INTRODUCTION
Minimally invasive spine surgery is a well-established concept in the management of lumbar disc herniation. Tubular micro-discectomy [9] and micro-endoscopic discectomy [3] are techniques where discectomy is performed through tubular ports with the aid of a microscope or an endoscope respectively. While 16 mm and 18 mm diameter tubular retractors are the most frequently and popularly utilized ports, there is no published literature on the use of 14 mm tubular retractor in the management of lumbar disc herniation. In the study the authors discuss the feasibility and outcomes of discectomy performed through a 14 mm tubular retractor and compare the outcomes with cases performed through 16 mm and 18 mm tubular retractors.
MATERIALS AND METHODS
1. Patients
This was a retrospective study of a prospectively collected data. Institutional review board approval was taken. The data of all patients who underwent tubular discectomy from July 2007 to April 2018 were analysed. The senior author initiated tubular discectomies with 18 mm tubular retractor in July 2007 and then evolved to 16 mm in October 2011. Use of 14 mm tube commenced from September 2017. The first 40 patients operated using 18 mm, 16 mm and 14 mm tube were included in the study and divided into three groups: Group A, Group B and Group C respectively (Table 1). The indication was lower limb radicular pain with MRI evidence of herniated nucleus pulposus and failure of conservative treatment of at least 6-weeks duration. Exclusion criteria was co-existing instability. The MRI films were reviewed to determine the level, size and location of the herniated fragments. Intra-operatively, the estimated blood loss, size of the incision, technical challenges and complications confronted were noted. VAS (Visual Analogue Scale) for leg pain, ODI (Oswestry Disability Index) and MacNab criteria were evaluated as outcome measures. Patients were followed up at intervals of 1 week, 6 weeks, 3 months, 6 months and 1 year.
RESULTS
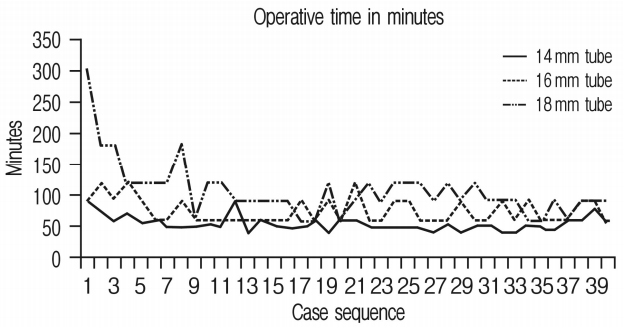
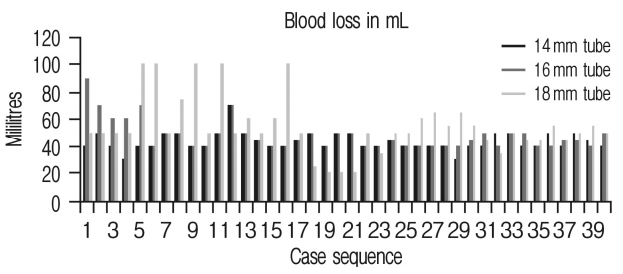
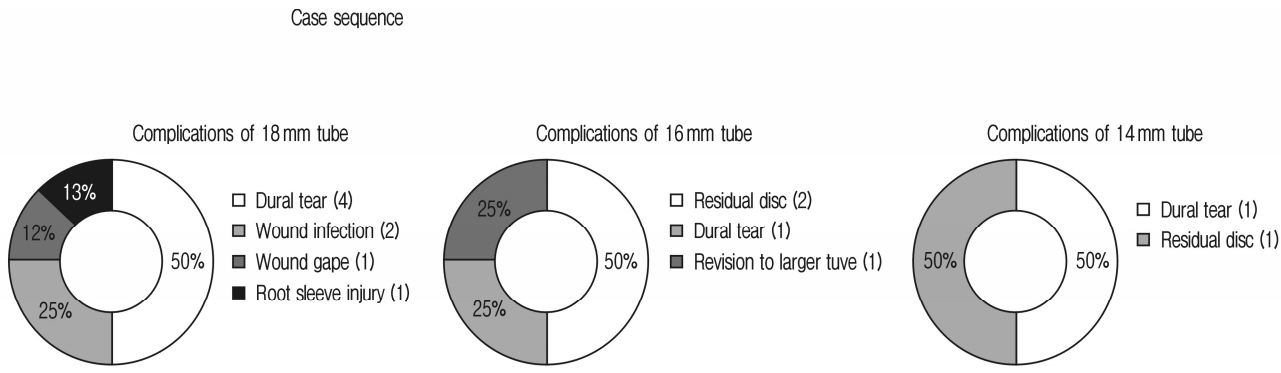
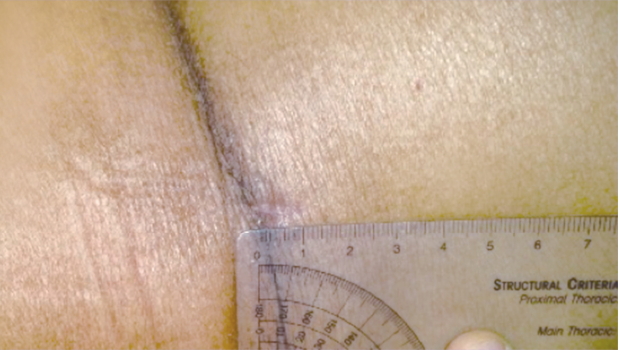
The age, pre-operative VAS and ODI were comparable in all three groups of patients. However, the difference in the postoperative outcomes was statistically significant between the three groups. The improvement in VAS and ODI were statistically significant in all the three groups. The operative time and blood loss in Groups A, B and C were 106.9±44.9, 74±19.45 and 53.37±12.26 min and 54.75±21.11 mL, 47.5±11.03 mL and 43.75±6.86 mL respectively. As experience grew, there was a proportionate decrease in the mean operative time and blood loss with decreasing diameters of the tube. The operative time and the blood loss reached a plateau after the 17th case (Table 2) (Figs. 1, 2, 3). The complication rate was also less in the 14 mm group. In Group A, dural tear was the most common complication, occurring in 4 out of 40 patients, followed by wound related problems. In Group B and C, a residual disc was the commonest complication, requiring revision surgery. Also, one patient in both Groups B and C, required conversion to a larger tube intra-operatively (Fig. 3). Dural tear was reported in one patient each in Groups B and C. Evaluation based on MacNab criteria showed ‘excellent’ surgical outcome in 36 patients and ‘good’ surgical outcome in 4 patients respectively in Group A, ‘excellent’ outcome in 37 patients and ‘good’ outcome in 3 patients in Group B, ‘excellent’ outcome in 38 patients and ‘good’ outcome in 2 patients in Group C. The 4 patients in Group A that did not have an ‘excellent’ surgical outcome were those with dural tears. The 2 patients in Group B and 1 patient in Group C who had only a ‘good’ outcome were cases of residual disc herniation.
