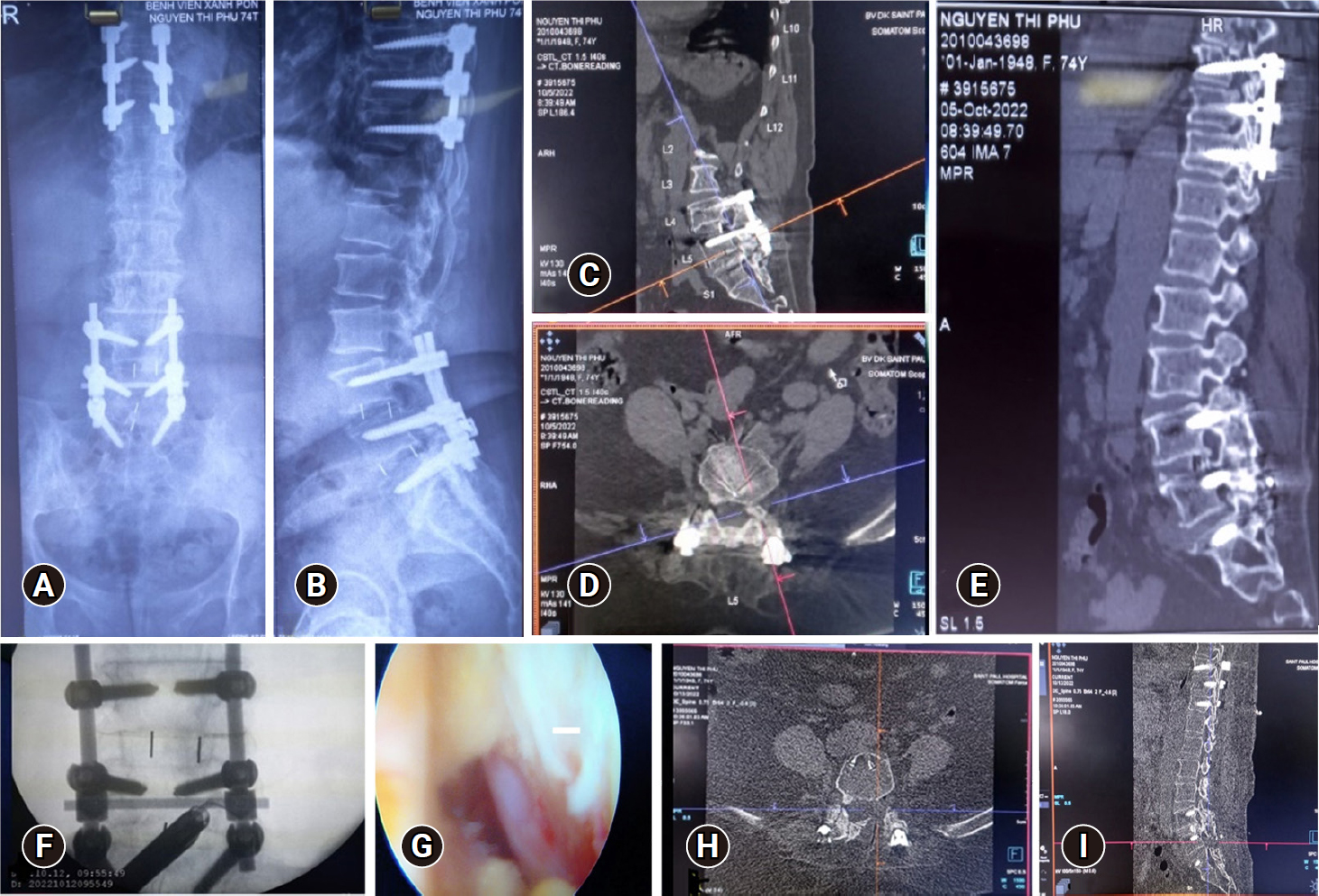
In this study, 3 patients had symptomatic foraminal stenosis causing radiculopathy. Preoperative imaging studies did not show any sign of instability. However, unilateral foraminal stenosis was diagnosed (Figure 1). The preoperative VAS score on the side of radicular pain was 7.3±0.6, the VAS score of back pain was 2.3±0.6, and the preoperative ODI of 54.0±8.1 shows that these patients were severely disabled. All of them underwent endoscopic foraminotomies. At an average follow-up time of 16 months, the average VAS score for leg pain was significantly changed to 2.7±0.6. One patient still had postoperative paresthesias (Table 1).
