AbstractTo describe a technique for reduction of spondyloptosis with minimal access surgery. A 40-year-old female with BMI of 31.29 presented with chronic back pain and claudicant right L5 dermatomal pain (VAS 9/10) and paresthesia. Radiographs of lumbosacral spine revealed spondyloptosis at L5-S1 with a slip angle of 38° and lumbar lordosis of 100°. Minimally invasive TLIF (MIS-TLIF) using tubular retractor and percutaneous pedicle screw-rod system was planned. MIS-TLIF was successful in achieving reduction and fusion of spondyloptosis. At 12 months follow up, the VAS for back pain improved from 9/10 to 2/10 and leg pain improved from 9/10 to 1/10. The ODI improved from 80% to 19%. Lumbar lordosis improved from 100° to 60° and slip angle 38° to 60°. There was no wound site morbidity and minimal operative site pain. Radiographs at 6 months revealed no loss of reduction or loosening of implants. Minimal access reduction and fusion technique (MIS-TLIF) using cantilever mechanism is feasible, safe and clinically effective in spondyloptosis.
INTRODUCTIONReduction of spondyloptosis is technically demanding and is associated with surgical morbidity and post-operative complications [1]. In the wake of increasing interest in minimally invasive fusions (MIS-TLIFs), question arises if the indications can extend to spondyloptosis. The main objective of this technical case report is to describe a cantilever reduction technique and fusion of spondyloptosis with minimal access (MIS-TLIF).
CASE REPORTA 40-year-old female with BMI of 31.29 presented with chronic back pain (VAS 9/10) and claudicant right lower limb L5 dermatomal pain (VAS 9/10) and paraesthesia. Radiographs revealed L5-S1 spondyloptosis (Fig. 1) with a slip angle of 38° and 100° of lumbar lordosis [2]. MIS-TLIF using tubular retractor and percutaneous pedicle screws was planned.
1. Operative ProcedureThree-dimensional navigation (Isocentric C-arm Arcadis, Siemens and S7 Medtronics Stealth) was utilized for the procedure. A 2.5 cm paramedian incision was taken bilaterally (Fig. 2). After bilateral placement of guide wires at L5 and S1, a non-expandable 22 mmX7 cm tubular retractor (Medtronics) was docked from the right side over L5-S1 facet joint complex using the Wiltse approach. Using the operating microscope (Pentero 900), the ipsilateral facet joint, pars and lamina were exposed. Using high power burr and Kerrison’s rongeurs, the superior facet of S1 above the pedicle and inferior articular process of L5 were removed. The lamina and pars interarticularis were excised. All bony fragments were used as autograft. The window of opportunity to perform TLIF, i.e. the L5-S1 disc lay bare between the exiting L5 and traversing S1 nerve roots. A 6 mm osteotome was hammered into the disc space and S1 dome osteotomy was performed. Cage size was confirmed with trials and a 12 X24 mm size titanium cage filled with bone-graft was pushed into the disc space. The cage helped in disc space distraction and acted as a fulcrum for the cantilever forces in reduction. Pedicle screws with SoleraⓇ (Medtronics, Memphis, USA) reduction tower assembly were inserted bi-laterally, cannulated over the guide-wires. Pre-contoured lordotic rod was introduced and confirmed under fluoroscopy. Both reduction towers were held firmly and screw caps were applied. Reduction was achieved by tightening the screw in the reduction assembly with interbody cage acting as lever arm over which slipped vertebra moved. This maneuver was applied simultaneously on both-sides and fluoroscopically confirmed. Screw caps were tightened first over the lower vertebra followed by the upper one to effect reduction of the slip. The blood loss was 150 mL and operating time was 3.5 hours. At 6-months follow-up (Fig. 3), the VAS for back and leg-pain improved from 9/10 to 2/10 and 9/10 to 1/10 respectively. The ODI improved from 80% to 19%, lordosis from 100°to 60° and slip- angle from 38° to 60°.
DISCUSSIONIn the context of reduction of spondyloptosis, almost every step of surgery starting from strategic positioning of the patient to achieving reduction are vital and challenging. While all the above steps are technically taxing with conventional open exposures, minimally invasive techniques make the situation even more intriguing and demanding.
There are several advantages of minimal access approach to tame spondyloptosis. The incision and exposure to access L5 and S1 pedicles in spondyloptosis is extensive and wide with open surgery (Fig. 4), and gets much larger in case of an obese patient. Percutaneous minimal access placement of pedicle screws circumvents this large exposure. Again, unlike in conventional open surgery, where extensive lateral exposure is required to obtain the perfect medial trajectory, in the context of MIS-TLIF, the most optimum entry point for percutaneous pedicle screw placement for the best possible trajectory can be chosen by the surgeon. The ability to gain excellent purchase in L5 body by inserting long, convergent, large diameter (7.5 mm) pedicle screws into L5 is vital for maneuverability and reduction of such extreme form of spondylolisthesis. The tubular retractor, once fixed in the trajectory of the L5-S1 (Fig 5) disc serves as a continuous guide to introduce various instruments like the chisel, shavers, curettes, cage trials as well as final placement of the cage filled with bone graft accurately. This step is important because it is not unusual to get disoriented and lose the sense of anatomy and direction in complex pathologies such as spondyloptosis.
