INTRODUCTION
Lumbar spinal stenosis is common lumbar degenerative diseases with narrowing of the spinal canal leads to radicular leg pain, back pain, and neurological intermittent claudication. Generally, the first treatment for symptomatic lumbar stenosis is conservative management including medication, physical therapy, and nerve-block procedures [1-4]. Hypertrophy of the articular process and yellow ligament and disc herniation are the main reasons for worsening of the clinical symptoms of lumbar stenosis. Nerve compression induced by these degenerative changes manifests as low back pain and radiculopathic leg pain, which worsens when standing or walking, and commonly referred to as neurogenic intermittent claudication [5,6]. Lumbar spinal stenosis can be classified into 3 different types, central spinal canal stenosis, lateral recess stenosis, and foraminal stenosis, according to the anatomically neural compression area [7]. Many middle-aged and elderly patients with lumbar and low back pain do not achieve satisfactory results with conservative treatment alone, resulting in decreased activity level and quality of life, eventually requiring spinal surgery. Lumbar spinal stenosis is the main indication for spinal surgery in patients over 65 years of age [8]. A variety of surgical techniques, including tubular and microsurgical decompression and fusion surgery, have been used for the treatment of spinal stenosis that does not achieve satisfactory improvement with long-term conservative treatment. The development of endoscopic spinal surgery technology has made it possible to decompress the lumbar nerve using a full endoscope. In particular, in the case of elderly patients who are at high risk of general anesthesia, surgery is possible without general anesthesia, there is little tissue damage, the hospital stay is short, and the cost is low, but the surgical results are similar or better [9]. Full endoscopic surgery for lumbar nerve decompression is largely divided into an interlaminar approach and a transforaminal approach, and these approaches select the most suitable method according to the type of central stenosis, lateral recess stenosis, and foraminal stenosis stenosis. The interlaminar endoscopic technique is similar to microscopic and tubular decompression surgery, meaning the anatomic orientation is familiar and similar in both techniques. Full-endoscopic interlaminar decompression shows that all the procedures of open decompression can be completely substituted by endoscopic management.
Transforaminal endoscopic techniques have been reported to be successful in disc surgery and unilateral foraminal stenosis, but there are anatomic limitations for symptomatic bilateral recess stenosis. This technique is more useful in foraminal stenosis and lateral recess stenosis rather than central spinal stenosis These limitations, especially at the level of L5-S1, are a high iliac crest, a large L5 transverse process, a large facet joint, and a narrowed disc space [10,11]. With advances in endoscopic spinal surgery methods and instruments, earlier contraindications have become indications for full-endoscopic spinal decompression in the treatment of lumbar degenerative diseases.
There are some reports about complications and contraindications of full endoscopic lumbar decompression. Among them, Incidental durotomy is the most common complication [12-14].
Sairyo et al. [15] reported complications which included dural tear, postoperative hematoma, neural complication and inferior articular process fracture .
MATERIALS AND METHODS
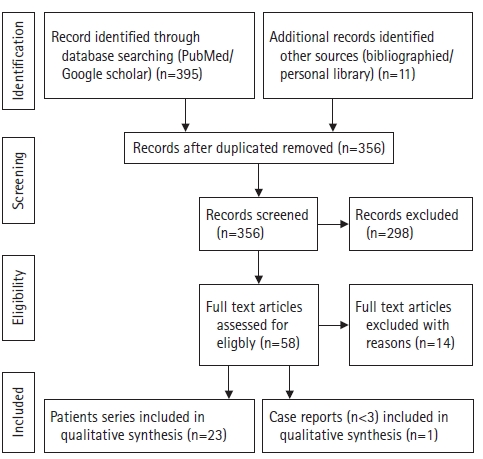
We used the Preferred Reporting Items for Systematic Review as a template for our systematic review. The review process started with a search of PubMed databases to identify articles on full endoscopic lumbar decompression. An independent reviewers assessed all articles and references and agreed on which articles should be included. To prevent selection bias during review, abstracts from the search were numbered and pasted into a document after deleting the publication journal, author, and institution. We used the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines as a template for our systematic review. These guidelines are an evidence-based minimum set of items aimed to help authors improve the reporting of systematic reviews and meta-analyses. The review process started with a search of PubMed and cochrane databases to identify articles on spinal stenosis and endoscopic decompression protocol. A reviewer assessed all articles and references and agreed on which articles should be included. To prevent selection bias during review, abstracts from the search were numbered and pasted into a document after deleting the publication journal, author, and institution. The initial search included keywords “spinal stenosis” and “endoscopic decompression” which returned 406 results.