3. Posterior Decompression
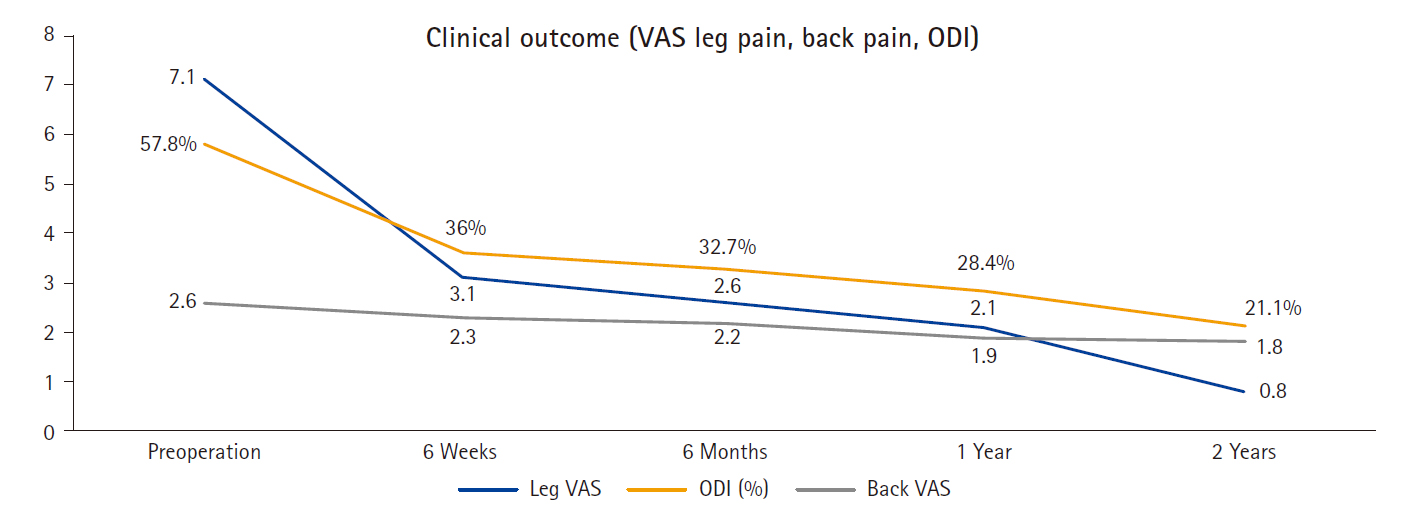
For 21 patients who suffered from lateral stenosis or central stenosis at the same or adjacent level. Patients reported preoperative leg VAS of 7.1±0.7, back VAS of 2.6±0.6, and an ODI of 58.0±9.0 (Table 1). We performed the full-endoscopic procedure via a posterior approach to the previous level with the patient in the prone position under general anesthesia with mild flexion of the lumbar spine. The puncture site was confirmed using fluoroscopy in the anteroposterior and lateral views. Anatomical bony landmarks were located based on the preoperative 3-dimensional CT scan because, in most cases, the laminae were removed in the previous surgery. We performed a 7-mm incision by opening the fascia and inserting the dilator and working cannula, always watching for bone contact nearest the target point to decompress. In case of difficulty in finding the bony contact, we changed to watch for the superior edge of the screw, then followed the screw deeper by bipolar cautery and micropunch to remove soft tissues and visualize the bony tissue. We will check our location by C-arm again on anteroposterior and lateral view to determine whether we have reached the decompress point. Next to it, we exposed the medial margin of the bony area by a blunt dissector and then started to drill with the diamond burr at the point 3 mm away from the medial margin until we could see the inner cortical bone. Opening the epidural space by Kerrison punch where it was still intact, then from this location we dissected medially to find out the compromised nerve root by bipolar cautery and blunt dissector. If there were any adhesion ligament or disc material remnants, they would be removed with a micro punch and grasper. Finally, we check the nerve pulsation for full decompressing and finish the surgery. Endoscopic decompression resulted in an average reduction of VAS by 4 for leg pain at 06 months follow-up, but the backpain VAS score remained unchanged (2.2±0.5) (Figure 2).