While there have been a few successful reports of high-grade spondylolisthesis [3] managed with minimally invasive approaches, this is the first report of a case of spondyloptosis performed with MIS techniques.
NOTESConflicts of Interest Statement There is No conflict of interest among the authors or the institution regarding the manuscript, the scientific work or data collection. No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. There was no breach of ethical issues by any of the authors mentioned. The manuscript has been read and approved by the authors and each one of the authors treat their work trust worthy within all ethical parameters. NOTESEthical Review Committee statement Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research. Fig. 1.Lumbar lateral radiograph with slip angle (yellow line) 38° and lumbar lordosis angle (white line) 100°. The L5 vertebral body is more than 90% translated anteriorly in relation to the s1 vertebral segment. 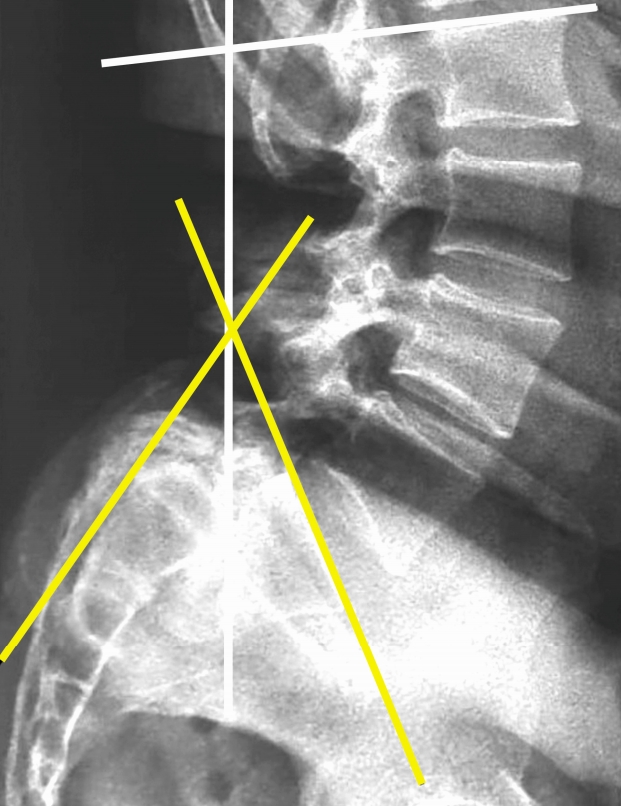
Fig. 3.Radiographs at 6 months revealed no loss of reduction or loosening of implants with lumbar lordosis (white line) improved from 100° to 60° and slip angle (yellow line) 38° to 60°. 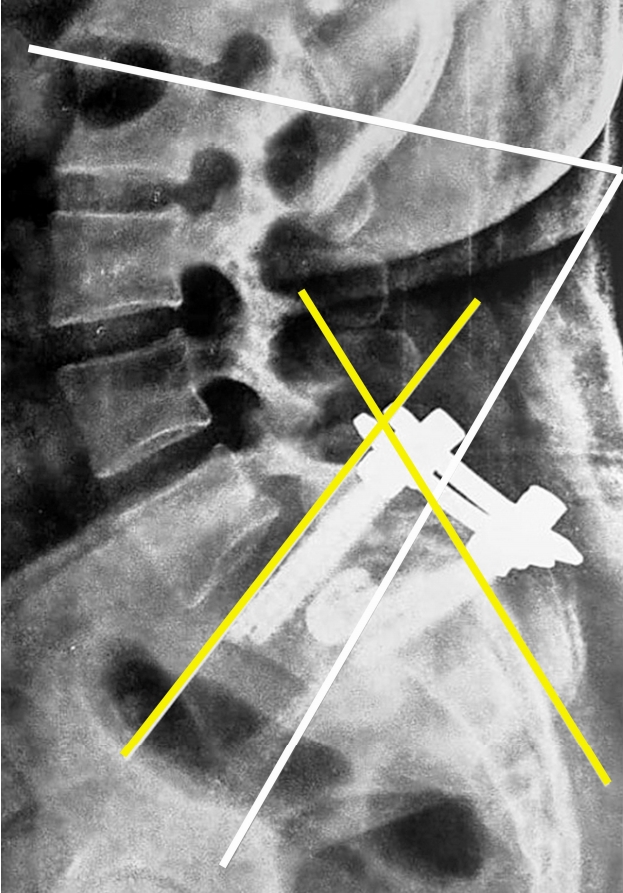
REFERENCES1. Lundine KM, Lewis SJ, Al-Aubaidi Z, Alman B, Howard AW: Patient outcomes in the operative and nonoperative management of high-grade spondylolisthesis in children. J Pediatr Orthop 34(5):483–489, 2014
|
|
|||||||||||||||||||||||||||||||||||||||