Due to the high variation of relevant articles and anatomical locations, the search was modified to included “lumbar,” which produced 356 results after duplicate articles were identified and discarded. The search also included the exact surgical technique term “interlamiar” and returned 58 results published from 1980 to 2011. Exclusion criteria included no complication results reported (10 articles), microendoscopic surgery (10 articles), endoscopic interbody fusion (3 articles), spondylolisthesis (2 articles). Metastasis (1 articles), biportal surgery (7 articles) and studies not in English (1 articles). A total of 24 articles meeting our criteria were identified through the search process. Thus, 24 articles met the criteria and were analyzed (Figure 1).
RESULTS
Comprehensively, the contraindication of full endoscopic lumbar interlaminar decompression is Spondylolisthesis, Instability, previous surgery, foraminal stenosis, tumor, infection, scoliosis, main back pain, calcified disc herniation, medical problem, cauda equine syndrome, severe stenosis, trauma, and painless weakness were reported in the following order (Table 1).
Complications of full endoscopic interlaminar decompression were reported in the following order, dural tearing is the most common, epidural hematoma is the 2nd common, In addition to these two most common complications, various complications occur frequently in the following order. transient dysesthesia, urinary retention, motor weakness, cauda equine syndrome, wound infection, disc herniation, persistent pain, medical problem, Inferior articular process fracture, incomplete decompression, and instability (Table 2).
DISCUSSION
Full Endoscopic Interlamiar Lumbar Decompression
Many authors reported the exclusion criteria of full endoscopic interlaminar lumbar decompression. In 2011, Komp et al. [16] reported prospective study of bilateral decompression of lumbar degenerative central spinal stenosis by full-endoscopic interlaminar technique with unilateral approach (level 2 of evidence). In this study, The following cases were excluded from the indication, predominant back pain, foraminal stenosis, in the lower level, disc herniation, degenerative spondylolisthesis more than meyerding Grade I, multidirectional rotation slide, Scoliosis more than 20 degrees, prior surgery in the same segment, cauda equina syndrome. Also, in this study, several complications were reported, 5 times transient postoperative dysesthesia, 2 times transient urinary retention, 2 times dura injuries, 1 time increase in preoperatively-existing foot dorsiflexion paresis. Apart from transient dysesthesia and transient urinary retention, the complication rate was 3.3%. Two patients (2.7%) required revision surgery with additional fusion owing to persistent leg pain and/or progradiant back pain.
In 2013, Ruetten et al. [17] reported prospective randomized controlled study of decompression of lumbar lateral spinal stenosis by full-endoscopic, interlaminar technique (level 1 of evidence), in this study, the contraindications of this surgery were pure back pain, instability, deformity requiring correction, foraminal stenosis.
In 2015, Komp et al. [18] reported a prospective, randomized, controlled study of bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique (level 1 of evidence). In this study, Exclusion criteria were predominant back pain, foraminal stenosis in the lower level, fresh soft disc herniations with bony stenosis, degenerative spondylolisthesis more than Meyerding Grade I, multidirectional rotation slide, scoliosis more than 20°, prior surgery in the same segment, and cauda equina syndrome. Also, in this study, the following complications occurred: transient postoperative dysesthesia, transient urinary retention and dura injuries. There were foot dorsiflexion paresis, epidural hematoma, delayed wound healing and soft-tissue infections. There were no other complications such as spondylodiscitis, cauda equina syndrome, or thrombosis. Apart from transient dysesthesia and transient urinary retention, the complication rate was 5% and was significantly higher in the Microscopic surgery group [18].
In 2017, Kamson et al. [19] reported the retrospective review of prospective study of full-endoscopic assisted lumbar decompressive surgery performed in an outpatient, ambulatory facility (level 3 of evidence). In this study, there were 3 major and 3 minor postoperative complications. The 3 major complications were all incidences of early postoperative reherniation that resulted in reoperation. The minor complications included 2 cases of sympathetically mediated pain syndrome and one case of transient urinary retention.