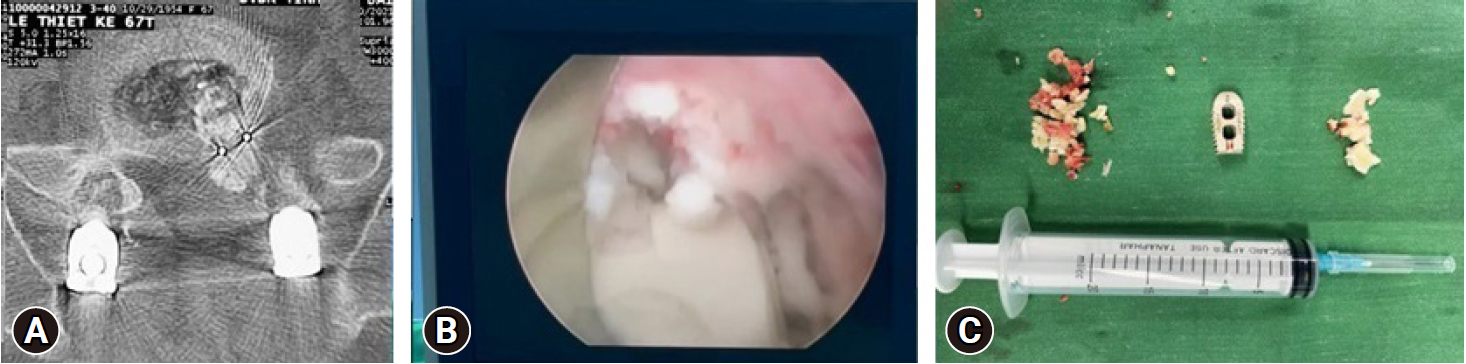
4. Decompression for the Interbody Cage Retropulsion
A 67-year-old man who had undergone an L2–S1 TLIF 10 months previously presented with left-side posterolateral thigh and calf pain. He also had right-side extensor hallucis longus weakness (3/5 strength on examination). Preoperative imaging showed that the L5–S1 interbody cage was displaced posteriorly. That caused very severe lateral recess stenosis (Figure 3). The patient underwent an endoscopic interlaminar removal of the interbody cage and bone graft. However, after removing the cage, the surgeon performed in-situ fusion without adding enough bone graft to improve stability and bone healing. Consequently, the patient resulted in complications, and they had to undergo another surgery to replace the new disc graft and interbody fusion.
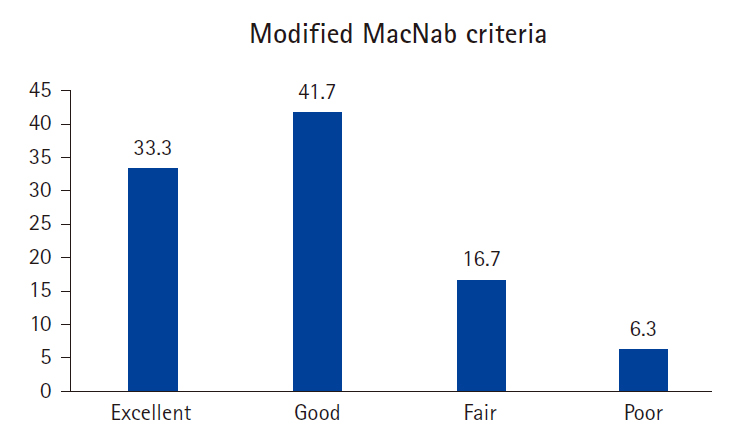
According to the improved MacNab classification, the proportion of FBSS patients with excellent results after endoscopic surgery is 33.3% and good is 41.7%, so the total rate of good and excellent status is 75% (Figure 4). In addition, there were 2 cases (6.3%) with poor results, including 1 case of compression due to a disc graft and 1 case of cauda equina syndrome with paraplegia before the first surgery. However, the majority of the first decompression was not extensive enough, so the patient's symptoms did not improve and were even worse than before surgery.
DISCUSSION
The number of patients undergoing spinal surgery, especially cement injection and spinal fusion, is increasing in other countries and also in Vietnam. With the number growing every day and the age of patients with the disease increasing, in addition to older patients with many different underlying conditions, it is clear that there is a high rate of complications during surgery. Not only that, according to the medical literature, there are more and more reports related to the increased rate of re-surgical instrumentation for cases of spinal fixation surgery, with some studies showing that this rate ranges from 10% to 29% [6].
In order to effectively treat FBSS, it is crucial for clinicians to understand the multifactorial etiology of postsurgical spine syndrome, which is categorized into preoperative, operative, and postoperative factors, as noted by Sebaaly et al. [2]. A spine surgery can fail due to various reasons, such as patient-related factors, poor candidate selection, inadequate decompression, instability, and more. However, before considering surgical intervention, conservative treatments such as pharmacologic, physical, and cognitive behavioral therapy, as well as injections, should be explored [7]. The goal of conservative treatment is to avoid the need for revision surgery and to identify the pain generators via injections. Although spinal cord stimulation trials have shown short-term pain relief, they are not without their own challenges, such as complications, infections, and loss of therapeutic effect [7]. Additionally, this treatment is not available in low-income countries like Vietnam. In our series, we first treated all patients conservatively, with at least 2 selective nerve infiltrations under CT guidance to accurately identify the pain generator before considering operative interventions such as opening and endoscopic surgery.