DISCUSSION
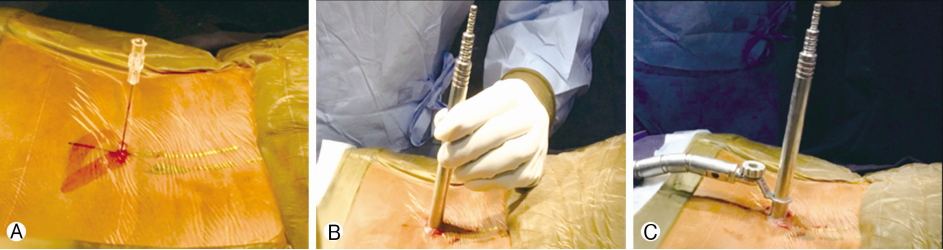
Tubular retractor system is being increasingly employed for decompression of spinal pathologies [10]. Lumbar disc herniations are usually excised through 16 and 18 mm diameter tubular retractors world-wide. The benefits include minimal muscle damage, negligible blood loss, short hospital stay, minimal post-operative back pain and discomfort, better cosmesis and faster recovery [2,4,6-8,11]. With increasing experience of dealing with complex pathologies utilizing the tubular retractors, the authors envisaged to incorporate 14 mm diameter tubular retractor to perform lumbar discectomies. The feasibility and outcomes of using a 14 mm tube have not been addressed in the literature. The improvement in the VAS, ODI as well as the surgical outcomes according to MacNab’s criteria in this series justifies the feasibility of 14 mm tube based approach in performing lumbar tubular micro-discectomies. It is worthwhile to note that as the diameter of the tube decreases, the corridor available to work also exponentially decreases (Table 3). Where the working area in the 18 mm and 16 mm tubes is 254 mm2 and 201 mm2 respectively, the working area in 14 mm tube is only 154 mm2 which is about 40% less than 18 mm tube and 23% less as compared to 16 mm tube. The improvement in ODI and VAS scores being better in Group C than in Group A and B may be due to the fact that the author is proficient with the use of the tubular retractor system. The author’s experience with 16 and 18 mm tubular retractors for more than a decade served as a learning ground to acquire skills to accomplish the goals of surgery through the narrow corridors of the 14 mm diameter tube. For the beginners, initial training in larger diameter tubes may be pertinent. Confidence gained in identifying structures and surgical skills acquired by operating through larger tubular retractors will lay the foundation for the use of 14 mm tube. The power drill (burr) used in the procedure has a cross-sectional area of 28.27 sq-mm (Aesculap) and the commonly used suction tips of 3 mm and 4 mm have cross-sectional areas of 7.06 sq-mm and 12.56 sq-mm, respectively. Technically, the insertion and employment of the above mentioned necessary instruments, rongeurs and especially the bipolar cautery through narrow corridors is extremely challenging. In particular, it is difficult to visualise the anatomy and use the suction tips as well as the ronguers at the same time. The suggestion to overcome this challenge is to use thinner suction tips and slender bipolar cautery forceps. Another critical point with the use of 14 mm tube is precise targeting of the location of the pathology. Since the tube is extremely narrow, any miscalculation with localisation can be unforgiving. A thorough pre-operative planning based on the radiographs as well as the MRI films to localise the site of the herniation guides in docking the tubular retractor at the right spot. This is applicable when one is dealing with caudal and cranially migrated disc herniation, as well as extra-foraminal herniation. However, in spite of some initial difficulties in the first few cases, we surmounted the initial learning curve of the 14 mm tube and were able to accomplish the objective in all cases. Only one patient did not improve favourably, probably secondary to a residual fragment left behind. Re-operation using a 16 mm tube after a week relieved the pain. However, the issue was unrelated to the size of the tubular retractor, the 16 mm tube being used more as a safeguard. In the context of comparison of the techniques, if the same degree of decompression and symptom relief can be achieved with lesser tissue trauma and morbidity, then the technique which is most minimally invasive would qualify to be adopted [1,5]. In view of this, the use of 14 mm tubular retractor in skilled hands is justified (Figs. 4, 5). However, there are certain limitations of the study. The results described at 1 year are relatively short and may require a long term follow-up. Secondly, since it is a retrospective study, there is a potential for selection bias. Lastly, the experiences are of a single surgeon and cannot be extrapolated to every surgeon.