In 2017, Hwang et al. [20] reported cases series of contralateral Interlaminar keyhole Percutaneous Endoscopic Lumbar Surgery (level 4 of evidence), an epidural hematoma was reported as complication after endoscopic decompression.
In 2018, Lee et al. [21] reported retrospective study of percutaneous endoscopic laminotomy with flavectomy by uniportal, unilateral approach for the lumbar canal or lateral recess stenosis (level 3 of evidence). In this study, the following cases were excluded from the indication, segmental instability and degenerative spondylolisthesis more than Meyerding grade I, multidirectional rotation slide, scoliosis >20° combined foraminal stenosis in the same or lower level, or coexisting pathologic conditions such as acute inflammation, infection, or tumor. Also, they reported complications of postoperative transient dysesthesia, lower extremity motor weakness, dural tearing, recurrent disc.
Kim et al. [22] reported early outcomes of endoscopic contralateral foraminal and lateral recess decompression via an interlaminar approach by retrospective study (level 3 of evidence), they experienced the complication of inadequate foraminal decompression.
Also, Kim et al. [23] reported retrospective study of percutaneous full endoscopic bilateral lumbar decompression of spinal stenosis through uniportal-contralateral approach (level 3 of evidence). In this study, the following cases were excluded from the indication, patients with spondylolisthesis grade II or greater, patients who demonstrated frank segmental instability in dynamic radiographs, patients who were inoperable due to other medical problems and patients with complaints of claudication pain due to vascular stenosis. Also, they reported complications of dural tear occurred in 3 cases (6.25%). Of these 3 cases, one case (2.1%) was converted to open decompression because of complaints of severe back pain and leg pain, and 2 cases (4.17%) who had Macnab fair and poor grades, respectively, required transforaminal lumbar interbody fusion after this procedure. Postoperative magnetic resonance imaging revealed adequate decompression in all cases.
Lee et al. [24] reported a meta-analysis of full-endoscopic decompression via interlaminar approach for central or lateral recess spinal stenosis (level 3 of evidence). In this study, they reported complications of revision surgery, transient paresthesia, incidental durotomy, epidural hematoma, headache, and infection.
In 2019, Park and Lee [25] reported a retrospecitive study on full-endoscopic interlaminar decompression (level 3 of evidence). In this study, patients with nonspecific symptoms, lateral recess or foraminal stenosis, spondylolisthesis, previous back surgery, or contraindication to surgery due to bleeding tendency were excluded. However, no serious complications such as epidural hemorrhage, dural or nerve damage or infection were reported.
Li et al. [26] reported comparative study about full endoscopic decompression via a transforaminal approach and an interlaminar approach for lateral recess stenosis (level 2 of evidence), in the interlaminar approach, the complication rate was 3.4% of transient dysthesia.
Lim et al. [27] reported retrospectively comparative study of endoscopic decompression surgery by using 1 port for multiple lumbar spinal canal stenosis (level 3 of evidence), they reported dura tearing, epidural hematoma, wound infection, and reoperation due to incomplete decompression as complications.
Lv et al. [28] reported prospective controlled study of comparison effect of PELD and fenestration in geriatric lumbar lateral stenosis (level 2 of evidence), in this study, the following cases were excluded from the indication, lumbar instability in dynamic radiographs: translation greater than 3 mm or changes in angulation greater than 10° at 1 motion segment on the lateral flexion and extension, pathological conditions such as lumbar infection, tumor or fracture, a history of previous lumbar surgery. Also, they reported dura tearing and postoperative delirium as complication.
Lee et al. [29] reported retrospective study of endoscopic decompression in lumbar central and lateral recess stenosis (level 3 of evidence), they excluded Patients with documented diagnoses of segmental instability, degenerative spondylolisthesis greater than Meyerding grade I, scoliosis of more than 20 degrees, combined foraminal stenosis in the same or lower level, or coexisting pathologic conditions, such as acute inflammation, infection, or the known presence of tumors. Dura tearing, motor weakness, dysethesia, postoperative hematoma, excessive facet resection were reported as complication.
Cao et al. [30] reported retrospective study of the “Tube in tube” interlaminar endoscopic decompression for lumbar spinal stenosis (level 3 of evidence), in this study, postoperative radiating pain due to nerve root disturbance or inflammatory stimulation, cauda equina symptom, Spinal cord hypertension were reported as complications.