Opening resurgery for FBSS patients carries the potential risk of serious complications such as nerve damage, dura mater tear, delayed wound healing, infection, adjacent laminar degeneration, bone nonunion, bleeding, and many other complications [5]. For the above reasons, the minimally invasive nature, precise access, and effectiveness of endoscopic surgery are necessary in treating patients with FBSS, especially elderly patients. Even if performed under local anesthesia, the risk of strokes—complications arising during and after general anesthesia—can be reduced [8].
Endoscopic surgery is often considered impossible through the traditional posterior approach due to the axilla or hidden zone of MacNab and scar tissue adhesion [2,4]. However, recent studies have shown that endoscopic surgery via posterior or lateral approach can also access this zone with great success [6,7]. Compared to revision opening surgery, endoscopic surgeries are more beneficial in terms of reduced bleeding, lower risk of infection, and less soft tissue trauma. Although endoscopic surgeries require a steep learning curve, experienced physicians can perform them with minimal risk of serious complications such as dural tear, infection, or hematoma [7].
At Saint Paul General Hospital, FESS is performed with local anesthesia (with 3 patients having lateral approach) and general anesthesia in treating FBSS patients. Although it is a very minimally invasive surgery, FESS still requires precise manipulation, careful identification, and gentle dissection of anatomical structures to avoid damaging essential nerve structures in the fibrous adhesion of the old surgical site. Thanks to mastering the technique, the ratio of patients having their nerves released from compressive factors brings relatively positive results. It is equivalent to another report by authors Ahn et al. [3] and McGrath et al. [6]. To supplement the above comments, we present a case (Figure 2) of the exiting L5 nerve root being compressed by a hypertrophic superior articular process in the left L5–S1 foramen in a 74-year-old female patient with a history of cardiovascular disease, diabetes, and 3 previous spinal surgeries. The surgeon used a 10-mm operating tube through the contralateral interlaminar approach to expand the suitable interlaminar space then completely isolating and removing the left superior articular process tip from the L5 nerve root (Figure 5). The surgery gave excellent results, but a more significant number of patients and a more extended follow-up period are needed to provide long-term results.
Endoscopic operations have been shown to provide high levels of patient satisfaction, with many studies reporting significant improvements in pain and disability. For instance, the research of Kim et al. [9] demonstrated good clinical outcomes with an 80% reduction in pain. Similarly, the study of Cao et al. [10] showed that 11 patients who underwent interlaminar endoscopic decompression experienced significantly improved sciatica pain and ODI scores postoperation. In a study of 65 elderly patients with comorbidities, health-related quality of life improved after endoscopic surgery, even though they still experienced back pain [11]. While all our patients still experienced nonstatistically significant low back pain, 75% reported a good or excellent clinical outcome. These findings are consistent with other studies that have shown the alleviation of pain and disability among patients ranging from 16 to 86 years of age. Overall, these studies suggest that endoscopic surgery is an effective and safe option for patients looking to improve their quality of life by reducing pain and disability [3,4,12].
In addition to the group of patients with FBSS, we also encountered patients with adjacent segmental disease causing narrowed foraminal, narrowed lateral recess, or even spinal canal stenosis. None of the 10 patients with adjacent segmental disease who had FESS needed fusion surgery during the follow-up period. We are referring to performing fusion in the adjacent segment because it is due to subsequent spinal degeneration causing nerve compression, even accompanied by spinal instability and global spinal imbalance. Therefore, evaluated preoperative inaccuracies about instability may lead to failure and cause the patient to need fusion surgery to the adjacent segments (even after endoscopic decompression surgery). When the patient shows no or very little back pain, accompanied by signs of disc height loss, many bony spurs around the disc or joint detected on CT, are signs of the stable condition of the adjacent disc level. However, determining the stability of the degenerative spine in adults is still controversial, with no genuinely accurate and precise standards yet [13]. Therefore, more future research is needed on the issue of determining the stability and instability of the spine based on clinical and imaging criteria to select appropriate patients to carry out immediate spinal stabilization instead of simple endoscopic decompression—potential risk of instability later [6].
Thus, endoscopic surgery is an effective approach to accessing fibrosis scar tissue in patients with FBSS. It plays a crucial role in treating this condition. This surgical technique allows for direct and clear visualization of compromised nerve roots. Endoscopic dissectors and radiofrequency cautery can be used to remove most of the scar tissue. This results in decompression of the nerve and resolution of pain, motor, and sensory dysfunction without causing spinal instability.
The patient group in our study was small in number and heterogeneous. The patient's previous surgery included many types: endoscopy, microsurgery, open decompression surgery, spinal fixation, and cement injection. Therefore, the study results have many confounding factors. In addition, this is a retrospective study, so there needs to be more data from the control group for comparison. We realize there is a need for more studies with a standard design, randomized controlled, to evaluate the results and effectiveness of this method. However, the obtained results also demonstrate the feasibility of uniportal endoscopic spine surgery in treating FBSS as an alternative to major surgery.