McGrath et al. [31] reported retrospective comparative study of unilateral laminotomy for bilateral lumbar decompression (level 3 of evidence), disc herniation and paresthesia were as complication of endoscopic surgery.
Huang et al. [32] reported retrospective study of full endoscopic uniportal unilateral laminotomy, in this study (level 3 of evidence), the exclusion criteria of indication were distinct instability in dynamic radiographs, spondylolisthesis grade III or greater according to the Meyerding criteria, foraminal stenosis with root neuropathy, symptomatic spondylolytic spondylolisthesis, stenosis merely caused by disc herniation, lesions induced by malignancy or infection. Postoperatively, residual claudication and back pain, back pain and sciatica due to recurrent stenosis from the hypertrophic facet joint, incomplete decompression, iatrogenic durotomy, delayed wound healing needing debridement were reported as complications.
Hua et al. [33] reported retrospective comparative study of comparison of endoscopic unilateral laminotomy bilateral decompression and TLIF (level 3 of evidence). In this study, they excluded patients with degenerative spondylolisthesis or deformity, tumors, infections, or other lesions, also they excluded a surgical history involving the corresponding segment. Intraoperative complication rate was 9.4% with dura rearing and cauda equina injury.
Chiu et al. [34] reported retrospective comparative study of endoscopic vs open laminectomy (level 3 of evidence) and they reviewed papers of endoscopic lumbar decompression and dural tearing, urinary retension, infection, motor weakness were complications.
Yang et al. [35] reported retrospective comparative study of endoscopic vs microscopic unilateral laminotomy bilateral decompression (level 3 of evidence), the following cases were excluded from the indication, isthmic spondylolisthesis or dynamic instability on the flexion/extension radiographs, pathological spinal diseases, such as infection, tumor, or previous spinal surgery. Also, in endoscopic group, dura tearing, urinary retention, acute exacerbation of chronic bronchitis, acute left heart failure were reported as complications.
Cheung et al. [9] reported economic and decision analysis of cost analysis between endoscopic and microscopic interlaminar decompression (level 2 of evidence), in this study, they reported dural tear, iatrogenic instability requiring fusion as complications of MIS.
Lim et al. [36] reported retrospective study of full endoscopic interlaminar inside-out unilateral laminotomy bilateral decompression (level 3 of evidence), in this study, the following cases were excluded from the indication, foraminal stenosis, multiple level stenosis, significant instability, those with a history of previous lumbar surgery, and those with degenerative spondylolisthesis grade 2 and above were excluded. On the other hand, Incidental dural tear, epidural hematoma, reoperation were reported as postoperative complications.
Ruetten and Komp [37] reported systemic review of endoscopic lumbar decompression (level 3 of evidence), in this study, contraindications are back pain as a main symptom, instability/deformities with an indication for a stabilizing procedure. Intraoperative complications were reported such as surgery on the wrong segment, epidural bleeding, insufficient decompression, injuries to the dura, injuries to neural structures, injuries to vessels, injuries to organs. Direct postoperative complications were persistent or progressive radicular symptoms, cauda equina syndrome, urinary retention, consequences of injury to vessels or organs. Delayed postoperative complications: soft tissue infection, spondylodiscitis, cerebrospinal fluid fistula, delayed consequences of injury to vessels or organs, further radicular symptoms, surgically induced symptoms (failed back surgery syndrome).
Zhao et al. [38] reported retrospective study of percutaneous endoscopic unilateral laminotomy and bilateral decompression for lumbar spinal stenosis (level 3 of evidence), in this study, exclusion criteria is as following as patients with lumbar instability and symptoms of lower back pain, LSS with Meyerding Grade II spondylolisthesis, multisegment stenosis with a history of lumbar surgery, infection, tumor or trauma, lower extremity neuropathy, or mental disorders.
CONCLUSION
According to literature analysis, the interlaminar approach is effective for central spinal stenosis and lateral recess stenosis, whereas the transforaminal approach is preferred for foraminal stenosis and lateral recess stenosis. Contraindication in both methods has many things in common, but the interalminar approach is preferred in cases of multiple sites, bilateral symptoms, or high iliac crest. In the interlaminar approach, dural tearing and epidural hematoma are the most common, whereas in the transforaminal approach, dysesthesia and untreated pain are relatively common. Additionally, various complications such as transient dysesthesia, urinary retention, motor weakness, cauda equine syndrome, wound infection may occur.